Syringe Services Programs
On This Page
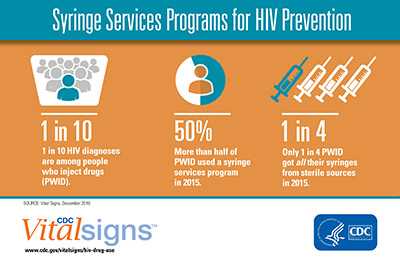
Persons who inject drugs can substantially reduce their risk of getting and transmitting HIV, viral hepatitis and other blood borne infections by using a sterile needle and syringe for every injection. In many jurisdictions, persons who inject drugs can access sterile needles and syringes through syringe services programs (SSPs) and through pharmacies without a prescription. Though less common, access to sterile needles and syringes may also be possible through a prescription written by a doctor and through other health care services.
SSPs, which have also been referred to as syringe exchange programs (SEPs), needle exchange programs (NEPs) and needle-syringe programs (NSPs) are community-based programs that provide access to sterile needles and syringes free of cost and facilitate safe disposal of used needles and syringes. As described in the CDC and U.S. Department of Health and Human Services (HHS) guidance, SSPs are an effective component of a comprehensive, integrated approach to HIV prevention among PWID. These programs have also been associated with reduced risk for infection with hepatitis C virus. Most SSPs offer other prevention materials (e.g., alcohol swabs, vials of sterile water, condoms) and services, such as education on safer injection practices and wound care; overdose prevention; referral to substance use disorder treatment programs including medication-assisted treatment; and counseling and testing for HIV and hepatitis C. Many SSPs also provide linkage to critical services and programs, such as HIV care, treatment, pre-exposure prophylaxis (PrEP), and post-exposure prophylaxis (PEP) services; hepatitis C treatment, hepatitis A and B vaccinations; screening for other sexually transmitted diseases and tuberculosis; partner services; prevention of mother-to-child HIV transmission; and other medical, social, and mental health services.
Federal Funding for SSPs
The Consolidated Appropriations Act of 2016 includes language in Division H, Sec. 520 that gives states and local communities, under limited circumstances, the opportunity to use federal funds to support certain components of SSPs.
To support implementation of this change in law, HHS has released new guidance for state, local, tribal, and territorial health departments that will allow them to request permission to use federal funds to support SSPs. Federal funds can now be used to support a comprehensive set of services, but they cannot be used to purchase sterile needles or syringes for illegal drug injection.
The guidance states that eligible state, local, tribal, and territorial health departments must consult with CDC and provide evidence that their jurisdiction is (1) experiencing, or (2) at risk for significant increases in hepatitis infections or an HIV outbreak due to injection drug use.
After receiving a request for determination of need, CDC will have 30 business days to notify the requestor whether the evidence is sufficient to demonstrate a need for SSPs. When CDC finds there is sufficient evidence, state, local, tribal, and territorial health departments and other eligible HHS grant recipients may then apply to their respective federal agencies to direct funds to support approved SSP activities. Each federal agency (e.g., CDC, HRSA, SAMHSA) is currently developing its own guidance for its funding recipients regarding which specific programs may apply and its application process.
The CDC Program Guidance for Implementing Certain Components of Syringe Services Programs, 2016 provides specific procedures for CDC-funded grantees. The CDC guidance details which SSP activities can be supported with CDC funds, which relevant CDC cooperative agreements can be used to support SSPs, and the process by which CDC-funded programs may request to direct resources to implement new or expand existing SSPs for PWID.
Requesting a Determination of Need for SSPs in Consultation with CDC
On April 27, 2016, CDC hosted a webinar to walk participants through the process of requesting a determination of need for SSPs in consultation with CDC. Participants received practical information and tips for preparing these requests as well as responses to their questions. If interested in requesting a CDC determination of need for SSPs within a jurisdiction, these webinar resources may be helpful to HIV, viral hepatitis, injury, and/or substance abuse prevention surveillance and program staff within health departments.
