Dextromethorphan
Dextromethorphan (DXM or DM) is a medication most often used as a cough suppressant in over-the-counter cold and cough medicines. It is sold in syrup, tablet, spray, and lozenge forms.
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Robitussin, Delsym, DM, DexAlone, Duract, others |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682492 |
| Pregnancy category | |
| Routes of administration | By mouth |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | 11%[1] |
| Metabolism | Hepatic (liver) enzymes: major CYP2D6, minor CYP3A4, and minor CYP3A5 |
| Elimination half-life | 2–4 hours (extensive metabolizers); 24 hours (poor metabolizers)[2] |
| Excretion | Renal |
| Identifiers | |
IUPAC name
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.004.321 |
| Chemical and physical data | |
| Formula | C18H25NO |
| Molar mass | 271.40 g/mol g·mol−1 |
| 3D model (JSmol) | |
| Melting point | 111 °C (232 °F) |
SMILES
| |
InChI
| |
| | |
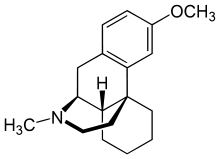
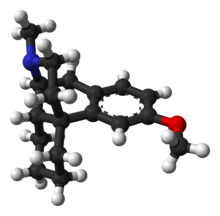
It is in the morphinan class of medications with sedative, dissociative, and stimulant properties (at lower doses). In its pure form, dextromethorphan occurs as a white powder.[3]
DXM is also used recreationally. When exceeding approved dosages, dextromethorphan acts as a dissociative hallucinogen. It has multiple mechanisms of action, including actions as a nonselective serotonin reuptake inhibitor[4] and a sigma-1 receptor agonist.[5][6] DXM and its major metabolite, dextrorphan, also act as an NMDA receptor antagonist at high doses, which produces effects similar to, yet distinct from, the dissociative states created by other dissociative anesthetics such as ketamine, nitrous oxide, and phencyclidine.
It was patented in 1949 and approved for medical use in 1953.[7]
Medical uses

Cough suppression
The primary use of dextromethorphan is as a cough suppressant, for the temporary relief of cough caused by minor throat and bronchial irritation (such as commonly accompanies the flu and common cold), as well as those resulting from inhaled particle irritants.[8] However, controlled studies have found the symptomatic effectiveness of dextromethorphan similar to placebo.[9]
Neuropsychiatric disorders
In 2010, the FDA approved the combination drug dextromethorphan/quinidine for the treatment of pseudobulbar affect (uncontrollable laughing/crying). Dextromethorphan is the actual therapeutic agent in the combination; quinidine merely serves to inhibit the enzymatic degradation of dextromethorphan and thereby increase its circulating concentrations via inhibition of CYP2D6.[10]
In 2013, a randomized clinical trial was conducted at Tabriz University of Medical Sciences in Tabriz, Iran, that indicated dextromethorphan may help reduce the overall discomfort and duration of withdrawal symptoms associated with opioid use disorder. When combined with clonidine, dextromethorphan reduced the overall time needed for withdrawal symptoms to peak by 24 hours while also reducing the severity of the symptoms compared to Clonidine alone.[11]
In 2016, the ASA released a promising study with the combination of dextromethorphan with pregabalin, acetaminophen, and naproxen which showed a decrease in postoperative pain intensity (preemptive analgesia).[12]
Contraindications
Because dextromethorphan can trigger a histamine release (allergic reaction), atopic children, who are especially susceptible to allergic reactions, should be administered dextromethorphan only if absolutely necessary, and only under the strict supervision of a healthcare professional.[13]
Adverse effects
Side effects of dextromethorphan at normal therapeutic doses can include:[2][8][13]
A rare side effect is respiratory depression.[8]
Neurotoxicity
Dextromethorphan had been thought to cause Olney's lesions when administered intravenously; however, this was later proven inconclusive, due to lack of research on humans. Tests were performed on rats, giving them 50 mg or more every day for as long as a month. Neurotoxic changes, including vacuolation, have been observed in posterior cingulate and retrosplenial cortices of rats administered other NMDA receptor antagonists such as PCP, but not with dextromethorphan.[14][15]
Dependence and withdrawal
In many documented cases, dextromethorphan has produced psychological dependence in people who used it recreationally. However, it does not produce physical addiction, according to the WHO Committee on Drug Dependence.[16] It is considered less addictive than the other common weak opiate cough suppressant, codeine.[2] Since dextromethorphan also acts as a serotonin reuptake inhibitor, users describe that regular recreational use over a long period of time can cause withdrawal symptoms similar to those of antidepressant discontinuation syndrome. Additionally, disturbances have been reported in sleep, senses, movement, mood, and thinking.
