Dexmedetomidine
Dexmedetomidine, sold under the trade name Precedex among others, is an anxiety reducing, sedative, and pain medication. Dexmedetomidine is notable for its ability to provide sedation without risk of respiratory depression (unlike other commonly used drugs such as propofol and fentanyl) and can provide cooperative or semi-rousable sedation.
 | |
| Clinical data | |
|---|---|
| Trade names | Precedex, Dexdor, Dexdomitor, Sileo |
| AHFS/Drugs.com | Monograph |
| License data | |
| Pregnancy category |
|
| Routes of administration | Intravenous infusion Transmucosal |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Protein binding | 94% |
| Metabolism | Near complete hepatic metabolism to inactive metabolites |
| Elimination half-life | 2 hours |
| Excretion | Urinary |
| Identifiers | |
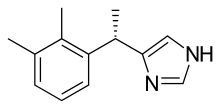
IUPAC name
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| ECHA InfoCard | 100.119.391 |
| Chemical and physical data | |
| Formula | C13H16N2 |
| Molar mass | 200.28 g/mol g·mol−1 |
| 3D model (JSmol) | |
SMILES
| |
InChI
| |
| (verify) | |
Similar to clonidine, it is an agonist of α2-adrenergic receptors in certain parts of the brain.[1] Dexmedetomidine hydrochloride is also used in veterinary medicine for dogs and cats.[2] It was developed by Orion Pharma.
Medical uses
Intensive care unit sedation
Dexmedetomidine is most often used in the intensive care setting for light to moderate sedation. It is not recommended for long-term deep sedation. A feature of dexmedetomidine is that it has analgesic properties in addition to its role as a hypnotic, but is opioid sparing; thus, it is not associated with significant respiratory depression (unlike propofol).
Many studies suggest dexmedetomidine for sedation in mechanically ventilated adults may reduce time to extubation and ICU stay.[3][4] People on dexmedetomidine can be rousable and cooperative, a benefit in some procedures.
Compared with other sedatives, some studies suggest dexmedetomidine may be associated with less delirium.[5] However, this finding is not consistent across multiple studies.[4] At the very least, when aggregating many study results together, use of dexmedetomidine appears to be associated with less neurocognitive dysfunction compared to other sedatives.[6] Whether this observation has a beneficial psychological impact is unclear.[5] From an economic perspective, dexmedetomidine is associated with lower ICU costs, largely due to a shorter time to extubation.[7]
Procedural sedation
Dexmedetomidine can also be used for procedural sedation such as during colonoscopy.[8] It can be used as an adjunct with other sedatives like benzodiazepines, opioids, and propofol to enhance sedation and help maintain hemodynamic stability by decreasing the requirement of other sedatives.[9][10] Dexmedetomidine is also used for procedural sedation in children.[11]
There is weak evidence that it can be used for sedation required for awake fibreoptic nasal intubation in patients with a difficult airway[12]
Other
Dexmedetomidine may be useful for the treatment of the negative cardiovascular effects of acute amphetamines and cocaine intoxication and overdose.[13][14]
Dosage and administration
Intravenous infusion of dexmedetomidine is commonly initiated with a loading dose followed by a maintenance infusion. There may be great individual variability in the hemodynamic effects (especially on heart rate and blood pressure), as well as the sedative effects of this drug. For this reason, the dose must be carefully adjusted to achieve the desired clinical effect.[15]
Side effects
There is no absolute contraindication to the use of dexmedetomidine. It has a biphasic effect on blood pressure with lower readings at lower drug concentrations and higher readings at higher concentrations.[16] Rapid IV administration or bolus has been associated with hypertension due to peripheral α2-receptor stimulation. Bradycardia can be limiting factor with infusions especially in higher doses.