Download Webinar
Additional Resources
Additional Resources
- Published by the National Alliance of State and Territorial AIDS Directors (NASTAD) and the Urban Coalition for HIV/AIDS Prevention Services (UCHAPS), The Syringe Services Program (SSP) Development and Implementation Guidelines for State and Local Health Departments provide information to assist state and local health departments with planning and implementing SSPs.
- Assessing Local Drug Use provides national, state, and local data sources, reports, publications, surveys, and guides that may be used to assess a community’s need for an SSP.
- Developing, Implementing, and Monitoring Programs provides resources and tools that may be used for developing and implementing SSPs as part of comprehensive, integrated prevention services for PWID.
Info Sheet
Bibliography
CDC. Syringe Service Programs for Persons Who Inject Drugs in Urban, Suburban, and Rural Areas — United States, 2013. MMWR 2015; 64(48);1337-41.
CDC. Integrated Prevention Services for HIV Infection, Viral Hepatitis, Sexually Transmitted Diseases, and Tuberculosis for Persons Who Use Drugs Illicitly: Summary Guidance from CDC and the U.S. Department of Health and Human Services.MMWR 2012; 61(RR05);1-40.
US Department of Health and Human Services, Office of the Secretary. Determination that a demonstration needle exchange program would be effective in reducing drug abuse and the risk of acquired immune deficiency syndrome infection among intravenous drug users. Available at http://www.federalregister.gov/articles/2011/02/23/2011-3990/determination-that-a-demonstration-needle-exchange-program-would-be-effective-in-reducing-drug-abuse. Accessed on January 26, 2016.
Wodak A and Cooney A (2005). Effectiveness of sterile needle and syringe programmes. Int J Drug Policy 16S:S31-44.
Satcher, D. (2000). Evidence-based findings on the efficacy of syringe exchange programs: An analysis of the scientific research completed since April 1998. Washington, DC: US Department of Health and Human Sciences.
FAQ's
GENERAL SSP
1. What are Syringe Services Programs (SSPs)?
SSPs, which have also been referred to as syringe exchange programs (SEPs), needle exchange programs (NEPs) and needle-syringe programs (NSPs) are community-based programs that provide, access to sterile needles and syringes free of cost, facilitate safe disposal of used needles and syringes, and offer safer injection education. Many SSPs also provide linkages to critical services and programs, including substance use disorder treatment programs; overdose prevention education; screening, care, and treatment for HIV and viral hepatitis; HIV pre- and post-exposure prophylaxis (PrEP); prevention of mother-to-child transmission; hepatitis A and hepatitis B vaccination; screening for other sexually transmitted diseases and tuberculosis; partner services; and other medical, social, and mental health services.
2. What are the benefits of SSPs?
Based on existing evidence, the U.S. Surgeon General has determined that SSPs, when part of a comprehensive prevention strategy, can play a critical role in preventing HIV among persons who inject drugs (PWID); can facilitate entry into drug treatment and medical services; and do not increase the unsafe illegal injection of drugs. These programs have also been associated with reduced risk for infection with hepatitis C virus (HCV).
Many SSPs offer other infection prevention materials (e.g., alcohol swabs, vials of sterile water), condoms, and services, such as education on safer injection practices and wound care; overdose prevention; referral to substance use disorder treatment programs including medication-assisted treatment; and counseling and testing for HIV and viral hepatitis. SSPs also provide linkages to other critical services and programs, including screening, care, and treatment for HIV and viral hepatitis, HIV pre- and post-exposure prophylaxis (PrEP), prevention of mother-to-child transmission, hepatitis A and hepatitis B vaccination, screening for other sexually transmitted diseases and tuberculosis, partner services, and other medical, social, and mental health services. SSPs also protect the public and first responders by providing safe needle disposal and by reducing the number of people living with HIV and HCV infections who could transmit those infections to others.
