Bumetanide
Bumetanide, sold under the trade name Bumex among others, is a medication used to treat swelling and high blood pressure.[1] This include swelling as a result of heart failure, liver failure, or kidney problems.[1] It may work for swelling when other medications have not.[1] For high blood pressure it is not a preferred treatment.[1] It is taken by mouth, or by injection into a vein or muscle.[1] Effects generally begin within an hour and lasts for about six hours.[1]
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Bumex, Burinex, others |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a684051 |
| Pregnancy category | |
| Routes of administration | By mouth, intravenous, intramuscular |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | Almost complete (~80%) |
| Protein binding | 97% |
| Metabolism | Liver |
| Elimination half-life | ~0.8 hours |
| Excretion | Kidney |
| Identifiers | |
IUPAC name
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.044.534 |
| Chemical and physical data | |
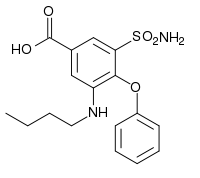
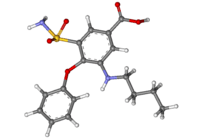
| Formula | C17H20N2O5S |
| Molar mass | 364.417 g/mol g·mol−1 |
| 3D model (JSmol) | |
SMILES
| |
InChI
| |
| (verify) | |
Common side effects include dizziness, low blood pressure, low blood potassium, muscle cramps, and kidney problems.[1] Other serious side effects may include hearing loss and low blood platelets.[1] People with a sulfa allergy, may also be allergic to bumetanide.[1] Blood tests are recommended regularly for those on treatment.[1] Safety during pregnancy and breastfeeding is unclear.[2] Bumetanide is a loop diuretic and works by decreasing the reabsorption of sodium by the kidneys.[3][1]
Bumetanide was patented in 1968 and came into medical use in 1972.[4] It is available as a generic medication.[3] A month supply in the United Kingdom costs the NHS about 1.20 £ as of 2019.[3] In the United States the wholesale cost of this amount is about US$12.[5] In 2016 it was the 266th most prescribed medication in the United States with more than a million prescriptions.[6]
Uses
Medical uses
It used to treat swelling and high blood pressure.[1] This include swelling as a result of heart failure, liver failure, or kidney problems.[1] For high blood pressure it is not a preferred treatment.[1] It is taken by mouth, or by injection into a vein or muscle.[1]
Other uses
It 2008, ESPN reported that four NFL players were being suspended under the steroid policy as a result of taking bumetanide.[7] It is sometimes used for weight loss because, as a diuretic, it removes water, but it also masks other drugs, including steroids, by diluting the contents of the user's urine, yielding a lower concentration of filtered substances, which makes them less likely to be detected.
Bumetanide was an undisclosed active ingredient in the over-the-counter weight loss supplement StarCaps, which was removed from the market after its presence was discovered by the United States Food and Drug Administration.[8]
Side effects
Common side effects include dizziness, low blood pressure, low blood potassium, muscle cramps, and kidney problems.[1] Other serious side effects may include hearing loss and low blood platelets.[1] People with a sulfa allergy, may also be allergic to bumetanide.[1] Blood tests are recommended regularly for those on treatment.[1] Safety during pregnancy and breastfeeding is unclear.[2]
Mechanism of action
Bumetanide is a loop diuretic and works by decreasing the reabsorption of sodium by the kidneys. The main difference between bumetanide and furosemide is in their bioavailability and potency. About 60% of furosemide is absorbed in the intestine, and there are substantial inter- and intraindividual differences in bioavailability (range 10-90%). About 80% of bumetanide is absorbed, and its absorption does not change when it is taken with food. It is said to be a more predictable diuretic, meaning that the predictable absorption is reflected in a more predictable effect.[9] Bumetanide is 40 times more potent than furosemide for people with normal renal function.[9]
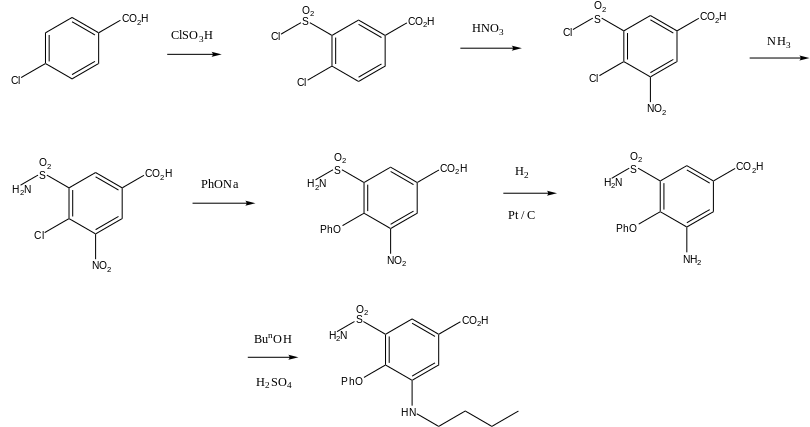
Synthesis
Bumetanide, 3-butylamino-4-phenoxy-5-sulfamoylbenzoic acid, is synthesized from 4-chlorobenzoic acid. In the first stage of synthesis, it undergoes sulfonylchlorination by chlorosulfonic acid, forming 4-chloro-3-chlorosulfonylbenzoic acid, which is further nitrated with nitric acid to 4-chloro-3-chlorosulfonyl-5-nitrobenzoic acid. Reacting this with ammonia gives 5-aminosulfonyl-4-chloro-3-nitrobenzoic acid, which when reacted with sodium phenolate is transformed into 5-amino-sulfonyl-3-nitro-5-phenoxybenzoid acid. Reduction of the nitro group in this product by hydrogen using a palladium on carbon catalyst gives 3-amino-5-aminosulfonyl- 5-phenoxybenzoic acid. Finally, reacting this with butyl alcohol in the presence of sulfuric acid gives the desired bumetanide.
