Nifedipine
Nifedipine, sold under the brand name Adalat among others, is a medication used to manage angina, high blood pressure, Raynaud's phenomenon, and premature labor.[1] It is one of the treatments of choice for Prinzmetal angina.[1] It may be used to treat severe high blood pressure in pregnancy.[1] Its use in preterm labor may allow more time for steroids to improve the baby's lung function and provide time for transfer of the mother to a well qualified medical facility before delivery.[1] Nifedipine is taken by mouth and comes in fast and slow release formulations.[1]
 | |||
| |||
| Clinical data | |||
|---|---|---|---|
| Trade names | Adalat, Procardia, others | ||
| AHFS/Drugs.com | Monograph | ||
| MedlinePlus | a684028 | ||
| Pregnancy category |
| ||
| Routes of administration | by mouth, topical | ||
| ATC code | |||
| Pharmacokinetic data | |||
| Bioavailability | 45-56% | ||
| Protein binding | 92-98% | ||
| Metabolism | Gastrointestinal, Liver | ||
| Elimination half-life | 2 hours | ||
| Excretion | Kidneys: >50%, Biliary: 5-15% | ||
| Identifiers | |||
IUPAC name
| |||
| CAS Number | |||
| PubChem CID | |||
| IUPHAR/BPS | |||
| DrugBank | |||
| ChemSpider | |||
| UNII | |||
| KEGG | |||
| ChEBI | |||
| ChEMBL | |||
| CompTox Dashboard (EPA) | |||
| ECHA InfoCard | 100.040.529 | ||
| Chemical and physical data | |||
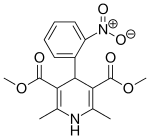
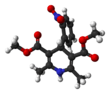
| Formula | C17H18N2O6 | ||
| Molar mass | 346.335 g/mol g·mol−1 | ||
| 3D model (JSmol) | |||
| Melting point | 173 °C (343 °F) | ||
SMILES
| |||
InChI
| |||
| (verify) | |||
Common side effects include lightheadedness, headache, feeling tired, leg swelling, cough, and shortness of breath.[1] Serious side effects may include low blood pressure and heart failure.[1] There is tentative evidence that its use in pregnancy is safe; however, it is not recommended during breastfeeding.[2] It is a calcium channel blocker of the dihydropyridine type.[1]
Nifedipine was patented in 1967 and approved for use in the United States in 1981.[1][3][4] It is on the World Health Organization's List of Essential Medicines, the most effective and safe medicines needed in a health system.[5] It is available as a generic medication.[1] The wholesale price in the developing world for the slow-release form is approximately US$1.90–3.80 per month.[6] In the United States, it costs approximately $40–60 per month, depending on the dose.[1] In 2016 it was the 154th most prescribed medication in the United States with more than 4 million prescriptions.[7]
Medical uses
High blood pressure
The approved uses are for the long-term treatment of hypertension and angina pectoris. In hypertension, recent clinical guidelines generally favour diuretics and ACE inhibitors, although calcium channel antagonists, along with thiazide diuretics, are still favoured as primary treatment for patients over 55 and African American patients.[8]
Nifedipine given as sublingual administration has previously been used in hypertensive emergencies. It was once frequently prescribed on an as-needed basis to patients taking MAOIs for real or perceived hypertensive crises.[9] This was found to be dangerous, and has been abandoned. Sublingual administration of nifedipine promotes a hypotensive effect via peripheral vasodilation. It can cause an uncontrollable decrease in blood pressure, reflex tachycardia, and a steal phenomenon in certain vascular beds. There have been multiple reports in the medical literature of serious adverse effects with sublingual nifedipine, including cerebral ischemia/infarction, myocardial infarction, complete heart block, and death. As a result of this, in 1985 the FDA reviewed all data regarding the safety and effectiveness of sublingual nifedipine for the management of hypertensive emergencies, and concluded that the practice should be abandoned because it was neither safe nor effective.[10][11] An exception to the avoidance of this practice is in the use of nifedipine for the treatment of hypertension associated with autonomic dysreflexia in spinal cord injury.[12]
Early labor
Nifedipine has been used frequently as a tocolytic (agent that delays premature labor). A Cochrane review has concluded that it has benefits over placebo or no treatment for prolongation of pregnancy. It also has benefits over beta-agonists and may also have some benefits over atosiban and magnesium sulfate, although atosiban results in fewer maternal adverse effects. No difference was found in the rate of deaths among babies around the time of birth, while data on longer-term outcomes is lacking.[13]
Other
Raynaud's phenomenon is often treated with nifedipine. A 2005 meta-analysis showed modest benefits (33% decrease in attack severity, 2.8-5 reduction in absolute number of attacks per week); it does conclude that most included studies used low doses of nifedipine.[14]
Topical nifedipine has been shown to be as effective as topical nitrates for anal fissures.[15]
Nifedipine is also used in high-altitude medicine to treat high altitude pulmonary edema.[16]
Other uses include painful spasms of the esophagus such as from cancer or tetanus. It is also used for the small subset of people with pulmonary hypertension.