3. Do SSPs increase drug use in a community?
No. Based on existing evidence, the U.S. Surgeon General has determined that SSPs, when part of a comprehensive HIV prevention strategy, do not increase the illegal use of drugs by injection. The opportunity to expand HIV and viral hepatitis prevention services through SSPs will support communities in their efforts to identify and prevent new infections. SSPs are an effective public health intervention that can reduce the transmission of HIV and facilitate entry into drug treatment and medical services, without increasing illegal injection of drugs. SSPs often provide other services important to improving the health of persons who inject drugs (PWID), including referrals to substance use disorder and mental health services, physical health care, social services, overdose prevention and recovery support services. Studies also show that SSPs protect the public and first responders by providing safe needle disposal.
USE OF FEDERAL FUNDS TO SUPPORT SSPs
4. Can federal resources be used to support the implementation of SSPs?
The Consolidated Appropriations Act of 2016includes language in Division H, Sec. 520 that gives states and local communities, meeting certain criteria, the opportunity to use federal funds provided through the Department of Health and Human Services to support certain components of SSPs.
5. What parts of SSPs can federal funding now support?
The change in federal law requires that the health departments where grantees interested in using federal funds for SSPs are located must first consult CDC to determine if there is a need for SSPs. Only after demonstrating the need for SSPs in consultation with CDC may federal funds be used to support various components of SSPs including, but not necessarily limited to, the following:
- Personnel;
- Testing kits for viral hepatitis (HBV and HCV) and HIV;
- Syringe disposal services;
- Navigation services to ensure linkage to HIV and viral hepatitis prevention, treatment and care services including antiretroviral therapy for HCV and HIV; HIV pre- and post-exposure prophylaxis (PrEP), prevention of mother-to-child transmission of HIV and viral hepatitis; hepatitis A and hepatitis B vaccination; substance use disorder treatment, and recovery support services; and medical and mental health services;
- Provision of naloxone to reverse opioid overdoses;
- Educational materials, including information about safer injection practices, overdose prevention and reversing opioid overdose with naloxone, HIV and viral hepatitis prevention, treatment and care services, and mental health and substance use disorder treatment including medication-assisted treatment and recovery support services;
- Condoms to reduce risk of sexual transmission of HIV, viral hepatitis, and other sexually transmitted diseases (STDs);
- Communication activities; and
- Planning and non-research evaluation activities.
Not all of the components listed above will be supported by all participating HHS agencies (i.e., CDC, Health Resource and Services Administration, Substance Abuse and Mental Health Services Administration); use of funding will depend on each HHS agency’s authorities, policies and procedures, as well as state and local laws and regulations.
6. Are there restrictions on what federal funds can support when setting up or expanding an SSP?
Current federal law prohibits the use of federal funds to purchase sterile needles or syringes for the purposes of illegal use of drugs by injection. The Department of Health and Human Services Implementation Guidance to Support Certain Components of Syringe Services Programs, 2016 also specifies that federal funding may not be used for the procurement of other equipment whose only purpose is to prepare drugs for illegal drug injection (e.g., cookers). Programs that use federal funding for SSPs must adhere to federal, state, and local laws, regulations, and other requirements related to such programs or services. SSPs are also subject to the terms and conditions incorporated or referenced in the recipient’s funding agreement.
TWO-STEP PROCESS FOR APPROVAL TO USE FEDERAL FUNDS TO SUPPORT SSPs
7. What is the process for getting approval to use Federal funding to support SSPs?
Federal grantees must follow a two-step process for obtaining approval to use federal funds to start new or expand existing SSPs.
Step 1: State, local, territorial, and tribal health departments must submit a determination of need (DON) request to CDC with data documenting that the jurisdiction is either (1) experiencing or (2) at risk for but not yet experiencing, increases in viral hepatitis infections or an HIV outbreak due to injection drug use. An affirmative determination of need by CDC can then be used to justify the use of federal funds from CDC, HRSA and SAMHSA.
