Enterobacter
Enterobacter is a genus of common Gram-negative, facultatively anaerobic, rod-shaped, non-spore-forming bacteria of the family Enterobacteriaceae. It is the type genus of the order Enterobacterales.[1] Several strains of these bacteria are pathogenic and cause opportunistic infections in immunocompromised (usually hospitalized) hosts and in those who are on mechanical ventilation. The urinary and respiratory tracts are the most common sites of infection. The genus Enterobacter is a member of the coliform group of bacteria. It does not belong to the fecal coliforms (or thermotolerant coliforms) group of bacteria, unlike Escherichia coli, because it is incapable of growth at 44.5 °C in the presence of bile salts. Some of them showed quorum sensing properties as reported before.[2][3]
| Enterobacter | |
|---|---|
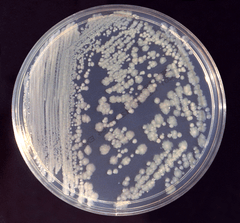 | |
| Enterobacter cloacae on tryptic soy broth agar. | |
| Scientific classification | |
| Kingdom: | Bacteria |
| Phylum: | |
| Class: | |
| Order: | |
| Family: | |
| Genus: | Enterobacter Hormaeche & Edwards 1960 |
| Species | |
|
E. amnigenus | |
| Synonyms | |
|
Cloaca Castellani & Chalmers, 1919
| |
One clinically important species from this genus is E. cloacae.
Researchers in 2018 reported, after detecting the presence on the International Space Station (ISS) of five Enterobacter bugandensis bacterial strains, none pathogenic to humans, that microorganisms on ISS should be carefully monitored to continue assuring a medically healthy environment for the astronauts.[4][5]
Biochemical characteristics
The genus Enterobacter ferments lactose with gas production during a 48-hour incubation at 35-37 °C in the presence of bile salts and detergents. It is oxidase-negative, indole-negative, and urease-variable.[3][6]
Treatment
- Note: Treatment is dependent on local trends of antibiotic resistance. Enterobacter huaxiensis and Enterobacter chuandaensis are two recently discovered species that exhibit especially antibiotic resistant characteristics. "Enterobacter strains 090008T and 090028T were recovered from the blood of two different patients at West China Hospital, Chengdu, PR China in 2017" [7]
- Cefepime, a fourth-generation cephalosporin from the β-Lactam antibiotic class.
- Imipenem (carbapenems) is often the antibiotic of choice.
- Aminoglycosides such as amikacin have been found to be very effective, as well.[6]
- Quinolones can be an effective alternative.[6]
Linked to obesity
A recent study has shown that the presence of Enterobacter cloacae B29 in the gut of a morbidly obese individual may have contributed to the patient’s obesity. Reduction of the bacterial load within the patient’s gut, from 35% E. cloacae B29 to non-detectable levels, was associated with a parallel reduction in endotoxin load in the patient and a concomitant, significant reduction in weight.[8] Furthermore, the same bacterial strain, isolated from the patient, induced obesity and insulin resistance in germfree C57BL/6J mice that were being fed a high-fat diet. The study concludes that E. cloacae B29 may contribute to obesity in its human hosts through an endotoxin-induced, inflammation-mediated mechanism.[8]
References
- Adeolu, M.; et al. (2016). "Genome based phylogeny and taxonomy of the 'Enterobacteriales': proposal for Enterobacterales ord. nov. divided into the families Enterobacteriaceae, Erwiniaceae fam. nov., Pectobacteriaceae fam. nov., Yersiniaceae fam. nov., Hafniaceae fam. nov., Morganellaceae fam. nov., and Budviciaceae fam. nov". Int. J. Syst. Evol. Microbiol.
- Tan, Wen-Si; Muhamad Yunos, Nina Yusrina; Tan, Pui-Wan; Mohamad, Nur Izzati; Adrian, Tan-Guan-Sheng; Yin, Wai-Fong; Chan, Kok-Gan (13 June 2014). "Freshwater-Borne Bacteria Isolated from a Malaysian Rainforest Waterfall Exhibiting Quorum Sensing Properties". Sensors. 14 (6): 10527–10537. doi:10.3390/s140610527. PMC 4118381. PMID 24932870.
- Cabral, JPS (2010). "Water Microbiology. Bacterial Pathogens and Water". Int. J. Environ. Res. Public Health. 7 (10): 3657–3703. doi:10.3390/ijerph7103657. PMC 2996186. PMID 21139855.
- BioMed Central (22 November 2018). "ISS microbes should be monitored to avoid threat to astronaut health". EurekAlert!. Retrieved 25 November 2018.
- Singh, Nitin K.; et al. (23 November 2018). "Multi-drug resistant Enterobacter bugandensis species isolated from the International Space Station and comparative genomic analyses with human pathogenic strains". BMC Microbiology. 18 (1): 175. doi:10.1186/s12866-018-1325-2. PMC 6251167. PMID 30466389.
- Russo Thomas A, Johnson James R, "Chapter 143. Diseases Caused by Gram-Negative Enteric Bacilli" (Chapter). Fauci AS, Braunwald E, Kasper DL, Hauser SL, Longo DL, Jameson JL, Loscalzo J: Harrison's Principles of Internal Medicine, 17e: http://www.accessmedicine.com/content.aspx?aID=2894446.
- Wu, Wenjing (19 October 2018). "Enterobacter huaxiensis sp. nov. and Enterobacter chuandaensis sp. nov., recovered from human blood". International Journal of Systematic and Evolutionary Microbiology: 708–714. doi:10.1099/ijsem.0.003207.
- Fei, Na; Zhao, Liping (December 13, 2012). "An opportunistic pathogen isolated from the gut of an obese human causes obesity in germfree mice". The ISME Journal. 7 (4): 880–4. doi:10.1038/ismej.2012.153. ISSN 1751-7362. PMC 3603399. PMID 23235292.
External links
| Wikispecies has information related to Enterobacter |