HIV Among Gay and Bisexual Men
Fast Facts
- Gay, bisexual, and other men who have sex with mena account for 70% of new HIV infections in the United States.
- New HIV infections among gay and bisexual men overall remained stable in recent years.
- More than 600,000 gay and bisexual men are living with HIV in the United States.

In 2014, gay and bisexual men made up an estimated 2% of the U.S. population, but accounted for 70% of new HIV infections. Approximately 492,000 sexually active gay and bisexual men are at high risk for HIV; however, we have more tools to prevent HIV than ever before.
The Numbers
HIV Infectionsb
In 2014, gay and bisexual men accounted for an estimated 70% (26,200) of new HIV infections in the United States.
From 2010 to 2014, estimated annual HIV infections remained stable at about 26,000 per year among all gay and bisexual men. However, trends varied by age and race/ethnicity. Estimated HIV infections
- Declined 16% among gay and bisexual men aged 13 to 24.
- Increased 23% among gay and bisexual men aged 25 to 34.
- Declined 16% among gay and bisexual men aged 35 to 44.
- Declined 11% among white gay and bisexual men.
- Increased 14% among Hispanic/Latinoc gay and bisexual men.
- Remained stable among black or African Americand gay and bisexual men, at about 10,000 per year.
HIV and AIDS Diagnosese
In 2015:
- Gay and bisexual men accounted for 82% (26,376) of new HIV diagnoses among all males aged 13 and older and 67% of the total new diagnoses in the United States.f
- Gay and bisexual men aged 13 to 24 accounted for 92% of new HIV diagnoses among all men in their age group and 27% of new diagnoses among all gay and bisexual men.
- Gay and bisexual men accounted for 55% (10,047) of people who received an AIDS diagnosis. Of those men, 39% were African American, 31% were white, and 24% were Hispanic/Latino.
From 2010 to 2014:
- HIV diagnoses remained stable at about 26,000 per year among all gay and bisexual men.
- After years of increases, diagnoses stabilized among young (aged 13-24) African American and white gay and bisexual men. Diagnoses increased 14% among young Hispanic/Latino gay and bisexual men.
HIV Diagnoses Among the Most-Affected Subpopulations, 2015—United States
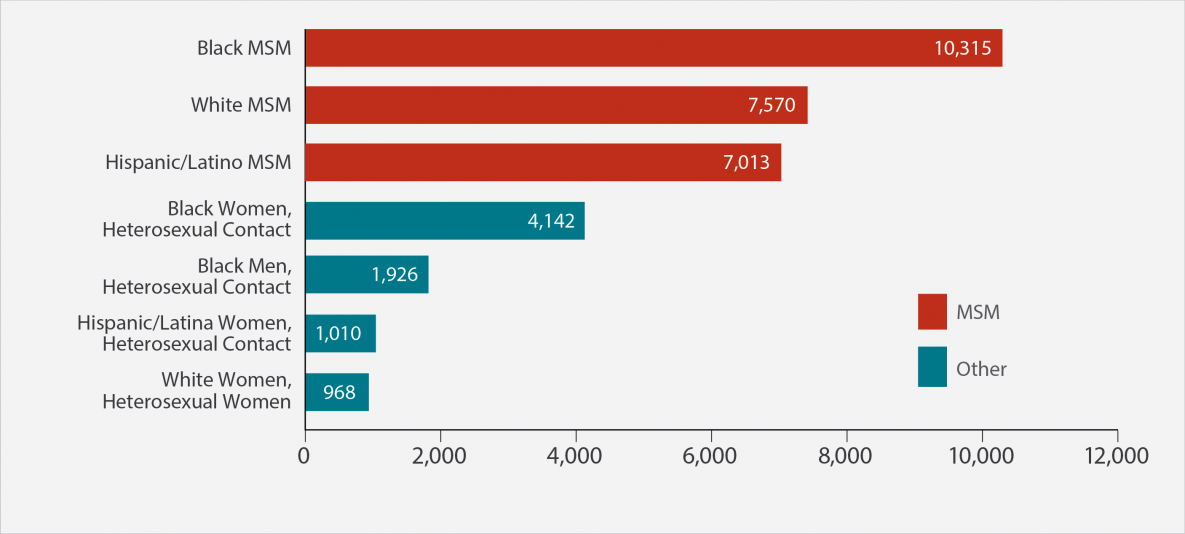
Subpopulations representing 2% or less of HIV diagnoses are not reflected in this chart.
