Tetrahydrocannabinol
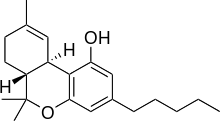
Tetrahydrocannabinol (THC) is one of at least 113 cannabinoids identified in cannabis. THC is the principal psychoactive constituent of cannabis. With chemical name (−)-trans-Δ⁹-tetrahydrocannabinol, the term THC also refers to cannabinoid isomers.
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Marinol |
| Other names | (6aR,10aR)-delta-9-Tetrahydrocannabinol; (−)-trans-Δ⁹-Tetrahydrocannabinol; THC |
| License data |
|
| Pregnancy category |
|
| Dependence liability | 8–10% (Relatively low risk of tolerance)[1] |
| Routes of administration | Oral, local/topical, transdermal, sublingual, inhaled |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | 10–35% (inhalation), 6–20% (oral)[3] |
| Protein binding | 97–99%[3][4][5] |
| Metabolism | Mostly hepatic by CYP2C[3] |
| Elimination half-life | 1.6–59 h,[3] 25–36 h (orally administered dronabinol) |
| Excretion | 65–80% (feces), 20–35% (urine) as acid metabolites[3] |
| Identifiers | |
IUPAC name
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.153.676 |
| Chemical and physical data | |
| Formula | C21H30O2 |
| Molar mass | 314.469 g·mol−1 |
| 3D model (JSmol) | |
| Specific rotation | −152° (ethanol) |
| Boiling point | 155-157°C @ 0.05mmHg,[6] 157-160°C @ 0.05mmHg[7] |
| Solubility in water | 0.0028,[8] (23 °C) mg/mL (20 °C) |
SMILES
| |
InChI
| |
| | |
Like most pharmacologically-active secondary metabolites of plants, THC is a lipid found in cannabis,[9] assumed to be involved in the plant's self-defense, putatively against insect predation, ultraviolet light, and environmental stress.[10][11][12]
THC, along with its double bond isomers and their stereoisomers[13], is one of only three cannabinoids scheduled by the UN Convention on Psychotropic Substances (the other two are dimethylheptylpyran and parahexyl). It was listed under Schedule I in 1971, but reclassified to Schedule II in 1991 following a recommendation from the WHO. Based on subsequent studies, the WHO has recommended the reclassification to the less-stringent Schedule III.[14] Cannabis as a plant is scheduled by the Single Convention on Narcotic Drugs (Schedule I and IV). It is specifically still listed under Schedule I by US federal law[15] under the Controlled Substances Act for having "no accepted medical use" and "lack of accepted safety". However, dronabinol is a synthetic form of THC approved by the FDA as an appetite stimulant for people with AIDS and antiemetic for people receiving chemotherapy.[16] The pharmaceutical formulation dronabinol is an oily resin provided in capsules available by prescription in the United States, Canada, Germany, and New Zealand.
Medical uses
THC is an active ingredient in Nabiximols, a specific extract of Cannabis that was approved as a botanical drug in the United Kingdom in 2010 as a mouth spray for people with multiple sclerosis to alleviate neuropathic pain, spasticity, overactive bladder, and other symptoms.[17][18] Nabiximols (as Sativex) is available as a prescription drug in Canada.[19]
Pharmacology
Mechanism of action
The actions of THC result from its partial agonist activity at the cannabinoid receptor CB1 (Ki = 10 nM[20]), located mainly in the central nervous system, and the CB2 receptor (Ki = 24 nM[20]), mainly expressed in cells of the immune system.[21] The psychoactive effects of THC are primarily mediated by the activation of cannabinoid receptors, which result in a decrease in the concentration of the second messenger molecule cAMP through inhibition of adenylate cyclase.[22]
The presence of these specialized cannabinoid receptors in the brain led researchers to the discovery of endocannabinoids, such as anandamide and 2-arachidonoyl glyceride (2-AG). THC targets receptors in a manner far less selective than endocannabinoid molecules released during retrograde signaling, as the drug has a relatively low cannabinoid receptor efficacy and affinity. In populations of low cannabinoid receptor density, THC may act to antagonize endogenous agonists that possess greater receptor efficacy.[23] THC is a lipophilic molecule[24] and may bind non-specifically to a variety of entities in the brain and body, such as adipose tissue (fat).[25][26]
THC, similarly to cannabidiol, albeit less potently, is a positive allosteric modulator of the μ- and δ-opioid receptors.[27]