Overdose
Adverse effects of dextromethorphan in overdose at doses 3 to 10 times the recommended therapeutic dose:[17]
- mild nausea
- restlessness
- insomnia
- talking fast
- dilated pupils
- glassy eyes
- dizziness
At doses 15 to 75 times the recommended therapeutic dose:[17][18]
- hallucinations
- dissociation
- vomiting
- delusions of grandeur
- blurred vision
- double vision
- bloodshot eyes
- dilated pupils
- sweating
- fever
- bruxia (teeth grinding)
- hypotension
- hypertension
- tachycardia
- shallow respiration
- diarrhea
- urinary retention
- muscle spasms
- sedation
- paresthesia
- hypomania
- slurred speech
- false positives on drug screens
- blackouts
- inability to focus eyes
- skin rash
- severe itchiness
- spontaneous memory recall
- acute psychosis
Episodic acute psychosis can occur with high doses of DXM taken for recreational use, and an abundance of psychiatric symptoms can result, including dissociation and other PCP-like symptoms.[19]
Interactions
Dextromethorphan should not be taken with monoamine oxidase inhibitors (MAOIs)[13] due to the potential for serotonin syndrome, which is a potentially life-threatening condition that can occur rapidly, due to a buildup of an excessive amount of serotonin in the body.
Caution should be exercised when taking dextromethorphan when drinking grapefruit juice or eating grapefruits, as compounds in grapefruit affect a number of drugs, including dextromethorphan, through the inhibition of the cytochrome p450 system in the liver, and can lead to excessive accumulation and prolonged effects. Grapefruit and grapefruit juices (especially white grapefruit juice, but also including other citrus fruits such as bergamot and lime, as well as a number of noncitrus fruits[20]) generally are recommended to be avoided while using dextromethorphan and numerous other medications.
Pharmacology
Pharmacodynamics
| Site | DXM | DXO | Species | Ref |
|---|---|---|---|---|
| NMDAR (MK-801) | 2,120–8,945 | 486–906 | Rat | [22] |
| σ1 | 142–652 | 118–481 | Rat | [22] |
| σ2 | 11,060–22,864 | 11,325–15,582 | Rat | [22] |
| MOR | 1,280 ND | 420 >1,000 | Rat Human | [22] [25] |
| DOR | 11,500 | 34,700 | Rat | [22] |
| KOR | 7,000 | 5,950 | Rat | [22] |
| SERT | 23–40 | 401–484 | Rat | [22] |
| NET | ≥240 | ≥340 | Rat | [22] |
| DAT | >1,000 | >1,000 | Rat | [22] |
| 5-HT1A | >1,000 | >1,000 | Rat | [22] |
| 5-HT1B/1D | 61% at 1 μM | 54% at 1 μM | Rat | [22] |
| 5-HT2A | >1,000 | >1,000 | Rat | [22] |
| α1 | >1,000 | >1,000 | Rat | [22] |
| α2 | 60% at 1 μM | >1,000 | Rat | [22] |
| β | >1,000 | 35% at 1 μM | Rat | [22] |
| D2 | >1,000 | >1,000 | Rat | [22] |
| H1 | >1,000 | 95% at 1 μM | Rat | [22] |
| mAChRs | >1,000 | 100% at 1 μM | Rat | [22] |
| nAChRs | 700–8,900 (IC50) | 1,300–29,600 (IC50) | Rat | [22] |
| VDSCs | >50,000 (IC50) | ND | Rat | [26][27] |
| Values are Ki (nM), unless otherwise noted. The smaller the value, the more strongly the drug binds to the site. | ||||
Dextromethorphan has been found to possess the following actions (<1 μM) using rat tissues:[22][28]
- Uncompetitive antagonist of the NMDA receptor via the MK-801/PCP site[28]
- Sigma σ1 receptor agonist
- μ-Opioid receptor agonist
- SERT and NET blocker (i.e., serotonin–norepinephrine reuptake inhibitor)
- Negative allosteric modulator of nicotinic acetylcholine receptors
- Ligand of the serotonin 5-HT1B/1D, histamine H1, α2-adrenergic, and muscarinic acetylcholine receptors
Rather than acting as a direct NMDA receptor antagonist itself, dextromethorphan acts as a prodrug of its much more potent metabolite dextrorphan, and this is the actual mediator of its dissociative effects.[29] What role, if any, (+)-3-methoxymorphinan, dextromethorphan's other major metabolite, plays in its effects is not entirely clear.[30]
Pharmacokinetics
Following oral administration, dextromethorphan is rapidly absorbed from the gastrointestinal tract, where it enters the bloodstream and crosses the blood–brain barrier.