Abbreviation: MSM=men who have sex with men.
Living With HIV and Deaths
- At the end of 2014, an estimated 615,400 gay and bisexual men were living with HIV. Of those, 17.3% were unaware of their infection.
- Among all gay and bisexual men living with HIV in 2014, 83% had received a diagnosis, 61% received HIV medical care in 2014, 48% were receiving continuous HIV care, and 51% had a suppressed viral load.g A person living with HIV who gets and stays virally suppressed can stay healthy and has effectively no risk of sexually transmitting HIV to HIV-negative partners.
- In 2014, there were 6,110 deaths among gay and bisexual men living with diagnosed HIV infection.h
Prevention Challenges
- A much higher proportion of gay and bisexual men are living with HIV compared to any other group in the United States. Therefore gay and bisexual men have an increased chance of having an HIV-positive partner.
- 1 in 6 gay and bisexual men living with HIV are unaware they have it. People who don’t know they have HIV cannot get the medicines they need to stay healthy and prevent transmitting HIV to their partners. Therefore, they may transmit the infection to others without knowing it.
- Most gay and bisexual men get HIV through having anal sex without condoms or medicines to prevent or treat HIV. Anal sex is the riskiest type of sex for getting or transmitting HIV. Receptive anal sex is 13 times as risky for getting HIV as insertive anal sex.
- Gay and bisexual men are also at increased risk for other sexually transmitted diseases (STDs), like syphilis, gonorrhea, and chlamydia. Condoms can protect from some STDs, including HIV.
- Homophobia, stigma, and discrimination may place gay and bisexual men at risk for multiple physical and mental health problems and affect whether they take protective actions with their partners or seek and are able to obtain high-quality health services.
What CDC Is Doing
CDC funds health departments and other community-based organizations (CBOs) to support HIV prevention services for gay and bisexual men. For example,
- Under the current funding opportunity, CDC has awarded at least $330 million per year to health departments to direct resources to the populations and geographic areas of greatest need and prioritize the HIV prevention strategies that will have the greatest impact. A new notice of funding opportunity (NOFO) will begin in 2018.
- In 2017, CDC awarded nearly $11 million per year for 5 years to 30 CBOs to provide HIV testing to young gay and bisexual men of color and young transgender persons of color, with the goals of identifying undiagnosed HIV infections and linking those who have HIV to care and prevention services.
- In 2015, CDC added three new NOFOs to help health departments reduce HIV infections and improve HIV medical care among gay and bisexual men.
- Targeted Highly Effective Interventions to Reverse the HIV Epidemic (THRIVE) supports state and local health department demonstration projects to develop community collaborations that provide comprehensive HIV prevention and care services for MSM of color.
- Training and Technical Assistance for THRIVE strengthens the capacity of funded health departments and their collaborative partners to plan, implement, and sustain (through ongoing engagement, assessment, linkage, and retention) comprehensive prevention, care, behavioral health, and social services models for MSM of color at risk for and living with HIV infection.
- Project PrIDE (PrEP, Implementation, Data2Care, and Evaluation) supports 12 health departments in implementing PrEP and Data to Care demonstration projects for gay and bisexual men of color.
CDC supports biomedical approaches to HIV prevention. People at very high risk for HIV can take HIV medicines daily (PrEP) to greatly reduce the chances that they will get HIV. Post-exposure prophylaxis (PEP), which means taking HIV medicines soon after possible exposure to HIV, also plays a role in HIV prevention, but should be not be considered a primary means of prevention.
Through its Act Against AIDS campaigns and partnerships, CDC provides gay and bisexual men with effective and culturally appropriate messages about HIV prevention and treatment. For example,
- Doing It, a national HIV testing and prevention campaign, encourages all adults to know their HIV status and make HIV testing a part of their regular health routine.
- Start Talking. Stop HIV. helps gay and bisexual men communicate about safer sex, testing, and other HIV prevention issues.