Due to its partial agonistic activity, THC appears to result in greater downregulation of cannabinoid receptors than endocannabinoids, further limiting its efficacy over other cannabinoids. While tolerance may limit the maximal effects of certain drugs, evidence suggests that tolerance develops irregularly for different effects with greater resistance for primary over side-effects, and may actually serve to enhance the drug's therapeutic window.[23] However, this form of tolerance appears to be irregular throughout mouse brain areas. THC, as well as other cannabinoids that contain a phenol group, possesses mild antioxidant activity sufficient to protect neurons against oxidative stress, such as that produced by glutamate-induced excitotoxicity.[21]
Pharmacokinetics
THC is metabolized mainly to 11-OH-THC by the body. This metabolite is still psychoactive and is further oxidized to 11-nor-9-carboxy-THC (THC-COOH). In humans and animals, more than 100 metabolites could be identified, but 11-OH-THC and THC-COOH are the dominating metabolites.[28] Metabolism occurs mainly in the liver by cytochrome P450 enzymes CYP2C9, CYP2C19, and CYP3A4.[29] More than 55% of THC is excreted in the feces and ≈20% in the urine. The main metabolite in urine is the ester of glucuronic acid and THC-COOH and free THC-COOH. In the feces, mainly 11-OH-THC was detected.[30]
Physical and chemical properties
Discovery and structure identification
In 1940, cannabidiol was isolated and identified from Cannabis sativa,[31] and THC was isolated and described for its structure and synthesis in 1964.[32][33]
Solubility
As with many aromatic terpenoids, THC has a very low solubility in water, but good solubility in most organic solvents, specifically lipids and alcohols.[8]
Total synthesis
A total synthesis of the compound was reported in 1965; that procedure called for the intramolecular alkyl lithium attack on a starting carbonyl to form the fused rings, and a tosyl chloride mediated formation of the ether.[34]
Biosynthesis
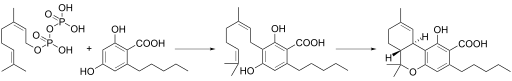
In the Cannabis plant, THC occurs mainly as tetrahydrocannabinolic acid (THCA, 2-COOH-THC, THC-COOH). Geranyl pyrophosphate and olivetolic acid react, catalysed by an enzyme to produce cannabigerolic acid,[35] which is cyclized by the enzyme THC acid synthase to give THCA. Over time, or when heated, THCA is decarboxylated, producing THC. The pathway for THCA biosynthesis is similar to that which produces the bitter acid humulone in hops.[36][37]
Detection in body fluids
THC and its 11-OH-THC and THC-COOH metabolites can be detected and quantified in blood, urine, hair, oral fluid or sweat using a combination of immunoassay and chromatographic techniques as part of a drug use testing program or in a forensic investigation.[38][39][40]
History
THC was first isolated in 1964 by Raphael Mechoulam and Yechiel Gaoni at the Weizmann Institute of Science in Israel.[32][41][42]
At its 33rd meeting, in 2003, the World Health Organization Expert Committee on Drug Dependence recommended transferring THC to Schedule IV of the Convention, citing its medical uses and low abuse potential.[43]
Society and culture
Comparisons with medical cannabis
| Part of a series on |
| Cannabis |
|---|
 |
|
|
Chemistry
|
|
Consumption
|
|
Economics
|
|
|
Forms
|
|
Law
|
|
Regional
|
|
Variants
|
|
Related
|
|
Female cannabis plants contain at least 113 cannabinoids,[44] including cannabidiol (CBD), thought to be the major anticonvulsant that helps people with multiple sclerosis;[45] and cannabichromene (CBC), an anti-inflammatory which may contribute to the pain-killing effect of cannabis.[46]
Regulation in Canada
As of October 2018 when recreational use of cannabis was legalized in Canada, some 220 dietary supplements and 19 veterinary health products containing not more than 10 parts per million of THC extract were approved with general health claims for treating minor conditions.[19]
Research
The status of THC as an illegal drug in most countries imposes restrictions on research material supply and funding, such as in the United States where the National Institute on Drug Abuse and Drug Enforcement Administration regulated sources of cannabis for researchers until August 2016 when licenses were provided to growers for supplies of medical marijuana.[47] Although cannabis is legalized for medical uses in half of the United States, no products have been approved for federal commerce by the Food and Drug Administration, a status that limits cultivation, manufacture, distribution, clinical research, and therapeutic applications.[48]