Research
In the brain, bumetanide blocks the NKCC1 cation-chloride co-transporter, and thus decreases internal chloride concentration in neurons. In turn, this concentration change makes the action of GABA more hyperpolarizing, which may be useful for treatment of neonatal seizures, which quite often are not responsive to traditional GABA-targeted treatment, such as barbiturates. Bumetanide is therefore under evaluation as a prospective antiepileptic drug.[15]
References
- "Bumetanide Monograph for Professionals". Drugs.com. American Society of Health-System Pharmacists. Retrieved 8 April 2019.
- "Bumetanide (Bumex) Use During Pregnancy". Drugs.com. Retrieved 8 April 2019.
- British national formulary : BNF 76 (76 ed.). Pharmaceutical Press. 2018. pp. 225–226. ISBN 9780857113382.
- Fischer, Jnos; Ganellin, C. Robin (2006). Analogue-based Drug Discovery. John Wiley & Sons. p. 458. ISBN 9783527607495.
- "NADAC as of 2019-02-27". Centers for Medicare and Medicaid Services. Retrieved 3 March 2019.
- "The Top 300 of 2019". clincalc.com. Retrieved 22 December 2018.
- "McAllister, Smith, Grant, Texans' Pittman among players testing positive". ESPN.com. ESPN. October 26, 2008. Retrieved June 6, 2017.
- "Food and Drug Administration Office of Criminal Investigations – U.S. Department of Justice Press Release – Pills Sold Throughout the United States Contained an Undisclosed Prescription Drug Banned By the National Football League". fda.gov. United States Food and Drug Administration. March 26, 2014. Retrieved June 6, 2017.
- Brunton, Laurence; Lazo, John S.; Parker, Keith L., eds. (2006). Goodman & Gilman's The Pharmacological Basis of Therapeutics (11th ed.). New York: McGraw-Hill. pp. 749–753. ISBN 0-07-142280-3.
- Loevens Kemiske Fabrik Produktionsaktieselskab (Jul 9, 1970). "Neue Sulfamylbenzoesaeurederivate". DPMAregister (in German). Ger. Pat. 19 64 503.5: German Patent and Trade Mark Office. Retrieved 20 June 2018.
- Loevens Kemiske Fabrik Produktionsaktieselskab (Jul 9, 1970). "Arzneimittelzubereitung mit einem Gehalt an 3-Butylamino-4-phenoxy-5-sulfamylbenzoesaeure und deren Salzen". DPMAregister (in German). Ger. Pat. 19 64 504.6: German Patent and Trade Mark Office. Retrieved 20 June 2018.
- Feit, P. W. (1971). "Aminobenzoic acid diuretics. 2. 4-Substituted-3-amino-5-sulfamoylbenzoic acid derivatives". Journal of Medicinal Chemistry. 14 (5): 432–9. doi:10.1021/jm00287a014. PMID 5117690.
- Feit, Peter Werner (11 January 1972). "Pharmaceutical composition for the treatment of oedematous conditions and hypertension" (PDF). US Pat. 3634583A: Leo Pharmaceutical Products Ltd AS. Retrieved 20 June 2018.
- Feit, Peter Werner; Nielsen, Ole Bent Tvaermose; Bruun, Herta; Bretting, Claus Aage Svensgaard (4 April 1978). "Sulphonamides, compositions containing the same and methods for using the same in the treatment of hypertension or odemeas" (PDF). US Pat. US4082851A: Leo Pharmaceutical Products Ltd AS. Retrieved 20 June 2018.
- Löscher W, Puskarjov M, Kaila K (June 2013). "Cation-chloride cotransporters NKCC1 and KCC2 as potential targets for novel antiepileptic and antiepileptogenic treatments". Neuropharmacology. 69: 62–74. doi:10.1016/j.neuropharm.2012.05.045. PMID 22705273.