HIV Among Transgender People
Fast Facts
- Transgender women in the United States are at high risk for HIV.
- Half of transgender people diagnosed with HIV are black/African American.
- Many factors make HIV prevention among transgender people a challenge.

Terminology
Transgender is a term for people whose gender identity or expression is different from their sex assigned at birth. Gender identity refers to a person’s internal understanding of their own gender. Gender expression describes a person’s outward presentation of their gender (for example, how they dress). Transgender women describes people who were assigned the male sex at birth but identify as women. Transgender men describes people who were assigned the female sex at birth but identify as men.
The Numbers
• In the United States, it is estimated that almost 1 million adults identify as transgender.a
• From 2009 to 2014, 2,351 transgender people were diagnosed with HIV in the United States.b Eighty-four percent (1,974) were transgender women, 15% (361) were transgender men, and less than 1% (16) had another gender identity.
• Around half of transgender people (43% [844] of transgender women; 54% [193] of transgender men) who received an HIV diagnosis from 2009 to 2014 lived in the South.c
• A 2013 report found that the estimated percentage of transgender women living with HIV in the United States was 22% among 2,705 transgender women sampled.
• Among the 3.3 million HIV testing eventsd reported to CDC in 2013, the percentage of transgender people who received a new HIV diagnosis was more than 3 times the national average.
HIV Diagnoses Among Transgender People in the United States
by Race/Ethnicity, 2009-2014
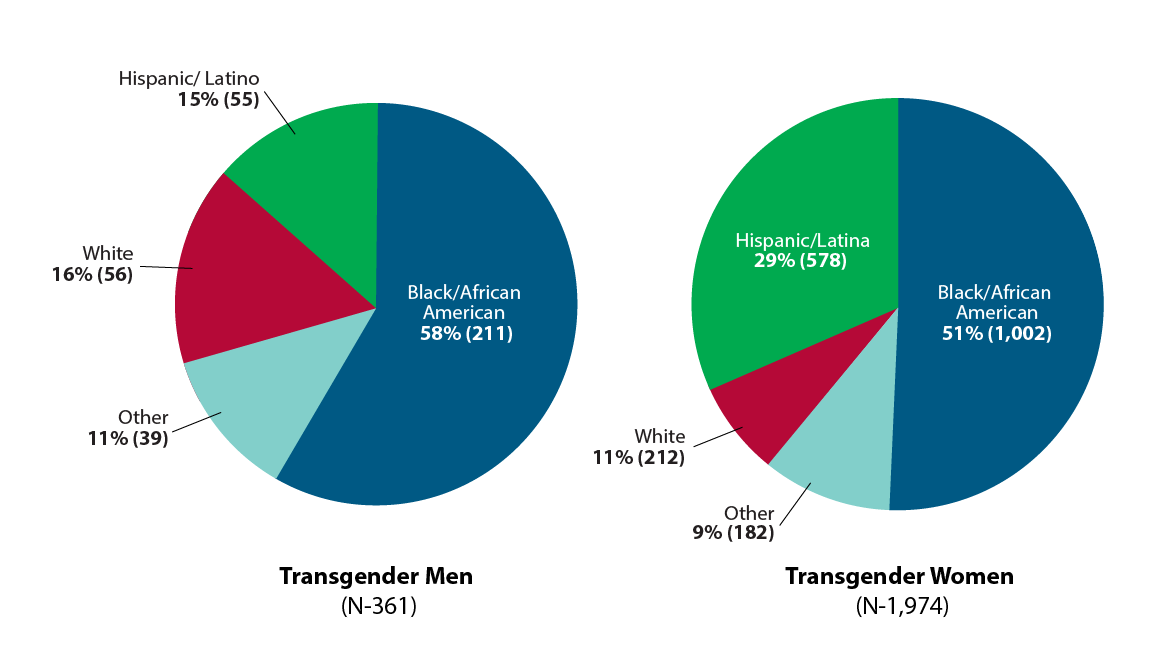
Source: Clark H, Babu AS, Wiewel EW, Opoku J, Crepaz N. Diagnosed HIV Infection in Transgender Adults and Adolescents: Results from the National HIV Surveillance System, 2009-2014. December 2016.
Prevention Challenges
- Multiple factors have put transgender people at risk for HIV infection and transmission, including multiple sexual partners, anal or vaginal sex without condoms or medicines to prevent HIV, injecting hormones or drugs with shared syringes and other drug paraphernalia, commercial sex work, mental health issues, incarceration, homelessness, unemployment, and high levels of substance misuse compared to the general population, as well as violence and lack of family support.