- On March 31, HHS released the Implementation Guidance to Support Certain Components of Syringe Services Programs, 2016 which outlines what SSP activities can now be supported and how state, local, territorial, and tribal communities should consult with CDC to demonstrate their need for these programs.
Step 2: Health departments and other grantees must follow agency-specific guidance, and work with their project officers to request funds to support SSPs.
- On April 27, CDC released the Program Guidance for Implementing Certain Components of Syringe Services Programs, 2016 which provides specific procedures for CDC-funded grantees.
- Other HHS guidance
Implementation Guidance to Support Certain Components of SSPs
1. What is the purpose of the Department of Health and Human Services (HHS) Implementation Guidance to Support Certain Components of SSPs, 2016?
The purpose of this document is to provide implementation guidance for programs directly funded by HHS interested in implementing or expanding SSPs for PWID.
2. What is a determination of need (DON) request?
Prior to directing federal funds to SSPs, federal law requires jurisdictions to demonstrate need for SSPs in consultation with CDC. As part of the consultation with CDC, state, local, territorial, and tribal health departments should submit to CDC evidence in a DON request that includes data indicating whether the jurisdiction is either (1) experiencing or (2) at risk for, significant increases in viral hepatitis infections or an HIV outbreak due to injection drug use. The scope of the evidence should address the geographic area that will be served by the SSPs and include county, city, and state level data, as appropriate.
Within 30 business days after receipt of the DON request, CDC will notify the requestor whether the evidence is sufficient to demonstrate need for SSPs. If the evidence is sufficient, the state, local, territorial, or tribal health department will receive a Notice of Approval regarding DON for the jurisdiction. This notice may be used by the state, local, territorial, or tribal health department or other eligible HHS recipients (as identified by each federal agency) to apply to the respective federal agency for use of federal funds. If the evidence is insufficient, no programmatic or budgetary changes will be authorized. However, jurisdictions may choose to revise and resubmit their request with additional evidence based on feedback from CDC.
3. Who can submit a determination of need (DON) request?
State, local, territorial, and tribal health departments can submit a DON request to CDC. Health departments should specify the geographic area (e.g., county or counties, metropolitan statistical area, etc.) for which a determination is being requested. Local health departments are encouraged to coordinate with their state health department, as states can submit a request for multiple jurisdictions in their state. It is important to note that if only one jurisdiction within a state has a need, the results of the CDC consultation will apply to that one jurisdiction and any new need in other geographic areas would require a new consultation with CDC. However, if multiple jurisdictions within a state have a need, the state health department can request a CDC DON for the entire state. If the result of the CDC consultation applies to the entire state, no new determinations for jurisdictions within a state would be needed to use federal funds for SSP programs in the future.
4. How does a state/municipality demonstrate that it needs SSPs?
Health departments need to submit data to CDC indicating the jurisdiction is either (1) experiencing or (2) at risk for but not yet experiencing increases in viral hepatitis or an HIV outbreak due to injection drug use. The information provided to CDC should specify: outcomes analyzed, data sources, geographic area covered, assessment period (beginning year/date to end year/date), type of measure (e.g., number, rate), and absolute and/or relative percent increase during the assessment period. An affirmative determination of need (DON) by CDC can then be used to justify the use of federal funds from CDC and other federal agencies. If the SSP is expected to serve multiple neighboring jurisdictions or if multiple jurisdictions within a state are at risk, data from multiple jurisdictions should be presented.
5. Who at CDC will be reviewing determination of need (DON) requests?
A CDC panel of HIV, viral hepatitis, and injury staff with expertise in epidemiology and surveillance will review the data provided by each jurisdiction and determine whether the evidence is sufficient to demonstrate need for SSPs.
