Perampanel
Perampanel (sold under the trade name Fycompa) is an antiepileptic drug developed by Eisai Co. that is used in addition to other drugs to treat partial seizures and generalized tonic-clonic seizures for people older than 12 years.[2] It was first approved in 2012 and as of 2016 its optimal role in the treatment of epilepsy relative to other drugs was not clear.[3] It was the first antiepileptic drug in the class of selective non-competitive antagonist of AMPA receptors.[4]
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Fycompa |
| Other names | E2007 |
| License data |
|
| Pregnancy category | |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | 116%[1] |
| Protein binding | 95–96% |
| Metabolism | hepatic, mostly via CYP3A4 and/or CYP3A5 |
| Elimination half-life | 105 hrs, 295 hrs (moderate hepatic impairment) |
| Excretion | 70% faeces, 30% urine |
| Identifiers | |
IUPAC name
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| PDB ligand | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.219.846 |
| Chemical and physical data | |
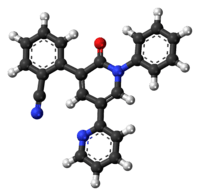
| Formula | C23H15N3O |
| Molar mass | 349.384 g/mol g·mol−1 |
| 3D model (JSmol) | |
SMILES
| |
InChI
| |
| | |
The drug label has a black box warning that the drug cause may cause serious psychiatric and behavioral changes; it may cause homicidal or suicidal thoughts.[2] Other side effects have included dizziness, somnolence, vertigo, aggression, anger, loss of coordination, blurred vision, irritability, and slurred speech.[2] Perampanel reduced the effectiveness of levonorgestrel oral contraceptives by about 40%.[2] Women who may get pregnant should not take it as studies in animals show it may harm a fetus.[5] Perampanel is liable to be abused; very high doses produced euphoria responses similar to ketamine.[2] It is designated as a Schedule III controlled substance by the Drug Enforcement Administration.[2]
As of August 2016 perampanel had been studied and development discontinued in migraine, multiple sclerosis, neuropathic pain, and Parkinson's disease.[6]
Medical uses
Perampanel is used in addition to other drugs to treat partial seizures and generalized tonic-clonic seizures for people older than 12 years.[2]
A 2016 review found it effective for both indications but due to the newness of the drug was unable to describe its optimal role in the treatment of epilepsy relative to other drugs.[3] A 2014 review of the probability of added benefit of perampanel to the standard of care was unable to come to any conclusions, as no trial conducted by Eisai compared perampanel to a drug within the standard of care, but only to placebo.[7]
Contraindications and drug interactions
Based on animal data, perampanel may cause fetal harm;[2] it is not recommended for women of child-bearing age not taking contraception.[5]
People with severe liver impairment or severe kidney disease, including those on dialysis, should not take perampanel.[2]
Perampanel reduced the effectiveness of levonorgestrel oral contraceptives by about 40%. Other antieptilectic drugs that induce cytochrome P450, including carbamazepine, phenytoin, and oxcarbazepine decrease the effectivenes of perampanel by 50-67%. Use of perampanel with strong CYP3A inducers like rifampin or St. John's wort is not recommended. Use of perampanel with CNS depressants like alcohol may increase the effect of the CNS depressant.[2]
Side effects
Perampanel's label has a black box warning noting that some people taking the drug have undergone serious psychiatric and behavioral changes. These events occurred in people who had no history of such issues, as well as people who had such a history. The psychiatric changes included mood changes like euphoric mood, anger, irritability, aggression, belligerence, agitation, and anxiety, as well as psychosis (acute psychosis, hallucinations, delusions, paranoia) and delirium (delirium, confusional state, disorientation, memory impairment). Behavioral changes included physical assault and homicidal ideation and/or threats.[2]
Other serious side effects include suicidal thoughts or behavior (like all anti-epileptic drugs), dizziness and gait disturbance, somnolence and fatigue, risk of falls, and increased risk of seizures if the drug is quickly withdrawn.[2]
In clinical trials, dizziness, somnolence, vertigo, aggression, anger, loss of coordination, blurred vision, irritability, and slurred speech were the side effects that most commonly led people to leave the trial.[2]
Perampanel is liable to be abused; very high doses produced euphoria responses similar to ketamine, although subjects liked it less and had experienced it more negatively than ketamine; it produced dissociative effects similar to ketamine.[2] It is designated as a Schedule III controlled substance by the Drug Enforcement Administration.[2] A study of dependence in rats found withdrawal symptoms when the drug was removed; dependence in humans wasn't studied well enough to make generalizations as of April 2016.[2] There is limited experience with overdose.[2]
Pharmacology
Perampanel is a selective non-competitive antagonist of AMPA receptors, the major subtype of ionotropic glutamate receptors.[8][9] It was the first drug of this class approved for epilepsy.[4]
Whole-cell voltage clamp studies have demonstrated that perampanel is a negative allosteric AMPA receptor antagonist.[10] Perampanel caused a slow (τ∼1 s at 3 μM), concentration-dependent inhibition of AMPA receptor currents. The rates of block and unblock of AMPA receptor currents were 1.5 × 105 M−1 s−1 and 0.58 s−1, respectively. Perampanel did not affect NMDA receptor currents. The extent of block (IC50, 0.56 μM) was similar at all agonist concentrations, demonstrating a noncompetitive blocking action. Parampanel did affect AMPA receptor desensitization, or the ratio of peak to late response to rapid application of AMPA.[10] Perampanel is a selective negative allosteric AMPA receptor antagonist of high-affinity and slow blocking kinetics, and is not use-dependent.