At therapeutic doses, dextromethorphan acts centrally (meaning that it acts on the brain) as opposed to locally (on the respiratory tract). It elevates the threshold for coughing, without inhibiting ciliary activity. Dextromethorphan is rapidly absorbed from the gastrointestinal tract and converted into the active metabolite dextrorphan in the liver by the cytochrome P450 enzyme CYP2D6. The average dose necessary for effective antitussive therapy is between 10 and 45 mg, depending on the individual. The International Society for the Study of Cough recommends "an adequate first dose of medication is 60 mg in the adult and repeat dosing should be infrequent rather than the qds recommended."[31]
DXM has an elimination half-life of approximately 4 hours in individuals with an extensive metabolizer phenotype; this is increased to approximately 13 hours when DXM is given in combination with quinidine.[24] The duration of action after oral administration is about three to eight hours for dextromethorphan hydrobromide, and 10 to 12 hours for dextromethorphan polistirex. Around one in 10 of the Caucasian population has little or no CYP2D6 enzyme activity, leading to long-lived high drug levels.[31]
Metabolism
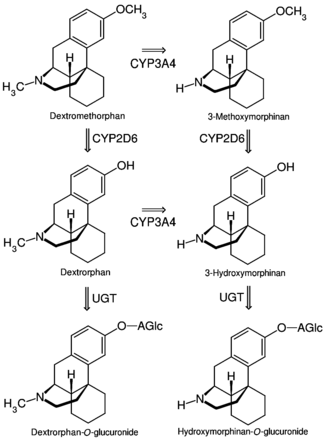
The first pass through the hepatic portal vein results in some of the drug being metabolized by O-demethylation into an active metabolite of dextromethorphan called dextrorphan (DXO). DXO is the 3-hydroxy derivative of dextromethorphan. The therapeutic activity of dextromethorphan is believed to be caused by both the drug and this metabolite. Dextromethorphan also undergoes N-demethylation (to 3-methoxymorphinan or MEM),[33] and partial conjugation with glucuronic acid and sulfate ions. Hours after dextromethorphan therapy, (in humans) the metabolites (+)-3-hydroxy-N-methylmorphinan, (+)-3-morphinan, and traces of the unchanged drug are detectable in the urine.[13]
A major metabolic catalyst involved is the cytochrome P450 enzyme known as 2D6, or CYP2D6. A significant portion of the population has a functional deficiency in this enzyme and are known as poor CYP2D6 metabolizers. O-demethylation of DXM to DXO contributes to at least 80% of the DXO formed during DXM metabolism.[33] As CYP2D6 is a major metabolic pathway in the inactivation of dextromethorphan, the duration of action and effects of dextromethorphan can be increased by as much as three times in such poor metabolizers.[34] In one study on 252 Americans, 84.3% were found to be "fast" (extensive) metabolizers, 6.8% to be "intermediate" metabolizers, and 8.8% were "slow" metabolizers of DXM.[35] A number of alleles for CYP2D6 are known, including several completely inactive variants. The distribution of alleles is uneven amongst ethnic groups.
A large number of medications are potent inhibitors of CYP2D6. Some types of medications known to inhibit CYP2D6 include certain SSRIs and tricyclic antidepressants, some antipsychotics, and the commonly available antihistamine diphenhydramine. Therefore, the potential of interactions exists between dextromethorphan and medications that inhibit this enzyme, particularly in slow metabolizers.