6. What criteria will be used by CDC when reviewing determination of need (DON) requests?
CDC will examine the data provided by each jurisdiction and base their determination of need for SSPs on whether the jurisdiction:
- Provided sufficient evidence to demonstrate that the jurisdiction is experiencing increases in viral hepatitis or HIV infections due to injection drug use.
- State, local, territorial or tribal health departments may provide multi-year surveillance data that demonstrate an increase in acute HCV, HBV, or HIV infections along with mode of transmission data, if available
- Provided sufficient evidence to demonstrate that the jurisdiction is at risk for increases in viral hepatitis or HIV infections due to injection drug use.
- Health departments may provide data from multiple sources that, when triangulated (combined), provide compelling evidence that there is likely an increase in injection drug use in the jurisdiction that could lead to new viral hepatitis and HIV infections. Examples of this evidence may come from many sources, such as existing SSP programs, arrest data, healthcare utilization data, or local drug treatment data.
7. How long will it take CDC to review determination of need (DON) requests?
Within 30 business days after receipt, CDC will notify the requestor whether the evidence is sufficient to demonstrate need for SSPs. If the evidence is sufficient, the state, local, territorial, or tribal health department will receive notice of approval regarding determination of need for the jurisdiction. This notice may be used by the health department to apply for federal funds to support SSPs. If the evidence is insufficient, no programmatic or budgetary changes will be authorized. However, jurisdictions may choose to revise and resubmit their request with additional evidence based on feedback from CDC.
8. Can CDC help us assess our need for SSPs, including reviewing our data?
Initially, health departments should gather the data available to them and internally assess whether this data indicates possible increases in viral hepatitis or HIV infections due to injection drug use, or increases in injection drug use. They should interpret these data within the context of local surveillance practices, disease patterns and long-term trends. If state, territorial, or tribal health departments have additional questions, they can submit questions or requests for additional technical assistance to the SSP coordinator mailbox provided in the HHS guidance (sspcoordinator@cdc.gov). Local health departments should request technical assistance from their state health department before contacting CDC for technical assistance.
9. What technical assistance is available to help areas with their determination of need (DON) requests?
CDC provided many detailed examples and suggested data sources in the HHS guidance. Initially, health departments should gather the data available to them and internally assess whether this data indicates possible increases in viral hepatitis or HIV infections due to injection drug use, or increases in injection drug use. They should interpret this data within the context of local surveillance practices, disease patterns and long-term trends. If state, territorial, or tribal health departments have additional questions, they can submit questions or requests for additional technical assistance to the SSP coordinator mailbox provided in the HHS guidance (sspcoordinator@cdc.gov). Local health departments should request technical assistance from their state health department.
10. After a determination of need (DON) is issued, what are the next steps for requesting to use funds for SSPs?
When CDC concurs with a DON request, the notice of approval can then be used to justify the use of federal funds from CDC and other federal agencies. State, local, territorial and tribal health departments will then need to follow agency-specific guidance to request funds to support SSPs. While no additional resources have been identified to support SSPs specifically, states may have some flexibility in how they target their existing resources.
11. If CDC concurs with a determination of need (DON) request for SSPs, how long does that concurrence remain valid?
CDC’s concurrence with a determination of need for SSPs in a certain jurisdiction remains valid while the existing law that permits the use of Federal funds for certain components of SSPs is in effect.[1] As with vaccination programs that remain in communities even after there is a reduction in infections due to these efforts, SSPs should remain in communities as long as injection drug use continues.
CDC Program Guidance for Implementing SSPs
1. What is the purpose of the CDC Program Guidance for Implementing SSPs?
The purpose of CDC Program Guidance for Implementing Certain Components of Syringe Services Programs, 2016 is to provide specific procedures for CDC-funded grantees. The CDC guidance details which SSP activities can be supported with CDC funds, which relevant CDC cooperative agreements can be used to support SSPs, and the process by which CDC-funded programs may request to direct resources to implement new or expand existing SSPs for PWID.
