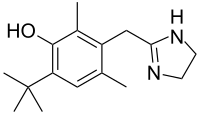
Oxymetazoline
Oxymetazoline is a selective α1 adrenergic receptor agonist and α2 adrenergic receptor partial agonist. It is a topical decongestant, used in the form of oxymetazoline hydrochloride. It was developed from xylometazoline at E. Merck Darmstadt by Fruhstorfer in 1961.[1] Oxymetazoline is generally available as a nasal spray.
 | |
| Clinical data | |
|---|---|
| Trade names | Afrin, Ocuclear, Drixine |
| AHFS/Drugs.com | Monograph |
| Pregnancy category |
|
| Dependence liability | Moderate |
| Routes of administration | Intranasal |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Metabolism | Kidney (30%), fecal (10%) |
| Elimination half-life | 5–6 hours |
| Identifiers | |
IUPAC name
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.014.618 |
| Chemical and physical data | |
| Formula | C16H24N2O |
| Molar mass | 260.381 g·mol−1 |
| 3D model (JSmol) | |
| Melting point | 301.5 °C (574.7 °F) |
SMILES
| |
InChI
| |
| | |
Medical uses
Oxymetazoline is available over-the-counter as a topical decongestant in the form of oxymetazoline hydrochloride in nasal sprays such as Otrivin, Afrin, Operil, Dristan, Dimetapp, Oxyspray, Facimin, Nasivin, Nostrilla, Utabon, Sudafed OM, Vicks Sinex, Zicam, SinuFrin, Drixoral[2] and Mucinex Full Force.[3]
In the United States, oxymetazoline 1% cream is approved by the Food and Drug Administration for topical treatment of persistent facial erythema (redness) associated with rosacea in adults.[4]
Due to its vasoconstricting properties, oxymetazoline is also used to treat nose bleeds[5][6] and eye redness due to minor irritation (marketed as Visine L.R. in the form of eye drops). [7]
Side effects and special considerations
Rebound congestion
Rebound congestion, or rhinitis medicamentosa, may occur. A 2006 review of the pathology of rhinitis medicamentosa concluded that use of oxymetazoline for more than three days may result in rhinitus medicamentosa and recommended limiting use to three days.[8] In a submission to the Therapeutic Goods Administration, a Novartis representative concluded, "The justification was not based on evidence." Citing an existing extensive body of evidence and noting a range of recommended periods from ten to five days, Novartis recommended the established five day period for its use for self-medication without medical consultation as it coincides with the typical duration of the common cold. [9]
Use in pregnancy
The Food and Drug Administration places oxymetazoline in category C, indicating risk to the fetus cannot be ruled out. While it has been shown that a single dose does not significantly alter either maternal or fetal circulation,[10] this subject has not been studied extensively enough to draw reliable conclusions.
Overdose
If accidentally ingested, standard methods to remove unabsorbed drugs should be considered. There is no specific antidote for oxymetazoline, although its pharmacological effects may be reversed by α adrenergic antagonists such as phentolamine. In the event of a possibly life-threatening overdose (such as a hypertensive crisis), benzodiazepines should be considered to decrease the likelihood of seizures and convulsions, as well as reduce anxiety and to lower blood pressure. In children, oxymetazoline may produce profound central nervous system depression due to stimulation of central α2 receptors and imidazoline receptors, much like clonidine.
Pharmacology
Pharmacodynamics
Oxymetazoline is a sympathomimetic that selectively agonizes α1 and, partially, α2 adrenergic receptors.[11] Since vascular beds widely express α1 receptors, the action of oxymetazoline results in vasoconstriction. In addition, the local application of the drug also results in vasoconstriction due to its action on endothelial postsynaptic α2 receptors; systemic application of α2 agonists, in contrast, causes vasodilation because of centrally-mediated inhibition of sympathetic tone via presynaptic α2 receptors.[12] Vasoconstriction of vessels results in relief of nasal congestion in two ways: first, it increases the diameter of the airway lumen; second, it reduces fluid exudation from postcapillary venules.[13] It can reduce nasal airway resistance (NAR) up to 35.7% and reduce nasal mucosal blood flow up to 50%.[14]
Pharmacokinetics
Imidazolines are sympathomimetic agents, with primary effects on α adrenergic receptors and little if any effect on β adrenergic receptors. Oxymetazoline is readily absorbed orally. Effects on α receptors from systemically absorbed oxymetazoline hydrochloride may persist for up to 7 hours after a single dose. The elimination half-life in humans is 5–8 hours. It is excreted unchanged both by the kidneys (30%) and in feces (10%).
