Sevoflurane
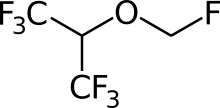
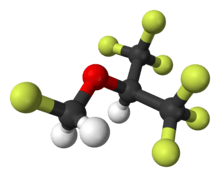
Sevoflurane is a sweet-smelling, nonflammable, highly fluorinated methyl isopropyl ether used as an inhalational anaesthetic for induction and maintenance of general anesthesia. After desflurane, it is the volatile anesthetic with the fastest onset and offset.[1]
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Sojourn, Ultane, Sevorane |
| AHFS/Drugs.com | Consumer Drug Information |
| Pregnancy category | |
| Routes of administration | inhaled |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Metabolism | Hepatic by CYP2E1 |
| Metabolites | Hexafluoroisopropanol |
| Elimination half-life | 15–23 hours |
| Excretion | Renal |
| Identifiers | |
IUPAC name
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.171.146 |
| Chemical and physical data | |
| Formula | C4H3F7O |
| Molar mass | 200.055 g/mol g·mol−1 |
| 3D model (JSmol) | |
| Boiling point | 58.5 °C (137.3 °F) |
SMILES
| |
InChI
| |
| | |
Medical uses
It is one of the most commonly used volatile anesthetic agents, particularly for outpatient anesthesia,[2] across all ages, as well as in veterinary medicine. Together with desflurane, sevoflurane is replacing isoflurane and halothane in modern anesthesiology. It is often administered in a mixture of nitrous oxide and oxygen.
Sevoflurane has an excellent safety record,[2] but is under review for potential neurotoxicity, especially relevant to administration in infants and children, and rare reports similar to halothane hepatotoxicity.[2] Sevoflurane is the preferred agent for mask induction due to its lesser irritation to mucous membranes.
Sevoflurane was discovered by Ross Terrell[3] and independently by Bernard M Regan. A detailed report of its development and properties appeared in 1975 in a paper authored by Richard Wallin, Bernard Regan, Martha Napoli and Ivan Stern. It was introduced into clinical practice initially in Japan in 1990 by Maruishi Pharmaceutical Co., Ltd. Osaka, Japan. The rights for sevoflurane worldwide were held by AbbVie. It is now available as a generic drug.
Sevoflurane is an inhaled anaesthetic that is often used to put children asleep for surgery.[4] During the process of waking up from the medication, it has been known to cause agitation and delirium.[4] It is not clear if this can be prevented.[4]
Adverse effects
Studies examining a current significant health concern, anesthetic-induced neurotoxicity (including with sevoflurane, and especially with children and infants) are "fraught with confounders, and many are underpowered statistically", and so are argued to need "further data... to either support or refute the potential connection".[5]
Concern regarding the safety of anaesthesia is especially acute with regard to children and infants, where preclinical evidence from relevant animal models suggest that common clinically important agents, including sevoflurane, may be neurotoxic to the developing brain, and so cause neurobehavioural abnormalities in the long term; two large-scale clinical studies (PANDA and GAS) were ongoing as of 2010, in hope of supplying "significant [further] information" on neurodevelopmental effects of general anaesthesia in infants and young children, including where sevoflurane is used.[6]
Pharmacology
The exact mechanism of the action of general anaesthetics has not been delineated.[7] Sevoflurane acts as a positive allosteric modulator of the GABAA receptor in electrophysiology studies of neurons and recombinant receptors.[8][9][10][11] However, it also acts as an NMDA receptor antagonist,[12] potentiates glycine receptor currents,[11] and inhibits nAChR[13] and 5-HT3 receptor currents.[14][15][16]
Physical properties
| Boiling point: | 58.6 °C | (at 101.325 kPa) | |
| Density: | 1.517–1.522 g/cm³ | (at 20 °C) | |
| MAC : | 2.1 vol % | ||
| Molecular weight: | 200 u | ||
| Vapor pressure: | 157 mmHg (20.9 kPa) | (at 20 °C) | |
| 197 mmHg (26.3 kPa) | (at 25 °C) | ||
| 317 mmHg (42.3 kPa) | (at 36 °C) | ||
| Blood:Gas partition coefficient: | 0.68 | ||
| Oil:Gas partition coefficient: | 47 |
References
- Sakai EM, Connolly LA, Klauck JA (December 2005). "Inhalation anesthesiology and volatile liquid anesthetics: focus on isoflurane, desflurane, and sevoflurane". Pharmacotherapy. 25 (12): 1773–88. doi:10.1592/phco.2005.25.12.1773. PMID 16305297.