In April 2014, the American Academy of Neurology found evidence supporting the effectiveness of the cannabis extracts in treating certain symptoms of multiple sclerosis and pain, but there was insufficient evidence to determine effectiveness for treating several other neurological diseases.[49] A 2015 review confirmed that medical marijuana was effective for treating spasticity and chronic pain, but caused numerous short-lasting adverse events, such as euphoria and dizziness.[50]
Multiple sclerosis symptoms
- Spasticity. Based on the results of 3 high quality trials and 5 of lower quality, oral cannabis extract was rated as effective, and THC as probably effective, for improving people's subjective experience of spasticity. Oral cannabis extract and THC both were rated as possibly effective for improving objective measures of spasticity.[49][50]
- Centrally mediated pain and painful spasms. Based on the results of 4 high quality trials and 4 low quality trials, oral cannabis extract was rated as effective, and THC as probably effective in treating central pain and painful spasms.[49]
- Bladder dysfunction. Based on a single high quality study, oral cannabis extract and THC were rated as probably ineffective for controlling bladder complaints in multiple sclerosis[49]
Neurodegenerative disorders
- Huntington disease. No reliable conclusions could be drawn regarding the effectiveness of THC or oral cannabis extract in treating the symptoms of Huntington disease as the available trials were too small to reliably detect any difference[49]
- Parkinson's disease. Based on a single study, oral CBD extract was rated probably ineffective in treating levodopa-induced dyskinesia in Parkinson's disease.[49]
- Alzheimer's disease. A 2009 Cochrane Review found insufficient evidence to conclude whether cannabis products have any utility in the treatment of Alzheimer's disease.[51]
Other neurological disorders
- Tourette syndrome. The available data was determined to be insufficient to allow reliable conclusions to be drawn regarding the effectiveness of oral cannabis extract or THC in controlling tics.[49]
- Cervical dystonia. Insufficient data was available to assess the effectiveness of oral cannabis extract of THC in treating cervical dystonia.[49]
See also
- Cannabinoids
- 11-Hydroxy-THC, metabolite of THC
- Anandamide, 2-Arachidonoylglycerol, endogenous cannabinoid agonists
- Cannabidiol (CBD), an isomer of THC
- Cannabinol (CBN), a metabolite of THC
- Dimethylheptylpyran
- Parahexyl
- Tetrahydrocannabinolic acid, the biosynthetic precursor for THC
- HU-210, WIN 55,212-2, JWH-133, synthetic cannabinoid agonists
- Medical cannabis
- Nabilone
- War on Drugs
- Effects of cannabis
- Cannabinoid hyperemesis syndrome
- List of investigational analgesics
References
- Marlowe, Douglas B (December 2010). "The Facts On Marijuana". NADCP.
Based upon several nationwide epidemiological studies, marijuana’s dependence liability has been reliably determined to be 8 to 10 percent.
Cite journal requires|journal=(help) - "Archived copy" (PDF). Archived from the original (PDF) on 2014-05-13. Retrieved 2014-03-14.CS1 maint: archived copy as title (link)
- Grotenhermen, F (2003). "Pharmacokinetics and pharmacodynamics of cannabinoids". Clin Pharmacokinet. 42 (4): 327–60. doi:10.2165/00003088-200342040-00003. PMID 12648025.
- The Royal Pharmaceutical Society of Great Britain (30 November 2006). "Cannabis". In Sean C. Sweetman (ed.). Martindale: The Complete Drug Reference: Single User (35th ed.). Pharmaceutical Press. ISBN 978-0-85369-703-9.
- "Tetrahydrocannabinol – Compound Summary". National Center for Biotechnology Information. PubChem. Retrieved 12 January 2014.
Dronabinol has a large apparent volume of distribution, approximately 10 L/kg, because of its lipid solubility. The plasma protein binding of dronabinol and its metabolites is approximately 97%.
- Gaoni, Y.; Mechoulam, R. (April 1964). "Isolation, Structure, and Partial Synthesis of an Active Constituent of Hashish". Journal of the American Chemical Society. 86 (8): 1646–1647. doi:10.1021/ja01062a046.
- Adams, Roger; Cain, C. K.; McPhee, W. D.; Wearn, R. B. (August 1941). "Structure of Cannabidiol. XII. Isomerization to Tetrahydrocannabinols". Journal of the American Chemical Society. 63 (8): 2209–2213. doi:10.1021/ja01853a052.
