HIV Among Women
Fast Facts
- Around a quarter of people living with HIV in the United States are women.
- Most HIV diagnoses in women are attributed to heterosexual sex.
- The annual number of HIV diagnoses among women has declined in recent years.
 Though HIV diagnoses among women have declined sharply in recent years, more than 7,000 women received an HIV diagnosis in 2015. Black/African Americana women are disproportionately affected by HIV, compared with women of other races/ethnicities. Of the total number of womenb living with diagnosed HIV at the end of 2014, 60% (139,058) were African American, 17% (39,343) were white, and 17% (40,252) were Hispanic/Latina.c
Though HIV diagnoses among women have declined sharply in recent years, more than 7,000 women received an HIV diagnosis in 2015. Black/African Americana women are disproportionately affected by HIV, compared with women of other races/ethnicities. Of the total number of womenb living with diagnosed HIV at the end of 2014, 60% (139,058) were African American, 17% (39,343) were white, and 17% (40,252) were Hispanic/Latina.c
The Numbers
HIV and AIDS Diagnosesd
- Women made up 19% (7,402) of the 39,513 new HIV diagnoses in the United States in 2015.
- Overall, 86% (6,391) of HIV diagnoses among women were attributed to heterosexual sex,e and 13% (980) were attributed to injection drug use. But among white women, 32% of HIV diagnoses were attributed to injection drug use.
- Among all women with HIV diagnosed in 2015, 61% (4,524) were African American, 19% (1,431) were white, and 15% (1,131) were Hispanic/Latina.
- Annual HIV diagnoses declined 20% among women from 2010 to 2014. They declined 24% among African American women, 16% among Hispanic/Latina women, and 9% among white women.
- Women accounted for 24% (4,459) of the 18,303 AIDS diagnoses in 2015 and represent 20% (248,270) of the 1,216,917 cumulative AIDS diagnoses in the United States from the beginning of the epidemic through the end of 2015.
HIV Diagnoses in the United States for the Most-Affected Subpopulations, 2015
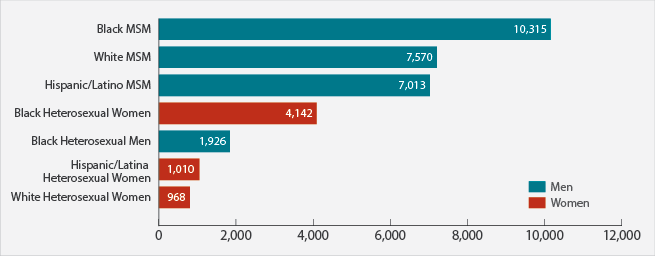
Source: CDC. Diagnoses of HIV infection in the United States and dependent areas, 2015. HIV Surveillance Report 2016;27. Subpopulations representing 2% or less of HIV diagnoses are not reflected in this chart. Abbreviation: MSM = men who have sex with men.
Living With HIV and Deaths
- An estimated 287,400 women were living with HIV at the end of 2013, representing 23% of all Americans living with the virus. Of women living with HIV, around 11% do not know they are infected.
- Of women diagnosed with HIV in 2014, 76% were linked to HIV medical care within 1 month.f
- Of women diagnosed with HIV in 2012 or earlier, 57% were retained in care (receiving continuous HIV medical care) at the end of 2013, and 52% had achieved viral suppression.g
- In 2014, 1,783 women died from HIV or AIDS.
Prevention Challenges
- The greater number of people living with HIV (prevalence) in African American and Hispanic/Latino communities and the fact that people tend to have sex with partners of the same race/ethnicity result in women from these communities facing a greater risk of HIV infection with each new sexual encounter.
- Because some women may be unaware of their male partner’s risk factors for HIV (such as injection drug use or having sex with men), they may not use condoms.
- Assuming no prevention methods (such as condoms or medicines to prevent HIV) are used, women have a higher risk for getting HIV during vaginal sex than men do. The riskiest behavior for getting HIV is receptive anal sex. In a behavioral survey of heterosexual women at increased risk of HIV infection, 92% of HIV-negative women reported having vaginal sex without a condom in the previous year, and 25% reported having anal sex without a condom.
- Some sexually transmitted diseases, such as gonorrhea and syphilis, greatly increase the likelihood of getting or transmitting HIV.
- Women who have been sexually abused may be more likely than women who have not to engage in sexual risk behaviors like exchanging sex for drugs, having multiple sex partners, or having sex without a condom.
What CDC Is Doing
 Through its high-impact prevention approach, CDC is working with state and local partners throughout the United States to identify and implement the most cost-effective and scalable interventions in the geographic areas and populations most affected by HIV. Activities include:
Through its high-impact prevention approach, CDC is working with state and local partners throughout the United States to identify and implement the most cost-effective and scalable interventions in the geographic areas and populations most affected by HIV. Activities include:
- Funding to health departments and community-based organizations:
- Starting in 2012, CDC has awarded at least $330 million each year ($343.7 million in 2015) to health departments to direct resources to the populations and geographic areas of greatest need and prioritize the HIV prevention strategies that will have the greatest impact.
- CDC is awarding approximately $130 million over 5 years (2014-2019) to provide training and technical assistance for staff of health departments, community-based organizations, and health care organizations to help them link HIV-positive people to care, retain or reengage them in care, and help them achieve viral suppression.
