Flucloxacillin
Flucloxacillin, also known as floxacillin, is a narrow-spectrum beta-lactam antibiotic of the penicillin class. It is used to treat infections caused by susceptible Gram-positive bacteria. Unlike other penicillins, flucloxacillin has activity against beta-lactamase-producing organisms such as Staphylococcus aureus[1] as it is beta-lactamase stable. However, it is ineffective against methicillin-resistant Staphylococcus aureus (MRSA).[2] It is very similar to dicloxacillin; they are considered interchangeable.
 | |
 | |
| Clinical data | |
|---|---|
| AHFS/Drugs.com | Micromedex Detailed Consumer Information |
| Pregnancy category |
|
| Routes of administration | Oral, IM, IV, intrapleural, intraarticular |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | 50–70% |
| Metabolism | Hepatic |
| Elimination half-life | 0.75–1 hour |
| Excretion | Renal |
| Identifiers | |
IUPAC name
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.023.683 |
| Chemical and physical data | |
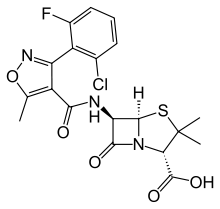
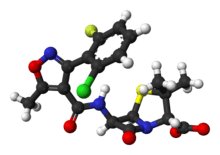
| Formula | C19H17ClFN3O5S |
| Molar mass | 453.87 g/mol g·mol−1 |
| 3D model (JSmol) | |
SMILES
| |
InChI
| |
| (verify) | |
It was patented in 1961.[3]
Medical uses
It is most commonly used to treat infections.
- Chest, ear, nose and throat (e.g. tonsillitis, sinusitis, pneumonia)
- Skin and soft tissue (e.g. boils, burns, wounds, abscesses, infected eczema, infected acne)
- Other infections including those of the heart (endocarditis), bones and joints (osteomyelitis), membranes of the brain (meningitis), guts (enteritis), blood (septicaemia), and the kidney, bladder or urethra
Flucloxacillin can also be used to prevent infections during major surgical procedures, particularly in heart or orthopedic surgery.
Flucloxacillin is indicated for the treatment of infections caused by susceptible bacteria. Specific approved indications include:[4][5]
- Staphylococcal skin infections and cellulitis – including impetigo, otitis externa, folliculitis, boils, carbuncles, and mastitis
- Pneumonia (adjunct)
- Osteomyelitis, septic arthritis
- Septicaemia
- Empirical treatment for endocarditis
- Surgical prophylaxis
Flucloxacillin has good activity against non-β-lactamase-producing bacteria including Streptococcus pyogenes.[6] Due to this widespread belief, empirical therapy for significant cellulitis often involves dual-therapy to cover both staphylococci and streptococci, however this has not shown to be of clinical benefit.[7]
Flucloxacillin is more acid-stable than many other penicillins and can be given orally, in addition to parenteral routes. However, like methicillin, it is less potent than benzylpenicillin against non-β-lactamase-producing Gram-positive bacteria.
Flucloxacillin has similar pharmacokinetics, antibacterial activity, and indications to dicloxacillin, and the two agents are considered interchangeable. It is reported to have higher, though rare, incidence of severe hepatic adverse effects than dicloxacillin,[8] but a lower incidence of renal adverse effects.[4]
Resistance
Despite flucloxacillin being insensitive to beta-lactamases, some organisms have developed resistance to it and other narrow-spectrum β-lactam antibiotics including methicillin. Such organisms include methicillin-resistant Staphylococcus aureus, which has developed resistance to flucloxacillin and other penicillins by having an altered penicillin-binding protein.
