Suramin
Suramin is a medication used to treat African sleeping sickness and river blindness.[1][2] It is the treatment of choice for sleeping sickness without central nervous system involvement.[3] It is given by injection into a vein.[4]
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Antrypol, 309 F, 309 Fourneau, Bayer 205, Moranyl, Naganin, Naganine |
| Routes of administration | by injection only |
| ATC code | |
| Legal status | |
| Legal status |
|
| Identifiers | |
IUPAC name
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.005.145 |
| Chemical and physical data | |
| Formula | C51H40N6O23S6 |
| Molar mass | 1297.26 g·mol−1 |
| 3D model (JSmol) | |
SMILES
| |
InChI
| |
| | |
Suramin causes a fair number of side effects.[4] Common side effects include nausea, vomiting, diarrhea, headache, skin tingling, and weakness.[2] Sore palms of the hands and soles of the feet, trouble seeing, fever, and abdominal pain may also occur.[2] Severe side effects may include low blood pressure, decreased level of consciousness, kidney problems, and low blood cell levels.[4] It is unclear if it is safe when breastfeeding.[2]
Suramin was made at least as early as 1916.[5] It is on the World Health Organization's List of Essential Medicines, the most effective and safe medicines needed in a health system.[6] In the United States it can be acquired from the Center for Disease Control (CDC).[3] The cost of the medication for a course of treatment is about 27 USD.[7] In regions of the world where the disease is common suramin is provided for free by the World Health Organization.[8]
Medical uses
Suramin is used for treatment of human sleeping sickness caused by trypanosomes.[1] Specifically, it is used for treatment of first-stage African trypanosomiasis caused by Trypanosoma brucei rhodesiense and Trypanosoma brucei gambiense without involvement of central nervous system.[9][10] It is considered first-line treatment for Trypanosoma brucei rhodesiense, and second-line treatment for early-stage Trypanosoma brucei gambiense, where pentamidine is recommended as first line.[10]
It has been used in the treatment of river blindness (onchocerciasis).[2]
Pregnancy and breastfeeding
It is unknown whether it is safe for the baby when a woman takes it while breastfeeding.[2]
Adverse reactions
The most frequent adverse reactions are nausea, vomiting, diarrhea, abdominal pain, and a feeling of general discomfort. It is also common to experience various sensations in the skin, from crawling or tingling sensations, tenderness of palms and the soles, and numbness of hands, arm, legs or feet.[11] Other skin reactions include skin rash, swelling and stinging sensation.[11] Suramin can also cause loss of appetite and irritability.[11] Suramin causes non-harmful changes in urine during use, specifically making the urine cloudy.[11] It may exacerbate kidney disease.[12]
Less common side effects include extreme fatigue, ulcers in the mouth, and painful tender glands in the neck, armpits and groin.[11] Suramin uncommonly affects the eyes causing watery eyes, swelling around the eyes, photophobia, and changes or loss of vision.[11]
Rare side effects include hypersensitivity reactions causing difficulty breathing. Other rare systemic effects include decreased blood pressure, fever, rapid heart rate, and convulsions.[11] Other rare side effects include symptoms of liver dysfunction such as tenderness in upper abdomen, jaundice in eyes and skin, unusual bleeding or bruising.[11]
Suramin has been applied clinically to HIV/AIDS patients resulting in a significant number of fatal occurrences and as a result the application of this molecule was abandoned for this condition.[13]
Pharmacokinetics
Suramin is not orally bioavailable and is given intravenously. Intramuscular and subcutaneous administration could result in local tissue inflammation or necrosis. Suramin is approximately 99-98% protein bound in the serum and has a half-life of 41–78 days average of 50 days; however, the pharmacokinetics of suramin can vary substantially between individual patients. Suramin does not distribute well into cerebral spinal fluid and its concentration in the tissues is equivalently lower than its concentration in the plasma. Suramin is not extensively metabolized and about 80% is eliminated via the kidneys.[12]
Chemistry
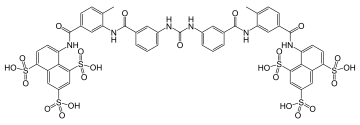
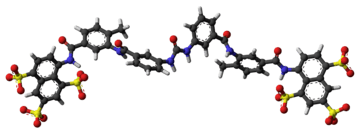
