Temocillin
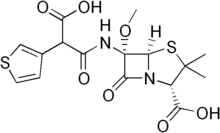
Temocillin is a β-lactamase-resistant penicillin[1][2] introduced by Beecham, marketed by Eumedica Pharmaceuticals as Negaban. It is used primarily for the treatment of multiple drug-resistant, Gram-negative bacteria.
It is a 6-methoxy penicillin; it is also a carboxypenicillin.[3]
 | |
| Clinical data | |
|---|---|
| AHFS/Drugs.com | International Drug Names |
| ATC code | |
| Identifiers | |
IUPAC name
| |
| CAS Number | |
| PubChem CID | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ECHA InfoCard | 100.060.148 |
| Chemical and physical data | |
| Formula | C16H18N2O7S2 |
| Molar mass | 414.453 g/mol g·mol−1 |
| 3D model (JSmol) | |
SMILES
| |
InChI
| |
| (verify) | |
Pharmacology
Temocillin is a β-lactamase-resistant penicillin. It is not active against Gram-positive bacteria or bacteria with altered penicillin-binding proteins.
It is normally active against Moraxella catarrhalis, Brucella abortus, Burkholderia cepacia, Citrobacter species, Escherichia coli, Haemophilus influenzae, Klebsiella pneumoniae, Pasteurella multocida, Proteus mirabilis, Salmonella typhimurium, and Yersinia enterocolitica. It is also active against some Enterobacter species, Morganella morganii, and Serratia species. Temocillin has no useful activity against Acinetobacter species or Pseudomonas aeruginosa.
Its primary use is against Enterobacteriaceae, and in particular against strains producing extended-spectrum β-lactamase or AmpC β-lactamase.[4]
Dosage
The common dose is 2 g intravenously every 12 hours and the high dose, notably in critically ill patients, is 2g every 8 hours. Theoretical reasons exist for giving temocillin as a continuous intravenous infusion in severe disease:[5][6] a single loading dose of 2 g is given intravenously followed by a 4-g or 6-g infusion over 24 hours. According to the SPC, chemical and physical in-use stability has been demonstrated for 24 hours at 25°C for the following solvents: water for injection, physiological saline (0.9% sodium chloride), dextrose 5%, sodium chloride compound (Ringer’s solution), Hartmann solution (sodium lactate compound + Ringer’s lactate solution). Temocillin for intravenous injection is diluted in 10 to 20 ml of sterile water; it is diluted in less than 2 ml of sterile water when being prepared for intramuscular injection; the continuous infusion is diluted in 48 ml of sterile water for ease of administration (2 ml per hour). To reduce pain, the intramuscular injection may be made up using sterile 1% lignocaine instead of sterile water.
Temocillin may be given to patients with impaired renal function after the dose has been adapted:
| Creatinine clearance (mL/min) | Dosage per administration | Interval between administrations |
|---|---|---|
| More than 60 | 2 g | 12 h |
| 60 to 30 | 1 g | 12 h |
| 30 to 10 | 1 g | 24 h |
In case of intermittent high-flux hemodialysis: 1 g (I.V. injection) per 24 h of inter-dialytic session, preferably at the end of the hemodialysis (1 g q24 h, 2 g q48 h, 3 g q72 h). In case of continuous peritoneal dialysis in ambulatory patients: 1 g every 24 hours.
No oral preparation of temocillin is licensed.
Adverse effects
The undesirable effects of temocillin are those of any β-lactam antibiotic. In particular, it has been associated with angioedema and anaphylaxis in penicillin-allergic patients. Animal studies have not shown any induction of Clostridium difficile infection.[7] As with any other penicillin, convulsions can occur if very high doses are given.
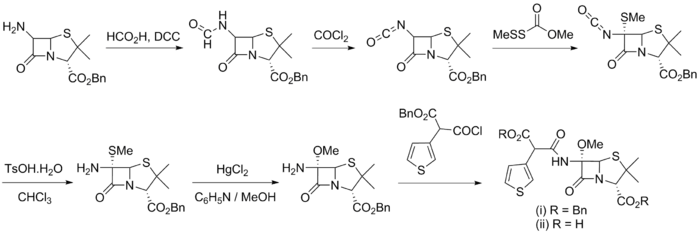
Synthesis
References
- Andrews JM, Jevons G, Walker R, Ashby J, Fraise AP (July 2007). "Temocillin susceptibility by BSAC methodology". J. Antimicrob. Chemother. 60 (1): 185–7. doi:10.1093/jac/dkm179. PMID 17550891.
- Van Landuyt HW, Pyckavet M, Lambert A, Boelaert J (October 1982). "In vitro activity of temocillin (BRL 17421), a novel beta-lactam antibiotic". Antimicrob. Agents Chemother. 22 (4): 535–40. doi:10.1128/aac.22.4.535. PMC 183789. PMID 7181470.
- Chanal M, Sirot J, Cluzel M, Joly B, Glanddier Y (June 1983). "[In vitro study of the bacteriostatic and bactericidal activity of temocillin (BRL 17421)]". Pathol. Biol. (in French). 31 (6): 467–70. PMID 6348653.
- Livermore DM et al. (2006) Activity of temocillin vs. prevalent ESBL- and AmpC-producing Enterobacteriaceae from SE England. J Antimicrob Chemother. 2006 May;57(5):1012-4.
- De Jongh R et al. (2008) Continuous versus intermittent infusion of temocillin, a directed spectrum penicillin for intensive care patients with nosocomial pneumonia: stability, compatibility, population pharmacokinetic studies and breakpoint selection. J Antimicrob Chemother. 2008 Feb;61(2):382-8.
- Laterre PF et al. (2015) Temocillin (6 g daily) in critically ill patients: continuous infusion versus three times daily administration. J Antimicrob Chemother. 2015 Mar;70(3):891-8.
- Boon RJ, et al. (1985). "Studies with temocillin in a hamster model of antibiotic-associated colitis". Antimicrob Agents Chemother. 27 (6): 980–1. doi:10.1128/aac.27.6.980. PMC 180203. PMID 3875312.
- Bentley, P. H.; Clayton, J. P.; Boles, M. O.; Girven, R. J. (1979). "Transformations using benzyl 6-isocyanopenicillanate". Journal of the Chemical Society, Perkin Transactions 1: 2455. doi:10.1039/P19790002455.
Further reading
- Livermore DM, Tulkens PM (February 2009). "Temocillin revived". Journal of Antimicrobial Chemotherapy. 63 (2): 243–5. doi:10.1093/jac/dkn511. PMID 19095679.