DXM is also metabolized by CYP3A4. N-demethylation is primarily accomplished by CYP3A4, contributing to at least 90% of the MEM formed as a primary metabolite of DXM.[33]
A number of other CYP enzymes are implicated as minor pathways of DXM metabolism. CYP2B6 is actually more effective than CYP3A4 at N-demethylation of DXM, but, since the average individual has a much lower CYP2B6 content in his/her liver relative to CYP3A4, most N-demethylation of DXM is catalyzed by CYP3A4.[33]
Chemistry
Dextromethorphan is the dextrorotatory enantiomer of levomethorphan, which is the methyl ether of levorphanol, both opioid analgesics. It is named according to IUPAC rules as (+)-3-methoxy-17-methyl-9α,13α,14α-morphinan. As its pure form, dextromethorphan occurs as an odorless, opalescent white powder. It is freely soluble in chloroform and insoluble in water; the hydrobromide salt is water-soluble up to 1.5 g/100 mL at 25 °C.[36] Dextromethorphan is commonly available as the monohydrated hydrobromide salt, however some newer extended-release formulations contain dextromethorphan bound to an ion-exchange resin based on polystyrene sulfonic acid. Dextromethorphan's specific rotation in water is +27.6° (20 °C, Sodium D-line).
History
The racemic parent compound racemorphan was first described in a Swiss and US patent application from Hoffmann-La Roche in 1946 and 1947, respectively; a patent was granted in 1950. A resolution of the two isomers of racemorphan with tartaric acid was published in 1952,[37] and DXM was successfully tested in 1954 as part of US Navy and CIA-funded research on nonaddictive substitutes for codeine.[38] DXM was approved by the FDA in 1958 as an over-the-counter antitussive.[37] As had been initially hoped, DXM was a solution for some of the problems associated with the use of codeine phosphate as a cough suppressant, such as sedation and opiate dependence, but like the dissociative anesthetics phencyclidine and ketamine, DXM later became associated with nonmedical use.[37][39]
During the 1960s and 1970s, dextromethorphan became available in an over-the-counter tablet form by the brand name Romilar. In 1973, Romilar was taken off the shelves after a burst in sales because of frequent misuse. A few years later, products with an unpleasant taste were introduced (such as Robitussin, Vicks-44, and Dextrotussion), but later the same manufacturers began producing products with a better taste.[39] The advent of widespread internet access in the 1990s allowed users to rapidly disseminate information about DXM, and online discussion groups formed around use and acquisition of the drug. As early as 1996, DXM HBr powder could be purchased in bulk from online retailers, allowing users to avoid consuming DXM in syrup preparations.[37] As of January 1, 2012, dextromethorphan is prohibited for sale to minors in the State of California and in the State of Oregon as of January 1, 2018, except with a doctor's prescription.[40] Several other states have also began regulating sales of dextromethorphan to minors.
In Indonesia, the National Agency of Drug and Food Control (BPOM-RI) prohibited single-component dextromethorphan drug sales with or without prescription. Indonesia is the only country in the world that makes single-component dextromethorphan illegal even by prescription[41] and violators may be prosecuted by law. National Anti-Narcotics Agency (BNN RI) has even threatened to revoke pharmacies' and drug stores' licenses if they still stock dextromethorphan, and will notify the police for criminal prosecution.[42] As a result of this regulation, 130 drugs have been withdrawn from the market, but drugs containing multicomponent dextromethorphan can be sold over the counter.[43] In its official press release, BPOM-RI also stated that dextromethorphan is often used as a substitute for marijuana, amphetamine, and heroin by drug abusers, and its use as an antitussive is less beneficial nowadays.[44]
Society and culture
Marketing
It may be used in generic labels and store brands, Benylin DM, Mucinex DM, Camydex-20 tablets, Robitussin, NyQuil, Dimetapp, Vicks, Coricidin, Delsym, TheraFlu, Charcoal D, Cinfatós and others. It has been used in counterfeit medications.[45]
Recreational use

Over-the-counter preparations containing dextromethorphan have been used in manners inconsistent with their labeling, often as a recreational drug.[39] At doses much higher than medically recommended, DXM and its major metabolite, dextrorphan, acts as an NMDA receptor antagonist, which produces dissociative hallucinogenic states somewhat similar to ketamine and phencyclidine.[46] Along with other drugs such as ketamine or phencyclidine, also known as PCP, there is a street name for dextromethorphan-infused substances which is also known as "Angel". It may produce distortions of the visual field – feelings of dissociation, distorted bodily perception, excitement, and a loss of sense of time. Some users report stimulant-like euphoria, particularly in response to music. Dextromethorphan usually provides its recreational effects in a non-linear fashion, so that they are experienced in significantly varied stages. These stages are commonly referred to as "plateaus". These plateaus are labeled between one and four, one being the lowest and so on. Each plateau is said to come with different related effects and experiences.[47] Teens tend to have a higher likelihood to use dextromethorphan-related drugs as they are easier to access, and an easier way to cope with psychiatric disorders.[48]
Research
Dextromethorphan/quinidine is also under investigation for the treatment of a variety of other neurological and neuropsychiatric conditions besides pseudobulbar affect, such as agitation associated with Alzheimer's disease and major depressive disorder.[10]
References
- Kukanich B, Papich MG (October 2004). "Plasma profile and pharmacokinetics of dextromethorphan after intravenous and oral administration in healthy dogs". Journal of Veterinary Pharmacology and Therapeutics. 27 (5): 337–41. doi:10.1111/j.1365-2885.2004.00608.x. PMID 15500572.