- Garrett ER, Hunt CA (July 1974). "Physicochemical properties, solubility, and protein binding of Δ9-tetrahydrocannabinol". J. Pharm. Sci. 63 (7): 1056–64. doi:10.1002/jps.2600630705. PMID 4853640.
- Firn, Richard (2010). Nature's Chemicals. Oxford: Biology.
- Pate, David W. (1994). "Chemical ecology of Cannabis". Journal of the International Hemp Association. 2 (29): 32–37.
- Pate, David W. (1983). "Possible role of ultraviolet radiation in evolution of Cannabis chemotypes". Economic Botany. 37 (4): 396–405. doi:10.1007/BF02904200.
- Lydon J, Teramura AH, Coffman CB (1987). "UV-B radiation effects on photosynthesis, growth and cannabinoid production of two Cannabis sativa chemotypes". Photochemistry and Photobiology. 46 (2): 201–206. doi:10.1111/j.1751-1097.1987.tb04757.x. PMID 3628508.
- Mazzoccanti, G.; Ismail, O. H.; D’Acquarica, I.; Villani, C.; Manzo, C.; Wilcox, M.; Cavazzini, A.; Gasparrini, F. (2017). "Cannabis through the looking glass: chemo- and enantio-selective separation of phytocannabinoids by enantioselective ultra high performance supercritical fluid chromatography" (PDF). Chemical Communications. 53 (91): 12262–12265. doi:10.1039/C7CC06999E. hdl:11573/1016698. ISSN 1359-7345.
- "The UN Drug Control Conventions". 8 October 2015.
- "Drug Schedules; Schedule 1". US Drug Enforcement Administration, Department of Justice. 1 December 2017. Retrieved 14 January 2018.
- "Marinol (Dronabinol)" (PDF). US Food and Drug Administration. September 2004. Retrieved 14 January 2018.
- "Sativex Oromucosal Spray - Summary of Product Characteristics". UK Electronic Medicines Compendium. March 2015.
- Multiple Sclerosis Trust. October 2014 Sativex (nabiximols) - factsheet
- "Health products containing cannabis or for use with cannabis: Guidance for the Cannabis Act, the Food and Drugs Act, and related regulations". Government of Canada. 11 July 2018. Retrieved 19 October 2018.
- "PDSP Database – UNC". NIMH Psychoactive Drug Screening Program. Archived from the original on 8 November 2013. Retrieved 11 June 2013.
- Pertwee RG (2006). "The pharmacology of cannabinoid receptors and their ligands: An overview". International Journal of Obesity. 30: S13–S18. doi:10.1038/sj.ijo.0803272. PMID 16570099.
- Elphick MR, Egertová M (2001). "The neurobiology and evolution of cannabinoid signalling". Philosophical Transactions of the Royal Society B: Biological Sciences. 356 (1407): 381–408. doi:10.1098/rstb.2000.0787. PMC 1088434. PMID 11316486.
- Pertwee RG (2008). "The diverse CB1 and CB2 receptor pharmacology of three plant cannabinoids: Δ9-tetrahydrocannabinol, cannabidiol and Δ9-tetrahydrocannabivarin". British Journal of Pharmacology. 153 (2): 199–215. doi:10.1038/sj.bjp.0707442. PMC 2219532. PMID 17828291.
- Rashidi H, Akhtar MT, van der Kooy F, Verpoorte R, Duetz WA (November 2009). "Hydroxylation and Further Oxidation of Δ9-Tetrahydrocannabinol by Alkane-Degrading Bacteria". Appl Environ Microbiol. 75 (22): 7135–7141. doi:10.1128/AEM.01277-09. PMC 2786519. PMID 19767471.
Δ9-THC and many of its derivatives are highly lipophilic and poorly water soluble. Calculations of the n-octanol/water partition coefficient (Ko/w) of Δ9-THC at neutral pH vary between 6,000, using the shake flask method, and 9.44 × 106, by reverse-phase high-performance liquid chromatography estimation.
- Ashton CH (February 2001). "Pharmacology and effects of cannabis: a brief review". Br J Psychiatry. 178 (2): 101–106. doi:10.1192/bjp.178.2.101. PMID 11157422.