Perampanel has a prolonged terminal half-life in humans of approximately 105 hours. The drug is 95% bound to plasma protein. Its primary route of metabolism is by CYP3A4. It does not induce P450 enzymes. About 70% of the dose is excreted in the feces and 30% in the urine; less than 2% of the dose is excreted unchanged into the urine.[5]
Chemistry
Perampanel's chemical formula is 2-(2-oxo-1-phenyl-5-pyridin-2-yl-1,2-dihydropyridin-3-yl)benzonitrile; it has a bipyridine core structure that sets it apart from other AMPA receptor antagonists.[9]
The tablets contain lactose monohydrate, low substituted hydroxypropyl cellulose, povidone, microcrystalline cellulose, magnesium stearate, hypromellose, polyethylene glycol, talc, and titanium dioxide in addition to the API; the oral suspension contains sorbitol, microcrystalline cellulose, carboxymethylcellulose sodium, poloxamer, simethicone, citric acid, sodium benzoate and purified water in addition to the API.[2]
History
It was approved for marketing under the brand name Fycompa by the European Medicines Agency in July 2012[5] and as of July 2016 was approved as an adjunct treatment of partial-onset seizures with or without secondarily generalised seizures in people with epilepsy older than 12 and as an adjunct treatment of primary generalised tonic-clonic seizures for people older than 12 years who have idiopathic generalised epilepsy.[5]
It was first approved by the FDA under the same brand name in October 2012 and then in June 2015 for the same uses as those in Europe; it was one of four new drugs for epilepsy approved between 2010 and 2016, along with clobazam (Onfi), ezogabine (Potiga), and eslicarbazepine (Aptiom).[4]
Research
As of August 2016 perampanel had been studied and development discontinued in migraine, multiple sclerosis, neuropathic pain, and Parkinson's disease[6]
References
- Yang, X; Wu T-C; Yuxin Men A; Lee J-Y; Bhattaram VA; Mehta MU. "U.S. FDA Clinical Pharmacology Review. Fycompa (perampanel)" (PDF): 25. Cite journal requires
|journal=(help) - FDA Fycompa Label Tablets and Oral Suspension Label updated April 2016, accessed August 2016
- Besag, FM; Patsalos, PN (2016). "Clinical efficacy of perampanel for partial-onset and primary generalized tonic-clonic seizures". Neuropsychiatric Disease and Treatment. 12: 1215–20. doi:10.2147/NDT.S83842. PMC 4876101. PMID 27274257.
- Chong, DJ; Lerman, AM (April 2016). "Practice Update: Review of Anticonvulsant Therapy". Current Neurology and Neuroscience Reports. 16 (4): 39. doi:10.1007/s11910-016-0640-y. PMID 26984292.
- EMA Summary of Product Characteristics. "Index pagel".
- "Perampanel". AdisInsight. Retrieved August 29, 2016.
- Institute for Quality and Efficiency in Health Care (Germany) (13 August 2014). "Perampanel -- Benefit Assessment According to §35a Social Code Book V [Internet]" (PDF). Extract of Dossier Assessment No. A14-16. IQWiG Dossier Assessment Extracts. PMID 26677496.
- Rogawski, M. A. (2011). "Revisiting AMPA Receptors as an Antiepileptic Drug Target". Epilepsy Currents. 11 (2): 56–63. doi:10.5698/1535-7511-11.2.56. PMC 3117497. PMID 21686307.
- Rogawski, MA; Hanada, T (2013). "Preclinical pharmacology of perampanel, a selective non-competitive AMPA receptor antagonist". Acta Neurologica Scandinavica Supplementum. 127 (197): 19–24. doi:10.1111/ane.12100. PMC 4506647. PMID 23480152.
- Chen CY, Matt L, Hell JW, Rogawski MA (Sep 17, 2014). "Perampanel inhibition of AMPA receptor currents in cultured hippocampal neurons". PLOS ONE. 9 (9): e108021. doi:10.1371/journal.pone.0108021. PMC 4168215. PMID 25229608.