- "Balminil DM, Benylin DM (dextromethorphan) dosing, indications, interactions, adverse effects, and more". Medscape Reference. WebMD. Retrieved 15 April 2014.
- "Reference Tables: Description and Solubility - D". Archived from the original on 2017-07-04. Retrieved 2011-05-06.
- Schwartz AR, Pizon AF, Brooks DE (September 2008). "Dextromethorphan-induced serotonin syndrome". Clinical Toxicology. 46 (8): 771–3. doi:10.1080/15563650701668625. PMID 19238739.
- Shin EJ, Nah SY, Chae JS, Bing G, Shin SW, Yen TP, et al. (May 2007). "Dextromethorphan attenuates trimethyltin-induced neurotoxicity via sigma1 receptor activation in rats". Neurochemistry International. 50 (6): 791–9. doi:10.1016/j.neuint.2007.01.008. PMID 17386960.
- Shin EJ, Nah SY, Kim WK, Ko KH, Jhoo WK, Lim YK, et al. (April 2005). "The dextromethorphan analog dimemorfan attenuates kainate-induced seizures via sigma1 receptor activation: comparison with the effects of dextromethorphan". British Journal of Pharmacology. 144 (7): 908–18. doi:10.1038/sj.bjp.0705998. PMC 1576070. PMID 15723099.
- Fischer, Jnos; Ganellin, C. Robin (2006). Analogue-based Drug Discovery. John Wiley & Sons. p. 527. ISBN 9783527607495.
- Rossi, S, ed. (2013). Australian Medicines Handbook. Adelaide: The Australian Medicines Handbook Unit Trust. ISBN 978-0-9805790-9-3.
- Van Amburgh JA. "Do Cough Remedies Work?". Medscape. Retrieved 10 April 2016.
- Nguyen L, Thomas KL, Lucke-Wold BP, Cavendish JZ, Crowe MS, Matsumoto RR (March 2016). "Dextromethorphan: An update on its utility for neurological and neuropsychiatric disorders". Pharmacology & Therapeutics. 159: 1–22. doi:10.1016/j.pharmthera.2016.01.016. PMID 26826604.
- Malek A, Amiri S, Habibi Asl B (2013). "The therapeutic effect of adding dextromethorphan to clonidine for reducing symptoms of opioid withdrawal: a randomized clinical trial". ISRN Psychiatry. 2013: 546030. doi:10.1155/2013/546030. PMC 3706070. PMID 23864983.
- Amiri HR, Mirzaei M, Beig Mohammadi MT, Tavakoli F (August 2016). "Multi-Modal Preemptive Analgesia With Pregabalin, Acetaminophen, Naproxen, and Dextromethorphan in Radical Neck Dissection Surgery: A Randomized Clinical Trial". Anesthesiology and Pain Medicine. 6 (4): e33526. doi:10.5812/aapm.33526. PMC 5099949. PMID 27843771.
- "Dextromethorphan". National Highway Traffic Safety Administration (NHTSA). Archived from the original on 2008-08-01.