- HIV behavioral interventions developed for other at-risk groups have been adapted for use with transgender people. However, the effectiveness of these interventions is understudied. Effective behavioral interventions that address the full range of risk factors and health concerns are needed to improve the health of transgender people.
- Many transgender people face stigma, discrimination, social rejection, and exclusion that prevent them from fully participating in society, including accessing health care, education, employment, and housing. These factors affect the health and well-being of transgender people, placing them at increased risk for HIV.
- Insensitivity to transgender issues by health care providers can be a barrier for transgender people diagnosed with HIV and seeking quality treatment and care services. Few health care providers receive proper training or are knowledgeable about transgender health issues and their unique needs. This can lead to limited health care access and negative health care encounters.
- Transgender-specific data are limited. Some federal, state, and local agencies do not collect or have complete data on transgender individuals. Using the two-step data collection method of asking for sex assigned at birth and current gender identity can help increase the likelihood that transgender people are correctly identified in HIV surveillance programs. Accurate data on transgender status can lead to more effective public health actions.
- Transgender men’s sexual health has not been well studied. Over half of transgender men with diagnosed HIV infection had no identified or reported risk. Additional research is needed to understand HIV risk behavior among transgender men, especially those who have sex with other men.
What CDC Is Doing
CDC and its partners are pursuing a high-impact prevention approach to maximize the effectiveness of current HIV prevention methods among transgender people. Activities include:
- Awarded $11 million per year for 5 years, beginning in 2011, to community-based organizations (CBOs) to provide HIV testing to young gay and bisexual men and young transgender people of color. A new funding opportunity focusing on this population will begin in 2017 and continue for 5 years, depending on the availability of funds.
- Supporting health department demonstration projects that provide pre-exposure prophylaxis (PrEP) support services and data-to-care activities prioritizing gay and bisexual men and transgender people at substantial risk for acquiring HIV, particularly people of color.
- Providing support and technical assistance to health departments, CBOs, and providers to support interventions for transgender people (e.g., condom distribution, community mobilization, HIV testing, and coordinated referral networks and service integration).
- Through its Capacity Building Assistance initiative, CDC is working with the Center of Excellence for Transgender Health to support National Transgender HIV Testing Day. This day promotes HIV testing, prevention, and treatment efforts among transgender people.
- Developed Act Against AIDS communication materials to reach transgender people, including campaigns such as:
- Doing It, which encourages all adults to get tested for HIV and know their status, and includes images and testimonial videos featuring transgender leaders.
- Let’s Stop HIV Together, which raises awareness about HIV and fights stigma, and includes the stories of transgender women.
- HIV Treatment Works, which encourages people living with HIV to stay in care, and features transgender women’s stories of staying healthy while living with HIV.
- Start Talking. Stop HIV., which helps gay and bisexual cisgender and transgender men communicate about safer sex, testing, and other HIV prevention issues.
a According to Williams Institute scholars, this estimate likely does not represent the entire transgender population. National surveys in the future may observe higher numbers of transgender people.
bThese data may underreport HIV diagnoses among transgender people because of challenges in accurately identifying and reporting gender identity in HIV surveillance.
c Includes Alabama, Arkansas, Delaware, District of Columbia, Florida, Georgia, Kentucky, Louisiana, Maryland, Mississippi, North Carolina, Oklahoma, South Carolina, Tennessee, Texas, Virginia, and West Virginia.
d An HIV testing event is one or more HIV tests performed with a person to determine that person’s HIV status. During one testing event, a person may be tested once or multiple times.
For more information, visit CDC’s Lesbian, Gay, Bisexual, and Transgender Health website.
Bibliography
- Baral SD, Poteat T, Strömdahl S, Wirtz AL, Guadamuz TE, Beyrer C. Worldwide burden of HIV in transgender women: a systematic review and meta-analysis. Lancet Infect Dis 2013;13(3):214-22.
- Brennan J, Kuhns LM, Johnson AK, Belzer M, Wilson EC, Garofalo R, and the Adolescent Medicine Trials Network for HIV/AIDS Interventions. Syndemic theory and HIV-related risk among young transgender women: the role of multiple, co-occurring health problems and social marginalization. Am J Public Health 2012;102(9):1751-7.
