HIV Among Native Hawaiians and Other Pacific Islanders in the United States
Fast Facts
- NHOPI represented less than 1% of new HIV diagnoses in the United States in 2015.
- From 2010 to 2014, the annual number of HIV diagnoses declined 22% among NHOPI.
- Nearly 20% of adult and adolescent NHOPI living with HIV do not know it.
Although Native Hawaiians and Other Pacific Islanders (NHOPI) account for a very small percentage of new HIV diagnoses, HIV affects NHOPI in ways that are not always apparent because of their small population sizes.
The Numbers
HIV and AIDS Diagnosesa
- In 2015, 79 NHOPI were diagnosed with HIV, representing less than 1% of new HIV diagnoses in the United States. NHOPI make up 0.2% of the population.
- NHOPI had the third-highest rate of HIV diagnoses (14.1 per 100,000 people) by race/ethnicity in 2015, behind blacks/African Americans and Hispanics/Latinos.b
- Gay and bisexual menc accounted for 78% (62) of HIV diagnoses among NHOPI in 2015.
- The annual number of HIV diagnoses among NHOPI declined 22% from 2010 to 2014.
- In 2015, 22 NHOPI were diagnosed with AIDS in the United States.
Diagnoses of HIV Infection among Adult and Adolescent Native Hawaiians and Other Pacific Islanders, by Transmission Category, 2015 – United States
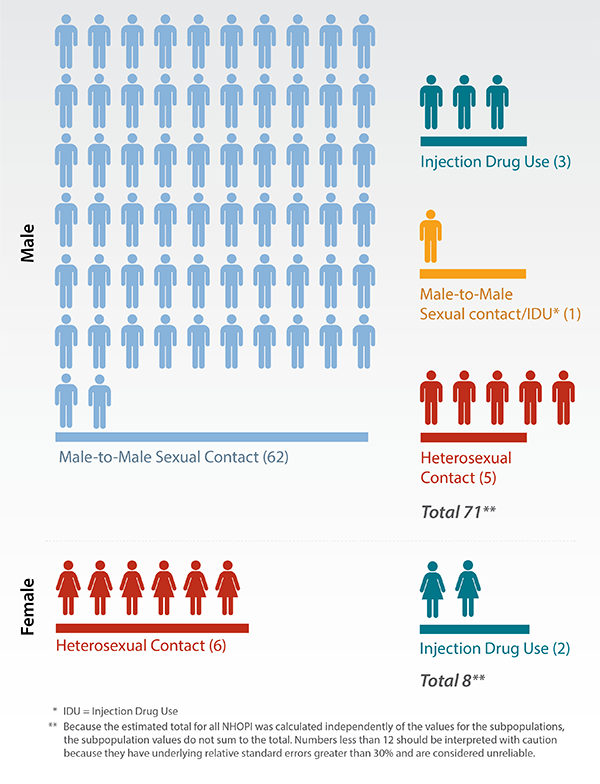
Source: CDC. Diagnoses of HIV infection in the United States and dependent areas, 2015. HIV Surveillance Report 2016;27
Living With HIV
- In 2013, an estimated 1,200 NHOPI were living with HIV in the United States. Of those, nearly 20% had not been diagnosed. By comparison, 13% of all Americans living with HIV are undiagnosed.
- Among NHOPI who were diagnosed with HIV in 2014, 84% were linked to care within 1 month.d
- Among NHOPI diagnosed with HIV in 2012 or earlier and alive at the end of 2013, 47% were retained in HIV care, and 55% had a suppressed viral load.e
Prevention Challenges
Some behaviors put everyone at risk for HIV, including NHOPI. These behaviors include having vaginal or anal sex without a condom or without medicines to prevent or treat HIV, or sharing injection drug equipment with someone who has HIV. Other factors particularly affect NHOPI:
- Lack of awareness of HIV status can affect HIV rates in communities. People who do not know they have HIV cannot take advantage of HIV care and treatment and may unknowingly pass HIV to others.
- Socioeconomic factors such as poverty, inadequate or no health care coverage, language barriers, and lower educational attainment among NHOPI may contribute to lack of awareness about HIV risk and higher-risk behaviors.