Interactions
Dexmedetomidine may enhance the effects of other sedatives and anesthetics when co-administered. Similarly, drugs that lower blood pressure and heart rate, such as beta blockers, may also have enhanced effects when co-administered with dexmedetomidine.[17]
Pharmacology
Pharmacodynamics
Dexmedetomidine is a highly selective α2-adrenergic agonist. Unlike opioids and other sedatives such as propofol, dexmedetomidine is able to achieve its effects without causing respiratory depression. Dexmedetomidine induces sedation by decreasing activity of noradrenergic neurons in the locus ceruleus in the brain stem, thereby increasing the activity of inhibitory gamma-aminobutyric acid (GABA) neurons in the ventrolateral preoptic nucleus.[18] In contrast, other sedatives like propofol and benzodiazepines directly increase activity of gamma-aminobutyric acid neurons.[19] Sedation by dexmedetomidine mirrors natural sleep.[20] As such, dexmedetomidine provides less amnesia than benzodiazepines.[19] Dexmedetomidine also has analgesic effects at the spinal cord level and other supraspinal sites.[19] Thus, unlike other hypnotic agents like propofol, dexmedetomidine can be used as an adjunct medication to help decrease the opioid requirements of people in pain while still providing similar analgesia.
Pharmacokinetics
Intravenous dexmedetomidine exhibits linear pharmacokinetics with a rapid distribution half-life of approximately 6 minutes and a terminal elimination half-life of approximately 2 hours. Plasma protein binding of dexemedotomindine is about 94% (mostly albumin).[21]
Dexmedetomidine is metabolized by the liver via glucuronidation and cytochrome P450. As such, it should be used with caution in people with liver disease.[17]
The majority of metabolized dexmedetomidine is excreted in the urine (~95%).
History
Dexmedetomidine was approved in 1999 by the US Food and Drug Administration (FDA) as a short-term sedative and analgesic (<24 hours) for critically ill or injured people on mechanical ventilation in the intensive care unit (ICU). The rationale for its short-term use was due to concerns over withdrawal side effects such as rebound high blood pressure. These effects have not been consistently observed in research studies, however.[22] In 2008 the FDA expanded its indication to include non-intubated people requiring sedation for surgical or non-surgical procedures, such as colonoscopy.
Veterinary use
Dexmedetomidine, under the trade name Dexdomitor (Orion Corporation), was approved in the European Union in for use in cats and dogs in 2002 for sedation and induction of general anesthesia.[23] The FDA approved dexmedetomidine for use in dogs in 2006 and cats in 2007.[24]
In 2015, the European Medicines Agency and the FDA approved an oromucosal gel form of dexmedetomidine marketed as Sileo (Zoetis) for use in dogs for relief of noise aversion.[25][26]
References
- Cormack JR, Orme RM, Costello TG (2005). "The role of alpha2-agonists in neurosurgery". Journal of Clinical Neuroscience. 12 (4): 375–8. doi:10.1016/j.jocn.2004.06.008. PMID 15925765.
- "Archived copy". Archived from the original on 2013-09-27. Retrieved 2013-08-02.CS1 maint: archived copy as title (link)
- Pasin, Laura; Greco, Teresa; Feltracco, Paolo; Vittorio, Annalisa; Neto, Caetano Nigro; Cabrini, Luca; Landoni, Giovanni; Finco, Gabriele; Zangrillo, Alberto (2013-01-01). "Dexmedetomidine as a sedative agent in critically ill patients: a meta-analysis of randomized controlled trials". PLOS ONE. 8 (12): e82913. Bibcode:2013PLoSO...882913P. doi:10.1371/journal.pone.0082913. ISSN 1932-6203. PMC 3877008. PMID 24391726.
- Chen, Ken; Lu, Zhijun; Xin, Yi Chun; Cai, Yong; Chen, Yi; Pan, Shu Ming (2015-01-01). "Alpha-2 agonists for long-term sedation during mechanical ventilation in critically ill patients". The Cochrane Database of Systematic Reviews. 1: CD010269. doi:10.1002/14651858.CD010269.pub2. ISSN 1469-493X. PMC 6353054. PMID 25879090.