- Livertox: Clinical and Research Information on Drug-Induced Liver Injury (2014) "Drug Record: Sevoflurane", U.S. National Library of Medicine, 2 July 2014 update, see , accessed 15 August 2014.
- Burns WB, Eger EI (August 2011). "Ross C. Terrell, PhD, an anesthetic pioneer". Anesthesia and Analgesia. 113 (2): 387–9. doi:10.1213/ane.0b013e3182222b8a. PMID 21642612.
- Costi D, Cyna AM, Ahmed S, Stephens K, Strickland P, Ellwood J, et al. (September 2014). "Effects of sevoflurane versus other general anaesthesia on emergence agitation in children". The Cochrane Database of Systematic Reviews. 9 (9): CD007084. doi:10.1002/14651858.CD007084.pub2. PMID 25212274.
- Vlisides P, Xie Z (2012). "Neurotoxicity of general anesthetics: an update". Current Pharmaceutical Design. 18 (38): 6232–40. doi:10.2174/138161212803832344. PMID 22762477.
- Sun L (December 2010). "Early childhood general anaesthesia exposure and neurocognitive development". British Journal of Anaesthesia. 105 Suppl 1 (Suppl 1): i61–8. doi:10.1093/bja/aeq302. PMC 3000523. PMID 21148656.
- Perkins B (7 February 2005). "How does anesthesia work?". Scientific American. Retrieved 30 June 2016.
- Jenkins A, Franks NP, Lieb WR (February 1999). "Effects of temperature and volatile anesthetics on GABA(A) receptors". Anesthesiology. 90 (2): 484–91. doi:10.1097/00000542-199902000-00024. PMID 9952156.
- Wu J, Harata N, Akaike N (November 1996). "Potentiation by sevoflurane of the gamma-aminobutyric acid-induced chloride current in acutely dissociated CA1 pyramidal neurones from rat hippocampus". British Journal of Pharmacology. 119 (5): 1013–21. doi:10.1111/j.1476-5381.1996.tb15772.x. PMC 1915958. PMID 8922750.
- Krasowski MD, Harrison NL (February 2000). "The actions of ether, alcohol and alkane general anaesthetics on GABAA and glycine receptors and the effects of TM2 and TM3 mutations". British Journal of Pharmacology. 129 (4): 731–43. doi:10.1038/sj.bjp.0703087. PMC 1571881. PMID 10683198.
- Schüttler J, Schwilden H (8 January 2008). Modern Anesthetics. Springer Science & Business Media. pp. 32–. ISBN 978-3-540-74806-9.
- Brosnan RJ, Thiesen R (June 2012). "Increased NMDA receptor inhibition at an increased Sevoflurane MAC". BMC Anesthesiology. 12 (1): 9. doi:10.1186/1471-2253-12-9. PMC 3439310. PMID 22672766.
- Christa J. Van Dort (2008). Regulation of Arousal by Adenosine A(1) and A(2A) Receptors in the Prefrontal Cortex of C57BL/6J Mouse. ProQuest. pp. 120–. ISBN 978-0-549-99431-2.
- Schüttler J, Schwilden H (8 January 2008). Modern Anesthetics. Springer Science & Business Media. pp. 74–. ISBN 978-3-540-74806-9.
- Suzuki T, Koyama H, Sugimoto M, Uchida I, Mashimo T (March 2002). "The diverse actions of volatile and gaseous anesthetics on human-cloned 5-hydroxytryptamine3 receptors expressed in Xenopus oocytes". Anesthesiology. 96 (3): 699–704. doi:10.1097/00000542-200203000-00028. PMID 11873047.
- Hang LH, Shao DH, Wang H, Yang JP (2010). "Involvement of 5-hydroxytryptamine type 3 receptors in sevoflurane-induced hypnotic and analgesic effects in mice" (PDF). Pharmacological Reports. 62 (4): 621–6. CiteSeerX 10.1.1.587.5552. doi:10.1016/s1734-1140(10)70319-4. PMID 20885002.
Further reading
- Patel SS, Goa KL (April 1996). "Sevoflurane. A review of its pharmacodynamic and pharmacokinetic properties and its clinical use in general anaesthesia". Drugs. 51 (4): 658–700. doi:10.2165/00003495-199651040-00009. PMID 8706599.
Haria M, Bryson HM, Goa KL, Patel SS (August 1996). "Erratum". Drugs. 52 (2): 253. doi:10.1007/bf03257493. - Wallin RF, Regan BM, Napoli MD, Stern IJ (Nov–Dec 1975). "Sevoflurane: a new inhalational anesthetic agent". Anesthesia and Analgesia. 54 (6): 758–66. doi:10.1213/00000539-197511000-00021. PMID 1239214.