Because they are extremely lipid soluble, cannabinoids accumulate in fatty tissues, reaching peak concentrations in 4–5 days. They are then slowly released back into other body compartments, including the brain. ... Within the brain, THC and other cannabinoids are differentially distributed. High concentrations are reached in neocortical, limbic, sensory and motor areas.
- Huestis MA (August 2007). "Human cannabinoid pharmacokinetics". Chem Biodivers. 4 (8): 1770–804. doi:10.1002/cbdv.200790152. PMC 2689518. PMID 17712819.
THC is highly lipophilic and initially taken up by tissues that are highly perfused, such as the lung, heart, brain, and liver.
- Kathmann M, Flau K, Redmer A, Tränkle C, Schlicker E (February 2006). "Cannabidiol is an allosteric modulator at mu- and delta-opioid receptors". Naunyn Schmiedebergs Arch. Pharmacol. 372 (5): 354–61. doi:10.1007/s00210-006-0033-x. PMID 16489449.
- Aizpurua-Olaizola, Oier; Zarandona, Iratxe; Ortiz, Laura; Navarro, Patricia; Etxebarria, Nestor; Usobiaga, Aresatz (2016-01-01). "Simultaneous quantification of major cannabinoids and metabolites in human urine and plasma by HPLC-MS/MS and enzyme-alkaline hydrolysis". Drug Testing and Analysis. 9 (4): 626–633. doi:10.1002/dta.1998. ISSN 1942-7611. PMID 27341312.
- Watanabe K, Yamaori S, Funahashi T, Kimura T, Yamamoto I (March 2007). "Cytochrome P450 enzymes involved in the metabolism of tetrahydrocannabinols and cannabinol by human hepatic microsomes". Life Science. 80 (15): 1415–9. doi:10.1016/j.lfs.2006.12.032. PMID 17303175.
- Huestis MA (2005). Pharmacokinetics and Metabolism of the Plant Cannabinoids, Δ9-Tetrahydrocannabinol, Cannabidiol and Cannabinol. Cannabinoids. Handbook of Experimental Pharmacology. 168. pp. 657–90. doi:10.1007/3-540-26573-2_23. ISBN 978-3-540-22565-2. PMID 16596792.
- Roger Adams, Madison Hunt, J. H. Clark (1940). "Structure of Cannabidiol, a Product Isolated from the Marihuana Extract of Minnesota Wild Hemp". Journal of the American Chemical Society. 62: 196–200. doi:10.1021/ja01858a058.CS1 maint: multiple names: authors list (link)
- Gaoni Y, Mechoulam R (1964). "Isolation, structure and partial synthesis of an active constituent of hashish". Journal of the American Chemical Society. 86 (8): 1646–1647. doi:10.1021/ja01062a046.
- Mechoulam R (1970). "Marihuana chemistry". Science. 168 (3936): 1159–66. Bibcode:1970Sci...168.1159M. doi:10.1126/science.168.3936.1159. PMID 4910003.
- Mechoulam R, Gaoni Y (1965). "A Total Synthesis of dl-Δ1-Tetrahydrocannabinol, the Active Constituent of Hashish". J. Am. Chem. Soc. 87 (14): 3273–3275. doi:10.1021/ja01092a065.
- Fellermeier M, Zenk MH (1998). "Prenylation of olivetolate by a hemp transferase yields cannabigerolic acid, the precursor of tetrahydrocannabinol". FEBS Letters. 427 (2): 283–5. doi:10.1016/S0014-5793(98)00450-5. PMID 9607329.
- Marks MD, Tian L, Wenger JP, Omburo SN, Soto-Fuentes W, He J, Gang DR, Weiblen GD, Dixon RA (2009). "Identification of candidate genes affecting Δ9-tetrahydrocannabinol biosynthesis in Cannabis sativa". Journal of Experimental Botany. 60 (13): 3715–26. doi:10.1093/jxb/erp210. PMC 2736886. PMID 19581347.
- Baker PB, Taylor BJ, Gough TA (June 1981). "The tetrahydrocannabinol and tetrahydrocannabinolic acid content of cannabis products". J Pharm Pharmacol. 33 (6): 369–72. doi:10.1111/j.2042-7158.1981.tb13806.x. PMID 6115009.