2. What is the process for requesting use of CDC funds for SSPs?
After obtaining CDC notification that the jurisdiction has sufficiently demonstrated need to use federal funding for SSP activities, CDC directly-funded state and/or local health departments, or other eligible entities, should discuss plans to direct funds to SSP activities with their CDC project officer. Local health departments, who are not directly funded by CDC, must work with CDC directly-funded state and/or local health departments to request program funding to support SSPs.
In accordance with CDC Office of Grant Services (OGS) guidelines, jurisdictions must then prepare a proposal that identifies the SSP activities that will be supported by CDC funds. The proposal should include: 1) a proposed program plan and 2) a revised budget. For all grantees, the proposal, including the proposed program plan and revised budget, must be submitted to OGS with a courtesy copy to the CDC project officer. Once approved by both the OGS Grants Management Specialist and the CDC Project Officer, the requestor will receive a revised Notice of Award signed by the OGS Grants Management Officer. Grantees must obtain this approval before using their awarded funding to implement any SSP activities.
CDC will then approve or disapprove requests to direct funding to support SSPs activities within 30 business days upon receipt of all requested information. After request approval, CDC will work in partnership with grantees to determine the appropriate process measures to capture for SSPs.
3. What needs to be included in requests to use CDC funds to support SSPs?
CDC grantees cannot request that funds be directed to support SSP activities unless the jurisdictional health department has first demonstrated the need for SSPs, in consultation with CDC, and received a notice of approval from the CDC SSP Review Panel. During the processes of requesting either: 1) determination of need or 2) directing CDC funds to support SSPs, grantees should contact their project officers to discuss specific capacity building and technical assistance needs and, if needed, submit a request(s) for additional technical assistance or training. All proposals to request the use of CDC funds to support SSPs should include the following elements, unless otherwise noted:
- CDC’s notice of approval that the jurisdiction has sufficiently demonstrated need to use federal funding for SSP activities;
- Description of proposed new or expanded SSP related activities;
- Timeline for implementation;
- Impact on current activities funded under the respective funding opportunity announcement (FOA);
- Copy of existing protocols and guidelines for SSP related activities, if available;
- Budget and budget justification, proposed activities and measures;
- Description of current training and technical assistance needs related to planning, implementing, and evaluating SSPs, as appropriate; and
- Location of SSP-related activities to be supported with federal funds.
4. Can any CDC FY 2016 grant or cooperative agreement funding be used to support SSP activities?
No, currently, only funds awarded through the following FOAs can be used to support SSPs:
- PS12-1201 – Comprehensive HIV Prevention Programs for Health Departments
- PS14-004 – Reduce Hepatitis Infections by Treatment and Integrated Prevention Services (Hepatitis-TIPS) among Non-urban Young Persons Who Inject Drugs Future FOAs will contain language specifying if SSP efforts can be supported with funding from that specific FOA.
Additionally, before funding can be used, proposed SSP activities must be included in an approved program plan and budget.
5. Have additional resources been identified to help communities fund SSPs?
No. While no additional resources have been identified to support SSPs specifically, states health departments have some flexibility in how they target their existing resources and should direct their funding and programmatic activities/strategies to the areas and populations with the greatest need in their states/locales.
6. If a jurisdiction (county, city, state, etc.) wants to discuss the potential need for and benefits of SSPs, who is the primary point of contact in the state’s department of health?
Entities seeking information about the potential needs for and benefits of SSPs in their jurisdiction should contact their state HIV and viral hepatitis coordinator(s). For jurisdictions where CDC has been consulted and concurred that need exists, the point of contacts can be found at www.cdc.gov/hiv/risk/ssps-jurisdictions.html.
7. How do we know if injection drug use (IDU) is on the rise and that the risk of HBV, HCV or HIV infection among persons who inject drugs (PWID) is increasing in our state or municipality?