The molecular formula of suramin is C51H40N6O23S6. It is a symmetric molecule in the center of which lies a urea (NH–CO–NH) functional group. Suramin contains six aromatic systems – four benzene rings, sandwiched by a pair of naphthalene moieties – plus four amide functional groups (in addition to the urea) and six sulfonic acid groups. When given as a medication, it is usually delivered as the sodium sulfonate salt as this formulation is water-soluble, though it does deteriorate rapidly in air.[12]
Mechanism of action
The mechanism of action for suramin is unclear, however, it is thought that parasites are able to selectively uptake suramin via receptor-mediated endocytosis of drug that is bound to low-density lipoproteins and to a lesser extent, other serum proteins.[12] Once inside parasites, suramin combines with proteins, especially trypanosomal glycolytic enzymes to inhibit energy metabolism.[14]
History
Suramin was first made by the chemists Oskar Dressel, Richard Kothe and Bernhard Heymann at Bayer AG laboratories in Elberfeld, after research on a series of urea-like compounds. The drug is still sold by Bayer under the brand name Germanin. The chemical structure of suramin was kept secret by Bayer for commercial and strategic reasons, however, it was elucidated and published in 1924 by Ernest Fourneau and his team of the Pasteur Institute.[15]:378–379[16]
Research
It is also used as a research reagent to inhibit the activation of heterotrimeric G proteins in a variety of GPCRs with varying potency. It prevents the association of heteromeric G proteins and therefore the receptors guanine exchange functionality (GEF). With this blockade the GDP will not release from the Gα subunit so it can not be replaced by a GTP and become activated. This has the effect of blocking downstream G protein mediated signaling of various GPCR proteins including rhodopsin, the A1 adenosine receptor, the D2 receptor,[17] the P2 receptor,[18][19] and ryanodine receptors.[20]
Suramin was studied as a possible treatment for prostate cancer in a clinical trial.[21]
Suramin has been studied in a mouse model of autism and in a small phase I/II human trial that was published in May 2017.[22][23][24]
References
- "WHO Model List of Essential Medicines. 18th list (April 2013)" (PDF). World Health Organization. October 2013. Archived (PDF) from the original on 23 April 2014. Retrieved 22 April 2014.
- "Micromedex Detailed Drug Information for the Consumer: Suramin (Injection route)". PubMed Health. 1 November 2016. Archived from the original on 8 September 2017.
- "Our Formulary Infectious Diseases Laboratories CDC". www.cdc.gov. 22 September 2016. Archived from the original on 16 December 2016. Retrieved 30 November 2016.
- Zuckerman, Dr Jane N. (2002). Principles and Practice of Travel Medicine. John Wiley & Sons. p. 113. ISBN 9780471490791. Archived from the original on 2016-11-30.
- Mehlhorn, Heinz (2008). Encyclopedia of Parasitology: A-M. Springer Science & Business Media. p. 475. ISBN 9783540489948. Archived from the original on 2016-11-30.
- "WHO Model List of Essential Medicines (19th List)" (PDF). World Health Organization. April 2015. Archived (PDF) from the original on 13 December 2016. Retrieved 8 December 2016.
- Dumas, Michel; Bouteille, Bernard; Buguet, Alain (2013). Progress in Human African Trypanosomiasis, Sleeping Sickness. Springer Science & Business Media. p. 256. ISBN 9782817808574. Archived from the original on 2016-11-30.
- "Trypanosomiasis, human African (sleeping sickness)". World Health Organization. February 2016. Archived from the original on 4 December 2016. Retrieved 7 December 2016.
- "CDC Infectious Diseases Laboratory: Our Formulary". CDC. Archived from the original on 2016-11-08. Retrieved 2016-11-08.
- Kappagoda, Shanthi; Singh, Upinder; Blackburn, Brian G. (September 22, 2016). "Antiparasitic Therapy". Mayo Clinic Proceedings. 86 (6): 561–583. doi:10.4065/mcp.2011.0203. ISSN 0025-6196. PMC 3104918. PMID 21628620.
- "Suramin Injection Advanced Patient Information - Drugs.com". Archived from the original on 2016-11-08. Retrieved 2016-11-08.
- Phillips, Margaret A.; Stanley, Jr, Samuel L. (2011). "Chapter 50: Chemotherapy of Protozoal Infections: Amebiasis, Giardiasis, Trichomoniasis, Trypanosomiasis, Leishmaniasis, and Other Protozoal Infections". In Brunton, Laurence L.; Chabner, Bruce A.; Knollmann, Bjorn Christian (eds.). Goodman and Gilman's The Pharmacological Basis of Therapeutics (12th ed.). McGraw Hill. pp. 1437–1438. ISBN 9780071769396.