- Cultural factors may affect the risk of HIV infection. NHOPI cultural customs, such as not talking about sex across generations, may stigmatize sexuality in general, and homosexuality specifically, as well as interfere with HIV risk-reduction strategies, such as condom use.
- Limited research about NHOPI health and HIV infection and small population numbers have resulted in a lack of targeted prevention programs and behavioral interventions for this population.
- The low reported number of HIV cases among NHOPI may not reflect the true burden of HIV in this population because of race/ethnicity misidentification that could lead to an underestimation of HIV infection.
What CDC Is Doing
CDC and its partners are pursuing a high-impact prevention approach to maximize the effectiveness of current HIV prevention methods.
- CDC provides support and technical assistance to health departments and community-based organizations to deliver prevention programs for NHOPI, such as The Banyan Tree Project.
- HIV Prevention Projects for Community-Based Organizations funds the Asian Pacific AIDS Intervention Team and the Asian and Pacific Islander Wellness Center, which provide an array of culturally sensitive services, including HIV care and testing, HIV education, counseling, behavioral health, substance abuse, and social support services.
- Capacity Building Assistance for High-Impact HIV Prevention provides technical assistance in capacity building to the Asian and Pacific Islander American Health Forum and the Asian and Pacific Islander Wellness Center.
- The CDC publication Effective HIV Surveillance Among Asian Americans and Native Hawaiians and Other Pacific Islanders outlines successful HIV data collection activities for health departments in states with high concentrations of NHOPI.
- Through its Act Against AIDS campaigns, CDC provides messages about HIV treatment and prevention. For example,
- Doing It encourages all adults to get tested for HIV and know their status.
- Let’s Stop HIV Together raises awareness about HIV and fights stigma.
- HIV Treatment Works encourages people living with HIV to stay in care.
a HIV and AIDS diagnoses indicate when a person received an HIV or AIDS diagnosis, not when the person was infected.
b Hispanics/Latinos can be of any race.
c The term male-to-male sexual contact is used in CDC surveillance systems. It indicates a behavior that transmits HIV infection, not how individuals self-identify in terms of their sexuality. This fact sheet uses the term gay and bisexual men.
d In 32 states and the District of Columbia (the areas with complete lab reporting by December 2015).
e A person with a suppressed viral load has a very low level of the virus. That person can stay healthy and has a dramatically reduced risk of transmitting the virus to others.
Bibliography
- CDC. Diagnoses of HIV infection and AIDS in the United States and dependent areas, 2015. HIV Surveillance Report 2016;27. Accessed February 14, 2017.
- CDC. Monitoring selected national HIV prevention and care objectives by using HIV surveillance data—United States and 6 dependent areas—2014. HIV Surveillance Supplemental Report 2015;21(4). Accessed February 14, 2017.
- Adih WK, Campsmith M, Williams CL, Hardnett FP, Hughes D. Epidemiology of HIV among Asians and Pacific Islanders in the United States, 2001-2008. J Int Assoc Physicians AIDS Care (Chic) 2011;10(3):150-9. PubMed abstract.
- Cook WK, Chung C, Ve’e T. Native Hawaiian and Pacific Islander Health Disparities. San Francisco, CA: Asian & Pacific Islander American Health Forum; August 2010.
- DiStefano AS, Hui B, Barrera-Ng A, et al. Contextualization of HIV and HPV risk and prevention among Pacific Islander young adults in Southern California. Soc Sci Med 2012;75(4):699-708.
- Takahashi LM, Kim AJ, Sablan-Santos L, et al. HIV testing behavior among Pacific Islanders in Southern California: exploring the importance of race/ethnicity, knowledge, and domestic violence. AIDS Educ Prev 2011;23(1):54-64. PubMed abstract.
Additional Resources
- CDC-INFO 1-800-CDC-INFO (232-4636)
- CDC HIV Website
- CDC Act Against AIDS Campaign
- CDC HIV Risk Reduction Tool (BETA)
- Page last reviewed: May 8, 2017
- Page last updated: May 8, 2017
- Content source: Division of HIV/AIDS Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, Centers for Disease Control and Prevention


 ShareCompartir
ShareCompartir