1. To best assess if unsafe injection drug use is occurring in your jurisdiction, examine all national and local data sources available to you that are either known or may reasonably be associated with unsafe (non-sterile) illegal injection of drugs. Such data sources include, but are not limited to, the following:
- Drug overdose deaths (especially opioid-related)
- Access to prescription opioids (e.g., production, sales, prescriptions)
- Access to care related to illegal injection of drugs (e.g., data on the use of care and treatment services for drug overdose or intoxication related to injectable drugs)
- Demand for medication-assisted therapy (e.g., methadone, buprenorphine, naltrexone)
- The six variables used in CDC’s national analysis (Percent White, Non-Hispanic Population; Drug Overdose Deaths per 100K Persons; Per Capita Income; Percent Unemployed Population; Prescription Opioid Sales per 10K; Buprenorphine Prescribing Potential by Waiver per 10K Persons)
- EMS calls for drug overdose;
- Arrests for drug possession or sales
- Arrests for possession of needles, syringes, or other drug paraphernalia;
- Population surveys assessing prevalence of IDU;
- State prescription drug monitoring plan data to identify for hot spots of prescribed opioids;
- Rates of endocarditis or skin and soft tissue infections; and
- Medical examiner and toxicology records.
2. To improve sensitivity to changes in rates of infection that may represent an outbreak and to identify people who need care and treatment, enhance testing for HBV, HCV, and HIV infections among PWID. Focus especially on the following settings: providers of drug treatment services, jails and prisons, emergency departments, and community health centers. High-risk individuals should be tested at regular intervals and should be interviewed to monitor on-going risk.
8. What should we do if injection drug use (IDU) is on the rise and the risk of HBV, HCV or HIV infection among persons who inject drugs (PWID) is increasing in our state or municipality?
To improve sensitivity to changes in rates of infection that may represent an outbreak and to identify people who need care and treatment, enhance testing for HBV, HCV, and HIV infections among PWID, focusing especially on the following settings: providers of drug treatment services, jails and prisons, emergency departments, and community health centers. High risk individuals should be tested at regular intervals and should be interviewed to monitor on-going risk.
- To reduce overall disease burden and to reduce the risk of onward transmission of infections, refer all persons diagnosed with HBV, HCV, or HIV infection to appropriate care and treatment; refer high-risk negatives to appropriate prevention counseling and to services (e.g., drug treatment facilities, vaccination for HBV).
- To reduce unsafe illegal injection of drugs,
- Institute or expand existing syringe services programs as permitted by state or other local law;
- Increase the number of providers able to prescribe medication–assisted therapy in the jurisdiction;
- Increase the availability of in-patient treatment for substance use disorder; and
- Educate PWID about the risks of HBV, HCV, and HIV infection associated with unsafe illegal injection of drugs.
For further information please open the following webinar:
9. What technical resources are available to help operationalize and implement an SSP?
CDC has identified tools and resources for health departments and local partners in developing, implementing, and monitoring SSPs. These materials provide:
- Examples to consider in planning, designing, and implementing SSPs in each jurisdiction as part of a comprehensive, integrated approach to prevention of HIV, viral hepatitis, and other injection-related harms among PWID.
- National and international guidelines.
- Sources for technical assistance and program supplies.
- Strategies for working with law enforcement and for building strong community relationships.
- Tools to guide monitoring and evaluation of comprehensive prevention programs for PWID, including SSPs.
For those needing technical or capacity building assistance, Capacity Building Assistance (CBA) providers with expertise in the implementation of SSPs have been identified to support SSP-related capacity building and technical assistance request
[1] The Consolidated Appropriations Act of 2016 includes language in Division H, Sec. 520 that gives states and local communities, under limited circumstances, the opportunity to use federal funds provided through the Department of Health and Human Services to support certain components of SSPs.
- Page last reviewed: September 28, 2017
- Page last updated: September 28, 2017
- Content source: Division of HIV/AIDS Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, Centers for Disease Control and Prevention


 ShareCompartir
ShareCompartir