Adverse effects
Common adverse drug reactions associated with the use of flucloxacillin include: diarrhoea, nausea, rash, urticaria, pain and inflammation at injection site, superinfection (including candidiasis), allergy, and transient increases in liver enzymes and bilirubin.[4] Rarely, cholestatic jaundice (also referred to as cholestatic hepatitis) has been associated with flucloxacillin therapy. The reaction may occur up to several weeks after treatment has stopped, and takes weeks to resolve. The estimated incidence is one in 15,000 exposures, and is more frequent in people >55 years, females, and those with treatment longer than two weeks.[4][5]
Flucloxacillin is contraindicated in those with a previous history of allergy to penicillins, cephalosporins, or carbapenems. It should also not be used in the eye, or administered to those with a history of cholestatic hepatitis associated with the use of dicloxacillin or flucloxacillin.[4]
It should be used with caution in the elderly, patients with renal impairment where a reduced dose is required, and those with hepatic impairment, due to the risk of cholestatic hepatitis.[4]
It should be taken on an empty stomach, one half to one hour before food, as absorption is reduced when taken with food[9], though some studies suggest that this doesn't compromise flucloxacillin plasma concentrations in most circumstances. [10]
The UK NHS recommends taking at least 30 minutes before food or at least 2 hours after. [11]
Mechanism of action
Like other β-lactam antibiotics, flucloxacillin acts by inhibiting the synthesis of bacterial cell walls. It inhibits cross-linkage between the linear peptidoglycan polymer chains that make up a major component of the cell wall of Gram-positive bacteria.
Chemistry
Flucloxacillin is insensitive to beta-lactamase (also known as penicillinase) enzymes secreted by many penicillin-resistant bacteria. The presence of the isoxazolyl group on the side chain of the penicillin nucleus facilitates the β-lactamase resistance, since they are relatively intolerant of side chain steric hindrance. Thus, it is able to bind to penicillin-binding proteins and inhibit peptidoglycan crosslinking, but is not bound by or inactivated by β-lactamases.
Available forms
Flucloxacillin is commercially available as the sodium salt flucloxacillin sodium, in capsules (250 or 500 mg), oral suspensions (125 mg/5 ml or 250 mg/5 ml), and injections (powder for reconstitution, 250, 500 and 1000 mg per vial).
Flucloxacillin is supplied under a variety of trade names including Floxapen (Beecham, now GSK), Flopen (CSL), Staphylex (Alphapharm), Softapen (Rephco Pharmaceuticals Limited), Fabclox (Efedra Pharmaceuticals Pvt Ltd, India),Flubex (Beximco Pharmaceuticals Ltd, Bangladesh), Phylopen (Square Pharmaceuticals Ltd, Bangladesh) and Flupen (for state use only in South Africa). It is no longer available in the United States.
References
- Sutherland R, Croydon EA, Rolinson GN (November 1970). "Flucloxacillin, a new isoxazolyl penicillin, compared with oxacillin, cloxacillin, and dicloxacillin". Br Med J. 4 (5733): 455–60. doi:10.1136/bmj.4.5733.455. PMC 1820086. PMID 5481218.
- NHS: Methicillin-resistant Staphylococcus aureus (MRSA) - Guidance for nursing staff "methicillin resistance means the same as flucloxacillin resistance"
- Fischer, Jnos; Ganellin, C. Robin (2006). Analogue-based Drug Discovery. John Wiley & Sons. p. 491. ISBN 9783527607495.
- Rossi S, editor. Australian Medicines Handbook 2006. Adelaide: Australian Medicines Handbook; 2006.
- Joint Formulary Committee. British National Formulary, 50th edition. London: British Medical Association and Royal Pharmaceutical Society of Great Britain; 2005.
- "Streptococcal skin infection - DermNet New Zealand". www.dermnetnz.org.
- Leman, P; Mukherjee, D (2005). "Flucloxacillin alone or combined with benzylpenicillin to treat lower limb cellulitis: A randomised controlled trial". Emergency Medicine Journal. 22 (5): 342–6. doi:10.1136/emj.2004.019869. PMC 1726763. PMID 15843702.
- "US National Library of Medicine: Livertox. PENICILLINASE-RESISTANT PENICILLINS, SECOND-GENERATION PENICILLINS".
- "New Zealand Consumer Medicine Information" (PDF). medsafe.govt.nz.
- Gardiner, Sharon; Drennan, Phillip; Begg, Ronald (2018). "In healthy volunteers, taking flucloxacillin with food does not compromise effective plasma concentrations in most circumstances". PLOS ONE. 13 (7): e0199370. doi:10.1371/journal.pone.0199370. PMC 6042703. PMID 30001392.