History
The oxymetazoline brand Afrin was first sold as a prescription medication in 1966. After finding substantial early success as a prescription medication, it became available as an over-the-counter drug in 1975. Schering-Plough did not engage in heavy advertising until 1986.[15]
From the mid 1980s to mid 1990s, the brand Sinex was featured in many television advertisements. Some of these commercials showed men, women, and children using other brands of nasal sprays, and then standing upside down on a sidewalk, or against a wall, etc or hanging upside down from various playground equipment to prevent their nasal spray from dripping out. This was juxtaposed with Sinex users not having to hang upside side down or stand on their heads as it didn't drip out.
Society and culture
Brand names
Brand names include Afrin, Drixine, Dristan, Nasivin, Nasivion, Nezeril, Nostrilla, Logicin, Vicks Sinex, Visine L.R., Sudafed OM, Zicam, Otrivin Oxy, SinuFrin and Mucinex Sinus-Max.
References
- German Patent 1,117,588
- "Drixoral Decongestant Nasal Spray". Bayer. Retrieved 18 November 2017.
- "Oxymetazoline: Drug Information Provided by Lexi-Comp: Merck Manual Professional". Merck.com. Retrieved 15 April 2013.
- Patel NU, Shukla S, Zaki J, Feldman SR (October 2017). "Oxymetazoline hydrochloride cream for facial erythema associated with rosacea". Expert Review of Clinical Pharmacology. 10 (10): 1049–1054. doi:10.1080/17512433.2017.1370370. PMID 28837365.
- Katz RI, Hovagim AR, Finkelstein HS, Grinberg Y, Boccio RV, Poppers PJ (1990). "A comparison of cocaine, lidocaine with epinephrine, and oxymetazoline for prevention of epistaxis on nasotracheal intubation". Journal of Clinical Anesthesia. 2 (1): 16–20. doi:10.1016/0952-8180(90)90043-3. PMID 2310576.
- Krempl GA, Noorily AD (September 1995). "Use of oxymetazoline in the management of epistaxis". The Annals of Otology, Rhinology, and Laryngology. 104 (9 Pt 1): 704–6. doi:10.1177/000348949510400906. PMID 7661519.
- "VISINE® Original Red Eye Drops | VISINE products". Visine.com. Retrieved 15 April 2013.
- Ramey JT, Bailen E, Lockey RF (2006). "Rhinitis medicamentosa". Journal of Investigational Allergology & Clinical Immunology. 16 (3): 148–55. PMID 16784007.
- Nguyen, Tra-My (2014). "Consultation submission: OTC nasal decongestant preparations for topical use: proposed advisory statements for medicines" (PDF). Novartis Consumer Health Australasia.
- Rayburn WF, Anderson JC, Smith CV, Appel LL, Davis SA (August 1990). "Uterine and fetal Doppler flow changes from a single dose of a long-acting intranasal decongestant". Obstetrics and Gynecology. 76 (2): 180–2. PMID 2196495.
- Westfall Thomas C, Westfall David P, "Chapter 6. Neurotransmission: The Autonomic and Somatic Motor Nervous Systems" (Chapter). Brunton LL, Lazo JS, Parker KL: Goodman & Gilman's The Pharmacological Basis of Therapeutics, 11e: "Archived copy". Archived from the original on 30 September 2011. Retrieved 24 January 2015.CS1 maint: archived copy as title (link).
- Biaggioni I, Robertson D. "Chapter 9. Adrenoceptor Agonists & Sympathomimetic Drugs". In Katzung BG (ed.). Basic & Clinical Pharmacology (11th ed.). Archived from the original on 30 September 2011. Retrieved 30 November 2011.
- Widdicombe J (1997). "Microvascular anatomy of the nose". Allergy. 52 (40 Suppl): 7–11. doi:10.1111/j.1398-9995.1997.tb04877.x. PMID 9353554.
- Bende M, Löth S (March 1986). "Vascular effects of topical oxymetazoline on human nasal mucosa". The Journal of Laryngology and Otology. 100 (3): 285–8. doi:10.1017/S0022215100099151. PMID 3950497.
- Dougherty, Phillip H. (20 October 1986). "Advertising; Afrin Goes After Users Of Nasal Decongestants". The New York Times. The New York Times Company. Retrieved 30 March 2015.