- MacLaren, Robert; Preslaski, Candice R.; Mueller, Scott W.; Kiser, Tyree H.; Fish, Douglas N.; Lavelle, James C.; Malkoski, Stephen P. (2015-03-01). "A randomized, double-blind pilot study of dexmedetomidine versus midazolam for intensive care unit sedation: patient recall of their experiences and short-term psychological outcomes". Journal of Intensive Care Medicine. 30 (3): 167–175. doi:10.1177/0885066613510874. ISSN 1525-1489. PMID 24227448.
- Li, Bo; Wang, Huixia; Wu, Hui; Gao, Chengjie (2015-04-01). "Neurocognitive dysfunction risk alleviation with the use of dexmedetomidine in perioperative conditions or as ICU sedation: a meta-analysis". Medicine. 94 (14): e597. doi:10.1097/MD.0000000000000597. ISSN 1536-5964. PMC 4554047. PMID 25860207.
- Turunen, Heidi; Jakob, Stephan M.; Ruokonen, Esko; Kaukonen, Kirsi-Maija; Sarapohja, Toni; Apajasalo, Marjo; Takala, Jukka (2015-01-01). "Dexmedetomidine versus standard care sedation with propofol or midazolam in intensive care: an economic evaluation". Critical Care (London, England). 19: 67. doi:10.1186/s13054-015-0787-y. ISSN 1466-609X. PMC 4391080. PMID 25887576.
- Dere, Kamer; Sucullu, Ilker; Budak, Ersel Tan; Yeyen, Suleyman; Filiz, Ali Ilker; Ozkan, Sezai; Dagli, Guner (2010-07-01). "A comparison of dexmedetomidine versus midazolam for sedation, pain and hemodynamic control, during colonoscopy under conscious sedation". European Journal of Anaesthesiology. 27 (7): 648–652. doi:10.1097/EJA.0b013e3283347bfe. ISSN 1365-2346. PMID 20531094.
- Paris A, Tonner PH (2005). "Dexmedetomidine in anaesthesia". Current Opinion in Anesthesiology. 18 (4): 412–8. doi:10.1097/01.aco.0000174958.05383.d5. PMID 16534267.
- Giovannitti, Joseph A.; Thoms, Sean M.; Crawford, James J. (2015-01-01). "Alpha-2 Adrenergic Receptor Agonists: A Review of Current Clinical Applications". Anesthesia Progress. 62 (1): 31–38. doi:10.2344/0003-3006-62.1.31. ISSN 0003-3006. PMC 4389556. PMID 25849473.
- Ahmed, S. S.; Unland, T; Slaven, J. E.; Nitu, M. E.; Rigby, M. R. (2014). "Successful use of intravenous dexmedetomidine for magnetic resonance imaging sedation in autistic children". Southern Medical Journal. 107 (9): 559–64. doi:10.14423/SMJ.0000000000000160. PMID 25188619.
- He, Xing-Ying; Cao, Jian-Ping; He, Qian; Shi, Xue-Yin (2014-01-19). "Dexmedetomidine for the management of awake fibreoptic intubation". Cochrane Database of Systematic Reviews (1): CD009798. doi:10.1002/14651858.cd009798.pub2. ISSN 1465-1858. PMID 24442817.
- Menon DV, Wang Z, Fadel PJ, Arbique D, Leonard D, Li JL, Victor RG, Vongpatanasin W (2007). "Central sympatholysis as a novel countermeasure for cocaine-induced sympathetic activation and vasoconstriction in humans". J Am Coll Cardiol. 50 (7): 626–33. doi:10.1016/j.jacc.2007.03.060. PMID 17692748.