Side effects
Nifedipine rapidly lowers blood pressure, and patients are commonly warned they may feel dizzy or faint after taking the first few doses. Tachycardia (fast heart rate) may occur as a reaction. These problems are much less frequent in the sustained-release preparations of nifedipine.
Extended release formulations of nifedipine should be taken on an empty stomach, and patients are warned not to consume anything containing grapefruit or grapefruit juice, as they raise blood nifedipine levels. There are several possible mechanisms, including the inhibition of CYP3A4-mediated metabolism.[17]
Overdose
A number of persons have developed toxicity due to acute overdosage with nifedipine, either accidentally or intentionally, and via either oral or parenteral administration. The adverse effects include lethargy, bradycardia, marked hypotension and loss of consciousness. The drug may be quantified in blood or plasma to confirm a diagnosis of poisoning, or to assist in a medicolegal investigation following death. Analytical methods usually involve gas or liquid chromatography and specimen concentrations are usually in the 100-1000 μg/L range.[18][19]
Mechanism of action
Nifedipine is a calcium channel blocker. Although nifedipine and other dihydropyridines are commonly regarded as specific to the L-type calcium channel, they also possess nonspecific activity towards other voltage-dependent calcium channels.[20][21]
Nifedipine has additionally been found to act as an antagonist of the mineralocorticoid receptor, or as an antimineralocorticoid.[22]
History
Nifedipine (initially BAY a1040) was developed by the German pharmaceutical company Bayer, with most initial studies being performed in the early 1970s.[23]
The use of nifedipine and related calcium channel antagonists was much reduced in response to 1995 trials that mortality was increased in patients with coronary artery disease who took nifedipine.[24] This study was a meta-analysis, and demonstrated harm mainly in short-acting forms of nifedipine (that could cause large fluctuations in blood pressure) and at high doses of 80 mg a day and more.[25]
See also
References
- "Nifedipine". The American Society of Health-System Pharmacists. [:https://web.archive.org/web/20180808043257/https://www.drugs.com/monograph/nifedipine.html Archived] Check
|archiveurl=value (help) from the original on 2018-08-08. Retrieved Sep 17, 2019. - "Nifedipine Pregnancy and Breastfeeding Warnings". Archived from the original on 21 December 2015. Retrieved 25 December 2015.
- Corey, E.J. (2013). Drug discovery practices, processes, and perspectives. Hoboken, N.J.: John Wiley & Sons. p. 172. ISBN 9781118354469. Archived from the original on 2017-09-01.
- Fischer, Jnos; Ganellin, C. Robin (2006). Analogue-based Drug Discovery. John Wiley & Sons. p. 464. ISBN 9783527607495.
- "WHO Model List of Essential Medicines (19th List)" (PDF). World Health Organization. April 2015. Archived (PDF) from the original on 13 December 2016. Retrieved 8 December 2016.
- "Nifedipine". International Drug Price Indicator Guide. Retrieved 25 December 2015.
- "The Top 300 of 2019". clincalc.com. Retrieved 22 December 2018.
- Hypertension: management of hypertension in adults in primary care. Clinical guideline CG34. National Institute for Health and Clinical Excellence (NICE), June 2006. Fulltext index Archived 2007-06-17 at the Wayback Machine. ISBN 1-86016-285-1.
- "Nifedipine for MAOI Hypertension? Reversing a Previous Recommendation". Biological Therapies in Psychiatry. March 1997. Archived from the original on 2015-09-10. Retrieved 22 Jan 2015.
