HIV Among American Indians and Alaska Natives in the United States
Fast Facts
- HIV affects AIs/ANs in ways that are not always obvious because of their small population sizes.
- Over the last decade, annual diagnoses increased 63% among AI/AN gay and bisexual men.
- AIs/ANs face HIV prevention challenges, including poverty, high rates of STIs, and stigma.
 HIV is a public health issue among American Indians and Alaska Natives (AIs/ANs), who represent about 1.2%a of the U.S. population. Overall, diagnosed HIV infections among AIs/ANs are proportional to their population size. Compared with other racial/ethnic groups, AIs/ANs ranked fifth in rates of HIV diagnoses in 2015, with a lower rate than blacks/African Americans, Hispanics/Latinos,b Native Hawaiians/Other Pacific Islanders, and people reporting multiple races, but a higher rate than Asians and whites.
HIV is a public health issue among American Indians and Alaska Natives (AIs/ANs), who represent about 1.2%a of the U.S. population. Overall, diagnosed HIV infections among AIs/ANs are proportional to their population size. Compared with other racial/ethnic groups, AIs/ANs ranked fifth in rates of HIV diagnoses in 2015, with a lower rate than blacks/African Americans, Hispanics/Latinos,b Native Hawaiians/Other Pacific Islanders, and people reporting multiple races, but a higher rate than Asians and whites.
The Numbers
HIV and AIDS Diagnosesc
- Of the 39,513 HIV diagnoses in the United States in 2015, 1% (209) were among AIs/ANs. Of those, 73% (152) were men and 26% (55) were women.
- Of the 152 HIV diagnoses among AI/AN men in 2015, most (79%; 120) were among gay and bisexual men.d
- Most of the 55 HIV diagnoses among AI/AN women in 2015 were attributed to heterosexual contact (73%; 40).
- From 2005 to 2014, the annual number of HIV diagnoses increased 19% (from 172 to 205) among AIs/ANs overall and 63% among AI/AN gay and bisexual men (from 81 to 132).
- In 2015, 96 AIs/ANs were diagnosed with AIDS. Of them, 59% (57) were men and 41% (39) were women.
HIV Diagnoses Among American Indians/Alaska Natives
in the US by Transmission Category and Sex, 2015
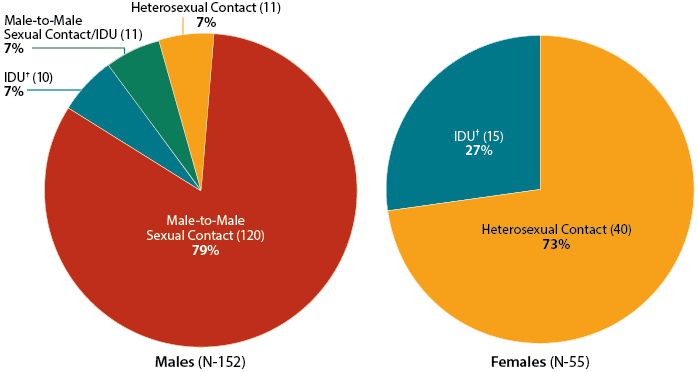
† Injection drug use
The terms male-to-male sexual contact and male-to-male sexual contact and injection drug use are used in CDC surveillance systems. They indicate the behaviors that transmit HIV infection, not how individuals self-identify in terms of their sexuality.
Source: CDC. Diagnoses of HIV infection in the United States and dependent areas, 2015. HIV Surveillance Report 2016;27.
Living With HIV and Deaths
- Of the 3,600 AIs/ANs estimated to be living with HIV in 2013, 18% (630) were undiagnosed. By comparison, 13% of everyone living with HIV were undiagnosed.
- Of AIs/ANs diagnosed with HIV in 2014, 78% were linked to medical care within 1 month.e
- At the end of 2013, 53% of AIs/ANs who had been living with diagnosed HIV for at least a year were retained in care (receiving continuous HIV medical care), and 52% had achieved viral suppression.
- During 2014, 51 AIs/ANs died from HIV or AIDS.
Prevention Challenges
- Sexually transmitted diseases (STDs). From 2011 to 2015, AIs/ANs had the second highest rates of chlamydia and gonorrhea among all racial/ethnic groups. Having another STD increases a person’s risk for getting or transmitting HIV.
- Lack of awareness of HIV status. Almost 1 in 5 AIs/ANs who were living with HIV at the end of 2013 were unaware of their status. People who do not know they have HIV cannot take advantage of HIV care and treatment and may unknowingly pass HIV to others.
- Stigma. AI/AN gay and bisexual men may face culturally based stigma and confidentiality concerns that could limit opportunities for education and HIV testing, especially among those who live in rural communities or on reservations.
- Cultural diversity. There are over 560 federally recognized AI/AN tribes, whose members speak over 170 languages. Because each tribe has its own culture, beliefs, and practices, creating culturally appropriate prevention programs for each group can be challenging.
- Socioeconomic issues. Poverty, including limited access to high-quality housing, directly and indirectly increases the risk for HIV infection and affects the health of people living with and at risk for HIV infection. Compared with other racial/ethnic groups, AIs/ANs have higher poverty rates, have completed fewer years of education, are younger, are less likely to be employed, and have lower rates of health insurance coverage.
- Alcohol and illicit drug use. Alcohol and substance use can impair judgment and lead to behaviors that increase the risk of HIV. Injection drug use can directly increase the risk of HIV through sharing contaminated needles, syringes, and other equipment. Compared with other racial/ethnic groups, AIs/ANs tend to use alcohol and drugs at a younger age and use them more often and in higher quantities.