- The Act Against AIDS campaigns and partnerships, including
- Doing It, a national HIV testing and prevention campaign that encourages all adults to know their HIV status and protect themselves and their community by making HIV testing a part of their regular health routine;
- Let’s Stop HIV Together, which raises HIV awareness and fights stigma among all Americans and provides many stories about people living with HIV;
- HIV Treatment Works, a campaign that features people from across the United States who are living with HIV talking about how sticking with care and treatment helps them stay healthy, protect others, and live longer, healthier lives; and
- Partnering and Communicating Together (PACT) to Act Against AIDS, a 5-year partnership between CDC and leading national organizations representing the populations hardest hit by HIV and AIDS, to intensify HIV prevention efforts in these populations.
- Research on microbicides—creams or gels that could be applied vaginally or anally before sexual contact to prevent HIV transmission.
- Support and technical assistance to health departments and community-based organizations to deliver effective behavioral interventions.
a Referred to as African American in this fact sheet.
b Adult and adolescent females aged 13 and older.
c Hispanics/Latinas can be of any race.
d HIV and AIDS diagnoses indicate when a person is diagnosed with HIV infection or AIDS, but do not indicate when the person was infected.
e Heterosexual sex with a person known to have, or be at high risk for, HIV infection.
f In 32 states and the District of Columbia (the areas with complete lab reporting by December 2015).
g A person with a suppressed viral load has a very low level of the virus. That person can stay healthy and has a dramatically reduced risk of transmitting the virus to others.
Additional Resources
Bibliography
- CDC. Diagnoses of HIV infection in the United States and dependent areas, 2015. HIV Surveillance Report 2015;27. Accessed January 6, 2017.
- CDC. Deaths: Final Data for 2014. National Vital Statistics Reports 2016;65(4). Accessed January 6, 2017.
- CDC. HIV infection, risk, prevention, and testing behaviors among heterosexuals at increased risk of HIV infection—National HIV Behavioral Surveillance, 20 U.S. cities, 2013. HIV Surveillance Special Report 13. Accessed January 6, 2017.
- CDC. Monitoring selected national HIV prevention and care objectives by using HIV surveillance data—United States and 6 dependent areas—2014. HIV Surveillance Supplemental Report 2016;21(4). Accessed January 6, 2017.
- Moreno CL. The relationship between culture, gender, structural factors, abuse, trauma, and HIV/AIDS for Latinas. Qual Health Res 2007;17(3):340-54. PubMed abstract. Accessed January 6, 2017.
- Crosby RA, DiClemente RJ, Wingood GM, Salazar LF, Head S, Rose E, McDermott-Sales J. Sexual agency versus relational factors: a study of condom use antecedents among high-risk young African American women. Sex Health 2008;5(1):41-7. PubMed abstract. Accessed January 6, 2017.
- Herbenick D, Reece M, Schick V, Sanders SA, Dodge B, Fortenberry JD. Sexual behavior in the United States: results from a national probability sample of men and women ages 14-94. J Sex Med 2010;7 Suppl 5:255-65. PubMed abstract. Accessed January 6, 2017.
- CDC. Sexually transmitted diseases surveillance 2013. Accessed January 6, 2017.
- Simoni JM, Sehgal S, Walters KL. Triangle of risk: urban American Indian women’s sexual trauma, injection drug use, and HIV sexual risk behaviors. AIDS Behav 2004;8(1):33-45. PubMed abstract. Accessed January 6, 2017.
- Cavanaugh CE, Hansen NB, Sullivan TP. HIV sexual risk behavior among low-income women experiencing intimate partner violence: the role of posttraumatic stress disorder. AIDS Behav 2010;14(2):318-27. Accessed January 6, 2017.
- Mosack KE, Randolph ME, Dickson-Gomez J, Abbott M, Smith E, Weeks MR. Sexual risk-taking among high-risk urban women with and without histories of childhood sexual abuse: mediating effects of contextual factors. J Child Sex Abus 2010;19(1):43-61. Accessed January 6, 2017.
- Coker AL. Does physical intimate partner violence affect sexual health? A systematic review. Trauma Violence Abuse 2007;8(2):149-77. PubMed abstract. Accessed January 6, 2017.
- Bauer HM, Gibson P, Hernandez M, Kent C, Klausner J, Bolan G. Intimate partner violence and high-risk sexual behaviors among female patients with sexually transmitted diseases. Sex Transm Dis 2002;29(7):411-6. PubMed abstract. Accessed January 6, 2017.
- Tross S, Hanner J, Hu MC, Pavlicova M, Campbell A, Nunes EV. Substance use and high risk sexual behaviors among women in psychosocial outpatient and methadone maintenance treatment programs. Am J Drug Alcohol Abuse 2009;35(5):368-74. PubMed abstract. Accessed January 6, 2017.
- Dinenno EA, Oster AM, Sionean C, Denning P, Lansky A. Piloting a system for behavioral surveillance among heterosexuals at increased risk of HIV in the United States. Open AIDS J 2012;6:169-76. Accessed January 6, 2017.
Fact Sheets
Other Resources
Organizations
AIDS Alliance for Children, Youth, & Families
Mother to Child Transmission Resources (AIDS Education and Training Centers)
Black Women and HIV/AIDS (National Alliance of State and Territorial AIDS Directors)
HIV/AIDS (womenshealth.gov)
Women, Children, and HIV (University of California, San Francisco)
Cervical Cancer and HIV (SmartGlobalHealth.org)
- Page last reviewed: March 10, 2017
- Page last updated: March 10, 2017
- Content source: Division of HIV/AIDS Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, Centers for Disease Control and Prevention


 ShareCompartir
ShareCompartir