- Grossman E, Messerli FH, Grodzicki T, Kowey P (1996). "Should a moratorium be placed on sublingual nifedipine capsules given for hypertensive emergencies and pseudoemergencies?". JAMA. 276 (16): 1328–31. doi:10.1001/jama.276.16.1328. PMID 8861992.
- Varon J, Marik PE (2003). "Clinical review: The management of hypertensive crises". Critical Care (London, England). 7 (5): 374–84. doi:10.1186/cc2351. PMC 270718. PMID 12974970.
- Campagnolo, DI. "Autonomic Dysreflexia in Spinal Cord Injury". eMedicine. Retrieved 2011-07-14.
- Flenady, Vicki; Wojcieszek, Aleena M.; Papatsonis, Dimitri N. M.; Stock, Owen M.; Murray, Linda; Jardine, Luke A.; Carbonne, Bruno (2014-06-05). "Calcium channel blockers for inhibiting preterm labour and birth". The Cochrane Database of Systematic Reviews (6): CD002255. doi:10.1002/14651858.CD002255.pub2. ISSN 1469-493X. PMID 24901312.
- Thompson AE, Pope JE (2005). "Calcium channel blockers for primary Raynaud's phenomenon: a meta-analysis". Rheumatology (Oxford, England). 44 (2): 145–50. doi:10.1093/rheumatology/keh390. PMID 15546967.
- Ezri T, Susmallian S (2003). "Topical nifedipine vs. topical glyceryl trinitrate for treatment of chronic anal fissure". Dis. Colon Rectum. 46 (6): 805–8. doi:10.1007/s10350-004-6660-8. PMID 12794583.
- Ali, Mir Omar & Qazi, Samia (2007-09-19). "Pulmonary Edema, High-Altitude". eMedicine. Archived from the original on 2007-11-16. Retrieved 2007-11-25.
- Odou P, Ferrari N, Barthélémy C, et al. (2005). "Grapefruit juice-nifedipine interaction: possible involvement of several mechanisms". Journal Clinical Pharm Ther. 30 (2): 153–8. doi:10.1111/j.1365-2710.2004.00618.x. PMID 15811168.
- Nifediac package insert, TEVA Pharmaceuticals, Sellersville, Pennsylvania, August, 2009.
- Baselt, Randall C. (2008). Disposition of Toxic Drugs and Chemicals in Man. Foster City, CA: Biomedical Publications. pp. 1108–1110. ISBN 978-0-9626523-7-0.
- Curtis, Tim M.; Scholfield, C. Norman (May 2001). "Nifedipine blocks Ca2+ store refilling through a pathway not involving L-type Ca2+ channels in rabbit arteriolar smooth muscle store refilling through a pathway not involving L-type Ca2+ channels in rabbit arteriolar smooth muscle". The Journal of Physiology. 532 (3): 609–623. doi:10.1111/j.1469-7793.2001.0609e.x. PMC 2278590. PMID 11313433.
- McDonald, TF; Pelzer, S; Trautwein, W; Pelzer, DJ (April 1994). "Regulation and modulation of calcium channels in cardiac, skeletal, and smooth muscle cells". Physiological Reviews. 74 (2): 365–507. doi:10.1152/physrev.1994.74.2.365. PMID 8171118.
- Luther, James M. (2014). "Is there a new dawn for selective mineralocorticoid receptor antagonism?". Current Opinion in Nephrology and Hypertension. 23 (5): 456–461. doi:10.1097/MNH.0000000000000051. ISSN 1062-4821. PMC 4248353. PMID 24992570.
- Vater W, Kroneberg G, Hoffmeister F, et al. (1972). "[Pharmacology of 4-(2'-nitrophenyl)-2,6-dimethyl-1,4-dihydropyridine-3,5-dicarboxylic acid dimethyl ester (Nifedipine, BAY a 1040)]". Arzneimittel-Forschung (in German). 22 (1): 1–14. PMID 4622472.
- Furberg CD, Psaty BM, Meyer JV (1995). "Nifedipine. Dose-related increase in mortality in patients with coronary heart disease". Circulation. 92 (5): 1326–31. doi:10.1161/01.cir.92.5.1326. PMID 7648682.
- Opie LH, Messerli FH (1995). "Nifedipine and mortality. Grave defects in the dossier". Circulation. 92 (5): 1068–73. doi:10.1161/01.cir.92.5.1068. PMID 7648646.