- Schwilke EW, Schwope DM, Karschner EL, Lowe RH, Darwin WD, Kelly DL, Goodwin RS, Gorelick DA, Huestis MA (2009). "Δ9-Tetrahydrocannabinol (THC), 11-Hydroxy-THC, and 11-Nor-9-carboxy-THC Plasma Pharmacokinetics during and after Continuous High-Dose Oral THC". Clinical Chemistry. 55 (12): 2180–2189. doi:10.1373/clinchem.2008.122119. PMC 3196989. PMID 19833841.
- Röhrich J, Schimmel I, Zörntlein S, Becker J, Drobnik S, Kaufmann T, Kuntz V, Urban R (2010). "Concentrations of Δ9-Tetrahydrocannabinol and 11-Nor-9-Carboxytetrahydrocannabinol in Blood and Urine After Passive Exposure to Cannabis Smoke in a Coffee Shop". Journal of Analytical Toxicology. 34 (4): 196–203. doi:10.1093/jat/34.4.196. PMID 20465865.
- Baselt, R. (2011). Disposition of Toxic Drugs and Chemicals in Man (9th ed.). Seal Beach, CA: Biomedical Publications. pp. 1644–8.
- "Interview with the winner of the first ECNP Lifetime Achievement Award: Raphael Mechoulam, Israel". February 2007. Archived from the original on 2011-04-30.
- Geller, Tom (2007). "Cannabinoids: A Secret History". Chemical Heritage Newsmagazine. 25 (2). Archived from the original on 19 June 2008.
- "WHO Expert Committee on Drug Dependence". World Health Organization. Retrieved 12 January 2014.
- Aizpurua-Olaizola, Oier; Soydaner, Umut; Öztürk, Ekin; Schibano, Daniele; Simsir, Yilmaz; Navarro, Patricia; Etxebarria, Nestor; Usobiaga, Aresatz (2016-02-26). "Evolution of the Cannabinoid and Terpene Content during the Growth of Cannabis sativa Plants from Different Chemotypes". Journal of Natural Products. 79 (2): 324–331. doi:10.1021/acs.jnatprod.5b00949. ISSN 0163-3864. PMID 26836472.
- Pickens JT (1981). "Sedative activity of cannabis in relation to its delta'-trans-tetrahydrocannabinol and cannabidiol content". British Journal of Pharmacology. 72 (4): 649–56. doi:10.1111/j.1476-5381.1981.tb09145.x. PMC 2071638. PMID 6269680.
- Morales, Paula; Hurst, Dow P.; Reggio, Patricia H. (2017). "Molecular Targets of the Phytocannabinoids: A Complex Picture". In Kinghorn, A. Douglas; Falk, Heinz; Gibbons, Simon; Kobayashi, Jun'ichi (eds.). Phytocannabinoids: Unraveling the Complex Chemistry and Pharmacology of Cannabis sativa. Progress in the Chemistry of Organic Natural Products. 103. Springer International Publishing. pp. 103–131. doi:10.1007/978-3-319-45541-9_4. ISBN 978-3-319-45539-6. PMC 5345356. PMID 28120232.
- "Medical Marijuana". Multidisciplinary Association for Psychoactive Substances. Retrieved 12 January 2014.
- Mead, A (2017). "The legal status of cannabis (marijuana) and cannabidiol (CBD) under U.S. Law". Epilepsy & Behavior. 70 (Pt B): 288–291. doi:10.1016/j.yebeh.2016.11.021. PMID 28169144.
- Koppel BS, Brust JC, Fife T, Bronstein J, Youssof S, Gronseth G, Gloss D (April 2014). "Systematic review: Efficacy and safety of medical marijuana in selected neurologic disorders: Report of the Guideline Development Subcommittee of the American Academy of Neurology". Neurology. 82 (17): 1556–63. doi:10.1212/WNL.0000000000000363. PMC 4011465. PMID 24778283.
- Whiting, P. F; Wolff, R. F; Deshpande, S; Di Nisio, M; Duffy, S; Hernandez, A. V; Keurentjes, J. C; Lang, S; Misso, K; Ryder, S; Schmidlkofer, S; Westwood, M; Kleijnen, J (2015). "Cannabinoids for Medical Use: A Systematic Review and Meta-analysis" (PDF). JAMA. 313 (24): 2456–73. doi:10.1001/jama.2015.6358. PMID 26103030.
- Krishnan S, Cairns R, Howard R (2009). Krishnan S (ed.). "Cannabinoids for the treatment of dementia". Cochrane Database of Systematic Reviews (2): CD007204. doi:10.1002/14651858.CD007204.pub2. PMID 19370677.