- John R. Richards; Timothy E. Albertson; Robert W. Derlet; Richard A. Lange; Kent R. Olson; B. Zane Horowitz (February 2015). "Treatment of toxicity from amphetamines, related derivatives, and analogues: A systematic clinical review". Drug and Alcohol Dependence. 150: 1–13. doi:10.1016/j.drugalcdep.2015.01.040. PMID 25724076.
- "Dosing Guidelines for Precedex" (PDF). Archived from the original (PDF) on 2011-07-15. Retrieved 2010-11-21.
- Ebert, T. J.; Hall, J. E.; Barney, J. A.; Uhrich, T. D.; Colinco, M. D. (2000-08-01). "The effects of increasing plasma concentrations of dexmedetomidine in humans". Anesthesiology. 93 (2): 382–394. doi:10.1097/00000542-200008000-00016. ISSN 0003-3022. PMID 10910487.
- Keating, Gillian M. (2015-07-01). "Dexmedetomidine: A Review of Its Use for Sedation in the Intensive Care Setting". Drugs. 75 (10): 1119–1130. doi:10.1007/s40265-015-0419-5. ISSN 0012-6667. PMID 26063213.
- Nelson, Laura E.; Lu, Jun; Guo, Tianzhi; Saper, Clifford B.; Franks, Nicholas P.; Maze, Mervyn (2003-02-01). "The alpha2-adrenoceptor agonist dexmedetomidine converges on an endogenous sleep-promoting pathway to exert its sedative effects". Anesthesiology. 98 (2): 428–436. doi:10.1097/00000542-200302000-00024. ISSN 0003-3022. PMID 12552203.
- Panzer, Oliver; Moitra, Vivek; Sladen, Robert N. (2009-07-01). "Pharmacology of sedative-analgesic agents: dexmedetomidine, remifentanil, ketamine, volatile anesthetics, and the role of peripheral mu antagonists". Critical Care Clinics. 25 (3): 451–469, vii. doi:10.1016/j.ccc.2009.04.004. ISSN 1557-8232. PMID 19576524.
- Huupponen, E.; Maksimow, A.; Lapinlampi, P.; Särkelä, M.; Saastamoinen, A.; Snapir, A.; Scheinin, H.; Scheinin, M.; Meriläinen, P. (2008-02-01). "Electroencephalogram spindle activity during dexmedetomidine sedation and physiological sleep". Acta Anaesthesiologica Scandinavica. 52 (2): 289–294. doi:10.1111/j.1399-6576.2007.01537.x. ISSN 1399-6576. PMID 18005372.
- "Precedex (Dexmedetomidine hydrochloride) Drug Information: Clinical Pharmacology - Prescribing Information at RxList". RxList. Retrieved 2015-11-16.
- Shehabi, Yahya; Ruettimann, Urban; Adamson, Harriet; Innes, Richard; Ickeringill, Mathieu (2004-12-01). "Dexmedetomidine infusion for more than 24 hours in critically ill patients: sedative and cardiovascular effects". Intensive Care Medicine. 30 (12): 2188–2196. doi:10.1007/s00134-004-2417-z. ISSN 0342-4642. PMID 15338124.
- Gozalo-Marcilla, M.; Gasthuys, F.; Luna, S. P. L.; Schauvliege, S. (April 2018). "Is there a place for dexmedetomidine in equine anaesthesia and analgesia? A systematic review (2005-2017)". Journal of Veterinary Pharmacology and Therapeutics. 41 (2): 205–217. doi:10.1111/jvp.12474. PMID 29226340.
- "Freedom of Information Summary | Supplemental New Animal Drug Application | NADA 141-267 | Dexdomitor". Food and Drug Administration. 16 August 2010. Retrieved 2018-07-01.
- "Recent Animal Drug Approvals". U.S. Department of Health and Human Services. 2 June 2016. Retrieved 3 July 2016.
For the treatment of noise aversion in dogs
- "Veterinary medicines: product update". Veterinary Record. 177 (5): 116–117. 31 July 2015. doi:10.1136/vr.h4051. PMID 26231872.