- Data limitations. Racial misidentification of AIs/ANs may lead to the undercounting of this population in HIV surveillance systems and may contribute to the underfunding of targeted services for AI/AN.
What CDC Is Doing
CDC and its partners are pursuing a high-impact prevention approach to advance the goals of the National HIV/AIDS Strategy, maximize the effectiveness of current HIV prevention methods, and improve HIV data collection among AI/AN. Activities include:
- Working with the Indian Health Service (IHS) and tribal leaders of the CDC Tribal Consultation Advisory Committee to discuss methods for developing and implementing scalable, effective prevention approaches that reach those at greatest risk for HIV, including young gay and bisexual AI/AN men.
- Providing support and technical assistance to health departments and community-based organizations to deliver effective prevention interventions.
- Ensuring that capacity-building assistance providers incorporate cultural competency, linguistics, and educational appropriateness into all services delivered.
- Providing capacity building assistance directly to the IHS so it can strengthen its support for HIV activities, including HIV testing capacity; We R Native, a comprehensive health resource for Native youth; and the Red Talon Project, which works to achieve a more coordinated national and Northwest tribal response to STDs/HIV.
- Collaborating with National Association of State and Territorial AIDS Directors to release an issue brief, Native Gay Men and Two Spirit People: HIV/AIDS and Viral Hepatitis Programs and Services.
- Raising awareness through the Act Against AIDS campaigns, including
- Doing It, a national HIV testing and prevention campaign that encourages all adults to get tested for HIV and know their status;
- Let’s Stop HIV Together, which raises HIV awareness and fights stigma among all Americans and provides many stories about people living with HIV; and
- HIV Treatment Works, which highlights how men and women who are living with HIV have overcome barriers. The campaign provides resources and encourages people living with HIV to Get In Care, Stay In Care, and Live Well.
In addition, the Office for State, Tribal, Local, and Territorial Support (OSTLTS) serves as the primary link between CDC, the Agency for Toxic Substance and Disease Registry, and tribal governments. OSTLTS’s tribal support activities are focused on fulfilling CDC’s supportive role in ensuring that AI/AN communities receive public health services that keep them safe and healthy.
a Percentage of AI/AN reporting only one race.
b Hispanics/Latinos can be of any race.
c HIV and AIDS diagnoses indicate when a person is diagnosed with HIV infection or AIDS, but do not indicate when the person was infected.
d The term gay and bisexual men, referred to as men who have sex with men in CDC surveillance systems, indicates how individuals self-identify in terms of their sexuality, not a behavior that transmits HIV infection.
eIn 32 states and the District of Columbia (the areas with complete lab reporting by December 2015).
Bibliography
- US Census Bureau. Facts for features, American Indian and Alaska Native heritage month, November 2016. Accessed January 17, 2017.
- CDC. Diagnoses of HIV infection in the United States and dependent areas, 2015. HIV Surveillance Report 2016;27. Accessed January 17, 2017.
- CDC. High-Impact HIV Prevention: CDC’s approach to reducing HIV infections in the United States. Accessed January 17, 2017.
- CDC. Improving HIV Surveillance among American Indians and Alaska Natives in the United States. Accessed January 17, 2017.
- CDC. Monitoring selected national HIV prevention and care objectives by using HIV surveillance data—United States and 6 dependent areas—2014. HIV Surveillance Supplemental Report 2015;21(4). Accessed January 17, 2017.
- CDC. Sexually transmitted disease surveillance 2015. Accessed January 17, 2017.
- Burks DJ, Robbins R, Durtschi JP. American Indian gay, bisexual and two-spirit men: a rapid assessment of HIV/AIDS risk factors, barriers to prevention and culturally-sensitive intervention. Cult Health Sex 2011;13(3):283-98. PubMed Abstract.
- Bureau of Indian Affairs. Indian entities recognized and eligible to receive services from the United States Bureau of Indian Affairs.. Fed Regist 2012;77(155):47868. Accessed January 17, 2017.
- James C, Schwartz K, Berndt J. A profile of American Indians and Alaska Natives and their health coverage. Menlo Park, CA: Henry J. Kaiser Family Foundation; 2009. Accessed January 17, 2017.
- Walters KL, Simoni JM, Evans-Campbell T. Substance use among American Indians and Alaska Natives: incorporating culture in an ‘Indigenist’ stress-coping paradigm Public Health Rep 2002;117(1):s104-17. PubMed Abstract.
- Bertolli J, Lee LM, Sullivan PS, American Indian/Alaska Native Race/Ethnicity Data Validation Workgroup. Racial misidentification of American Indians/Alaska Natives in the HIV/AIDS reporting systems of five states and one urban health jurisdiction, US, 1984–2000. Public Health Rep 2007;122(3):382-94. PubMed Abstract.
- CDC. Deaths: final data for 2014. National Vital Statistics Reports 2016; 65(4). Accessed January 17, 2017.
- CDC. Trends in U.S. HIV diagnoses, 2005-2014. Accessed January 17, 2017.
Additional Resources
- CDC-INFO 1-800-CDC-INFO (232-4636)
- CDC HIV Website
- CDC Act Against AIDS Campaign
- CDC HIV Risk Reduction Tool (BETA)
- Page last reviewed: March 16, 2017
- Page last updated: March 16, 2017
- Content source: Division of HIV/AIDS Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, Centers for Disease Control and Prevention


 ShareCompartir
ShareCompartir