- Kaplan, Lawrence D.; Wolfe, Peter R.; Volberding, Paul A.; Feorino, Paul; Abrams, Donald I.; Levy, Jay A.; Wong, Roberta; Kaufman, Lilian; Gottlieb, Michael S. (1987). "Lack of response to suramin in patients with AIDS and AIDS-related complex". The American Journal of Medicine. 82 (3): 615–620. doi:10.1016/0002-9343(87)90108-2. PMID 3548350.
- Moore, Thomas A. (2015). "246e: Agents Used to Treat Parasitic Infections". In Kasper, Dennis L.; et al. (eds.). Harrison's Principles of Internal Medicine (19th ed.). McGraw-Hil. ISBN 9780071802161.
- Walter Sneader (2005). Drug Discovery: A History. John Wiley & Sons. ISBN 9780471899792.
- Fourneau, E.; Tréfouël, J.; Vallée, J. (1924). "Sur une nouvelle série de médicaments trypanocides". Comptes Rendus des Séances de l'Académie des Sciences. 178: 675.
- Beindl W, Mitterauer T, Hohenegger M, Ijzerman AP, Nanoff C, Freissmuth M (August 1996). "Inhibition of receptor/G protein coupling by suramin analogues". Molecular Pharmacology. 50 (2): 415–23. PMID 8700151. Archived from the original on 2017-09-08.
- Abbracchio MP, Burnstock G, Boeynaems JM, Barnard EA, Boyer JL, Kennedy C, Knight GE, Fumagalli M, Gachet C, Jacobson KA, Weisman GA (September 2006). "International Union of Pharmacology LVIII: update on the P2Y G protein-coupled nucleotide receptors: from molecular mechanisms and pathophysiology to therapy". Pharmacological Reviews. 58 (3): 281–341. doi:10.1124/pr.58.3.3. PMC 3471216. PMID 16968944.
- Khakh BS, Burnstock G, Kennedy C, King BF, North RA, Séguéla P, Voigt M, Humphrey PP (March 2001). "International union of pharmacology. XXIV. Current status of the nomenclature and properties of P2X receptors and their subunits". Pharmacological Reviews. 53 (1): 107–118. PMID 11171941. Archived from the original on 2016-11-18.
- Wolner I, Kassack MU, Ullmann H, Karel A, Hohenegger M (October 2005). "Use-dependent inhibition of the skeletal muscle ryanodine receptor by the suramin analogue NF676". British Journal of Pharmacology. 146 (4): 525–33. doi:10.1038/sj.bjp.0706359. PMC 1751178. PMID 16056233.
- Ahles TA, Herndon JE, Small EJ, et al. (November 2004). "Quality of life impact of three different doses of suramin in patients with metastatic hormone-refractory prostate carcinoma: results of Intergroup O159/Cancer and Leukemia Group B 9480". Cancer. 101 (10): 2202–8. doi:10.1002/cncr.20655. PMID 15484217.
- Scott LaFee and Heather Buschman. Researchers Studying Century-Old Drug in Potential New Approach to Autism. UC San Diego Health, May 26, 2017 Archived June 1, 2017, at the Wayback Machine
- Naviaux, J C; Schuchbauer, M A; Li, K; Wang, L; Risbrough, V B; Powell, S B; Naviaux, R K (2014). "Reversal of autism-like behaviors and metabolism in adult mice with single-dose antipurinergic therapy". Translational Psychiatry. 4 (6): e400. doi:10.1038/tp.2014.33. PMC 4080315.
- Naviaux, Robert K.; Curtis, Brooke; Li, Kefeng; Naviaux, Jane C.; Bright, A. Taylor; Reiner, Gail E.; Westerfield, Marissa; Goh, Suzanne; Alaynick, William A.; Wang, Lin; Capparelli, Edmund V.; Adams, Cynthia; Sun, Ji; Jain, Sonia; He, Feng; Arellano, Deyna A.; Mash, Lisa E.; Chukoskie, Leanne; Lincoln, Alan; Townsend, Jeanne (26 May 2017). "Low-dose suramin in autism spectrum disorder: a small, phase I/II, randomized clinical trial". Annals of Clinical and Translational Neurology. doi:10.1002/acn3.424. PMC 5497533.
External links
- Suramin bound to proteins in the PDB
- Suramin, drug information by JBC Online
- National Cancer Institute