- Olney JW, Labruyere J, Price MT (June 1989). "Pathological changes induced in cerebrocortical neurons by phencyclidine and related drugs". Science. 244 (4910): 1360–2. Bibcode:1989Sci...244.1360O. doi:10.1126/science.2660263. PMID 2660263.
- Carliss RD, Radovsky A, Chengelis CP, O'Neill TP, Shuey DL (July 2007). "Oral administration of dextromethorphan does not produce neuronal vacuolation in the rat brain". Neurotoxicology. 28 (4): 813–8. doi:10.1016/j.neuro.2007.03.009. PMID 17573115.
- WHO Expert Committee on Drug Dependence, Seventeenth Report (PDF). World Health Organization. 1970. p. 24. Retrieved 2008-12-29.
- "Teen Drug Abuse: Cough Medicine and DXM (Dextromethorphan)". webmd. Archived from the original on 2017-11-21.
- Martinak B, Bolis RA, Black JR, Fargason RE, Birur B (September 2017). "Dextromethorphan in Cough Syrup: The Poor Man's Psychosis". Psychopharmacology Bulletin. 47 (4): 59–63. PMC 5601090. PMID 28936010.
- Martinak B, Bolis RA, Black JR, Fargason RE, Birur B (September 2017). "Dextromethorphan in Cough Syrup: The Poor Man's Psychosis". Psychopharmacology Bulletin. 47 (4): 59–63. PMC 5601090. PMID 28936010.
- "Inhibitors of CYP3A4". ganfyd.org. Archived from the original on 2017-07-20. Retrieved 23 August 2013.
- Roth, BL; Driscol, J. "PDSP Ki Database". Psychoactive Drug Screening Program (PDSP). University of North Carolina at Chapel Hill and the United States National Institute of Mental Health. Retrieved 14 August 2017.
- Nguyen L, Thomas KL, Lucke-Wold BP, Cavendish JZ, Crowe MS, Matsumoto RR (March 2016). "Dextromethorphan: An update on its utility for neurological and neuropsychiatric disorders" (PDF). Pharmacology & Therapeutics. 159: 1–22. doi:10.1016/j.pharmthera.2016.01.016. PMID 26826604.
- Werling LL, Keller A, Frank JG, Nuwayhid SJ (October 2007). "A comparison of the binding profiles of dextromethorphan, memantine, fluoxetine and amitriptyline: treatment of involuntary emotional expression disorder". Experimental Neurology. 207 (2): 248–57. doi:10.1016/j.expneurol.2007.06.013. PMID 17689532.
- Taylor CP, Traynelis SF, Siffert J, Pope LE, Matsumoto RR (August 2016). "Pharmacology of dextromethorphan: Relevance to dextromethorphan/quinidine (Nuedexta®) clinical use". Pharmacology & Therapeutics. 164: 170–82. doi:10.1016/j.pharmthera.2016.04.010. PMID 27139517.
- Raynor K, Kong H, Mestek A, Bye LS, Tian M, Liu J, et al. (January 1995). "Characterization of the cloned human mu opioid receptor". The Journal of Pharmacology and Experimental Therapeutics. 272 (1): 423–8. PMID 7815359.
- Lee JH, Shin EJ, Jeong SM, Lee BH, Yoon IS, Lee JH, et al. (June 2007). "Effects of dextrorotatory morphinans on brain Na+ channels expressed in Xenopus oocytes". European Journal of Pharmacology. 564 (1–3): 7–17. doi:10.1016/j.ejphar.2007.01.088. PMID 17346698.
- Gao XF, Yao JJ, He YL, Hu C, Mei YA (2012). "Sigma-1 receptor agonists directly inhibit Nav1.2/1.4 channels". PLOS ONE. 7 (11): e49384. Bibcode:2012PLoSO...749384G. doi:10.1371/journal.pone.0049384. PMC 3489664. PMID 23139844.
- Burns JM, Boyer EW (2013). "Antitussives and substance abuse". Substance Abuse and Rehabilitation. 4: 75–82. doi:10.2147/SAR.S36761. PMC 3931656. PMID 24648790.
- Chou YC, Liao JF, Chang WY, Lin MF, Chen CF (March 1999). "Binding of dimemorfan to sigma-1 receptor and its anticonvulsant and locomotor effects in mice, compared with dextromethorphan and dextrorphan". Brain Research. 821 (2): 516–9. doi:10.1016/S0006-8993(99)01125-7. PMID 10064839.