- HIV Treatment Works shows how people living with HIV have overcome barriers to stay in care and provides resources on how to live well with HIV.
- Partnering and Communicating Together (PACT) to Act Against AIDS, a 5-year partnership with organizations such as AIDS United and the National Lesbian & Gay Journalists Association, is raising awareness about testing, prevention, and retention in care among populations disproportionately affected by HIV, including gay and bisexual men.
To learn more about a range of health issues affecting gay and bisexual men, visit the CDC Gay and Bisexual Men’s Health site.
a The term male-to-male sexual contact is used in CDC surveillance systems. It indicates a behavior that transmits HIV infection, not how individuals self-identify in terms of their sexuality. This fact sheet uses the term gay and bisexual men.
bEstimated annual HIV infections are the estimated number of new infections (HIV incidence) that occurred in a particular year, regardless of when those infections were diagnosed.
c Hispanics/Latinos can be of any race.
d Referred to as African American in this fact sheet.
eHIV and AIDS diagnoses refers to the number of people with HIV infection and AIDS diagnosed during a given time period, not when the people were infected.
f The numbers reported in this fact sheet include infections attributed to male-to-male sexual contact only, not those attributed to male-to-male sexual contact and injection drug use.
g Viral suppression is defined as having fewer than 200 copies of the virus per milliliter of blood on the most recent viral load test in 2014. Receiving continuous HIV care is defined as having two viral load or CD4 tests 3 or more months apart in 2014. (CD4 cells are the cells in the body’s immune system that are destroyed by HIV.)
h Deaths may be due to any cause.
Bibliography
- Diagnoses of HIV infection in the United States and dependent areas, 2015. HIV Surveillance Report 2016;27.
- High-impact HIV prevention: CDC’s approach to reducing HIV infections in the United States. Accessed September 19, 2017.
- HIV incidence: Estimated annual infections in the U.S., 2008-2014 [fact sheet]. Accessed September 19, 2017.
- HIV infection risk, prevention, and testing behaviors among men who have sex with men—National HIV Behavioral Surveillance, 20 U.S. cities, 2014. HIV Surveillance Special Report 2016;15.
- HIV prevention modeling study [press release]. Accessed September 19, 2017.
- HIV testing experience before HIV diagnosis among men who have sex with men—21 Jurisdictions, United States, 2007–2013. MMWR 2016;65(37):999-1003.
- Lifetime risk of HIV diagnosis [press release]. Accessed September 19, 2017.
- Monitoring selected national HIV prevention and care objectives by using HIV surveillance data—United States and 6 dependent areas, 2015. HIV Surveillance Supplemental Report 2017;22(2).
- New HIV infections drop 18 percent in six years [press release]. Accessed September 19, 2017.
- Trends in U.S. HIV diagnoses, 2005-2014 [fact sheet]. Accessed September 19, 2017.
- Kwan CK, Rose CE, Brooks JT, Marks G, Sionean C. HIV testing among men at risk for acquiring HIV infection before and after the 2006 CDC recommendations. Public Health Rep 2016;131:311-9. PubMed abstract.
- Purcell D, Johnson CH, Lansky A, et al. Estimating the population size of men who have sex with men in the United States to obtain HIV and syphilis rates. Open AIDS J 2012;6(Suppl 1: M6):98-107.
- Wejnert C, Le B, Rose CE, et al. HIV infection and awareness among men who have sex with men–20 Cities, United States, 2008 and 2011. PLoS One 2013;8(10).
Fact Sheets
Other Resources
Web Sites
- Gay and Bisexual Men’s Health
- Lesbian, Gay, Bisexual, and Transgender Health
- Positive Spin
- National Gay Men’s HIV/AIDS Awareness Day
- National Black HIV/AIDS Awareness Day
General Resources
- CDC-INFO 1-800-CDC-INFO (232-4636)
- CDC HIV Website
- CDC Act Against AIDS Campaign
- CDC HIV Risk Reduction Tool (BETA)
- Page last reviewed: September 27, 2017
- Page last updated: September 27, 2017
- Content source: Division of HIV/AIDS Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, Centers for Disease Control and Prevention


 ShareCompartir
ShareCompartir