- CDC. CDC-funded HIV testing: United States, Puerto Rico, and U.S. Virgin Islands, 2013. June 2015. Accessed February 27, 2017.
- CDC. Funding opportunity announcement: PS11-1113: Human immunodeficiency virus (HIV) prevention projects for young men of color who have sex with men and young transgender persons of color. Accessed February 27, 2017.
- CDC. Funding opportunity announcement: PS15-1502: Comprehensive high-impact HIV prevention projects for community-based organizations. Accessed February 27, 2017.
- CDC. Funding opportunity announcement: PS15-1506: Health department demonstration projects to reduce HIV infections and improve engagement in HIV medical care among men who have sex with men (MSM) and transgender persons. Accessed February 27, 2017.
- Chen S, McFarland W, Thompson HM, Raymond HF. Transmen in San Francisco: what do we know from HIV test site data? AIDS Behav 2011;15:659-62.
- Clark H, Babu AS, Wiewel EW, Opoku J, Crepaz N. Diagnosed HIV Infection in Transgender Adults and Adolescents: Results from the National HIV Surveillance System, 2009-2014. December 2016. Accessed February 27, 2017.
- De Santis JP. HIV infection risk factors among male-to-female transgender persons: a review of the literature. J Assoc Nurses AIDS Care 2009;20(5):362-72.
- Flores AR, Herman JL, Gates GJ, Brown TNT. How many adults identify as transgender in the United States? Los Angeles, CA: The Williams Institute. June 2016. Accessed February 27, 2017.
- Garofalo R, Johnson AK, Kuhns LM, Cotton C, Joseph H, Margolis A. Life Skills: evaluation of a theory-driven behavioral HIV prevention intervention for young transgender women. J Urban Health 2012;89(3):419-31.
- Grant JM, Mottet LA, Tanis J, Harrison J, Herman JL, Keisling M. Injustice at every turn: a report of the National Transgender Discrimination Survey. Washington: National Center for Transgender Equality; 2011.
- Herbst JH, Jacobs ED, Finlayson TJ, McKleroy VS, Neumann MS, Crepaz N. Estimating HIV prevalence and risk behaviors of transgender persons in the United States: a systematic review. AIDS Behav 2008;12(1):1-17.
- Hotton AL, Garofalo R, Kuhns LM, and Johnson AK. Substance use as a mediator of the relationship between life stress and sexual risk among young transgender women. AIDS Educ Prev 2013;25(1):62-71.
- James SE, Herman JL, Rankin S, Keisling M, Mottet L, Anafi M. The Report of the 2015 U.S. Transgender Survey. Washington: National Center for Transgender Equality and National Gay 2016.
- Meerwijk EL, Sevelius JM. Transgender population size in the United States: a meta-regression of population-based probability samples. Am J Public Health 2017; 107(2):e1-e8.
- Mizuno Y, Frazier EL, Huang P, Skarbinski J. Characteristics of transgender women living with HIV receiving medical care in the United States. LGBT Health 2015;2(00):1-7.
- New York City Department of Health and Mental Hygiene. Surveillance slide sets: HIV among people identified as transgender in New York City, 2011-2015. December 2016. Accessed April 18, 2017.
- Nuttbrock L, Hwahng S, Bockting W, et al. Lifetime risk factors for HIV/sexually transmitted infections among male-to-female transgender persons. J Acquir Immun Def Syndr 2009;52(3):417–21.
- Reisner SL, Perkovich B, and Mimiaga MJ. A mixed methods study of the sexual health needs of New England transmen who have sex with nontransgender men. AIDS Patient Care STDS 2010;24(8):501-13.
- Rowniak S, Chesla C, Rose CD, Holzemer WL. Transmen: the HIV risk of gay identity. AIDS Educ Prev 2011;23(6):508-20.
- Sanchez T, Finlayson T, Murrill C, Guilin V, Dean L. Risk behaviors and psychosocial stressors in the New York City House Ball community: a comparison of men and transgender women who have sex with men. AIDS Behav 2010;14:351-8.
Additional Resources
- CDC-INFO 1-800-CDC-INFO (232-4636)
- CDC HIV Website
- CDC Act Against AIDS Campaign
- CDC HIV Risk Reduction Tool (BETA)
- Page last reviewed: July 26, 2017
- Page last updated: August 3, 2017
- Content source: Division of HIV/AIDS Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, Centers for Disease Control and Prevention


 ShareCompartir
ShareCompartir