- Schmider J, Greenblatt DJ, Fogelman SM, von Moltke LL, Shader RI (April 1997). "Metabolism of dextromethorphan in vitro: involvement of cytochromes P450 2D6 and 3A3/4, with a possible role of 2E1". Biopharmaceutics & Drug Disposition. 18 (3): 227–40. doi:10.1002/(SICI)1099-081X(199704)18:3<227::AID-BDD18>3.0.CO;2-L. PMID 9113345.
- Morice AH. "Cough". International Society for the Study of Cough. Archived from the original on 2017-05-09.
- Strauch K, Lutz U, Bittner N, Lutz WK (August 2009). "Dose-response relationship for the pharmacokinetic interaction of grapefruit juice with dextromethorphan investigated by human urinary metabolite profiles". Food and Chemical Toxicology. 47 (8): 1928–35. doi:10.1016/j.fct.2009.05.004. PMID 19445995.
- Yu A, Haining RL (November 2001). "Comparative contribution to dextromethorphan metabolism by cytochrome P450 isoforms in vitro: can dextromethorphan be used as a dual probe for both CTP2D6 and CYP3A activities?". Drug Metabolism and Disposition. 29 (11): 1514–20. PMID 11602530.
- Capon DA, Bochner F, Kerry N, Mikus G, Danz C, Somogyi AA (September 1996). "The influence of CYP2D6 polymorphism and quinidine on the disposition and antitussive effect of dextromethorphan in humans". Clinical Pharmacology and Therapeutics. 60 (3): 295–307. doi:10.1016/S0009-9236(96)90056-9. PMID 8841152.
- Woodworth JR, Dennis SR, Moore L, Rotenberg KS (February 1987). "The polymorphic metabolism of dextromethorphan". Journal of Clinical Pharmacology. 27 (2): 139–43. doi:10.1002/j.1552-4604.1987.tb02174.x. PMID 3680565.
- "Dextromethorphan (PIM 179)". www.inchem.org. Archived from the original on 2017-03-10. Retrieved 2018-03-24.
- Morris H, Wallach J (2014). "From PCP to MXE: a comprehensive review of the non-medical use of dissociative drugs". Drug Testing and Analysis. 6 (7–8): 614–32. doi:10.1002/dta.1620. PMID 24678061.
- "Memorandum for the Secretary of Defense" (PDF). Archived (PDF) from the original on 2017-09-16. Retrieved 2013-07-28.
- "Dextromethorphan (DXM)". Cesar.umd.edu. Archived from the original on 2018-01-06. Retrieved 2013-07-28.
- "Senate Bill No. 514" (PDF). An act to add Sections 11110 and 11111 to the Health and Safety Code, relating to nonprescription drugs. State of California, Legislative Counsel. Archived (PDF) from the original on 2018-03-08.
- http://nasional.news.viva.co.id/news/read/506418-bpom-tetap-batalkan-izin-edar-obat-dekstrometorfan Archived 2015-05-28 at the Wayback Machine
- "SINDOnews | Berita Daerah Dan Provinsi Di Indonesia". daerah.sindonews.com (in Indonesian). Retrieved 2017-12-10.
- "Pimpinan dan Apoteker Penanggung Jawab" (PDF). Archived from the original (PDF) on 2017-08-10.
- "Badan Pengawas Obat dan Makanan - Republik Indonesia". www.pom.go.id. Archived from the original on 2017-02-03. Retrieved 2017-12-10.
- "Fake drugs: the global industry putting your life at risk". Mosaic. 30 October 2018. Retrieved 13 December 2018.
- "Dextromethorphan" (PDF). Drugs and Chemicals of Concern. Drug Enforcement Administration. August 2010. Archived from the original (PDF) on 2012-10-16.
- Giannini AJ (1997). Drugs of abuse (2nd ed.). Los Angeles: Practice Management Information Corp. ISBN 1570660530.
- Ackerman, Sarah C.; Hammel, John L.; Brunette, Mary F. (2010-12-20). "Dextromethorphan Abuse and Dependence in Adolescents". Journal of Dual Diagnosis. 6 (3–4): 266–278. doi:10.1080/15504263.2010.537515.
External links
| Wikimedia Commons has media related to Dextromethorphan. |