Lesson 1: Introduction to Epidemiology
Section 9: Natural History and Spectrum of Disease
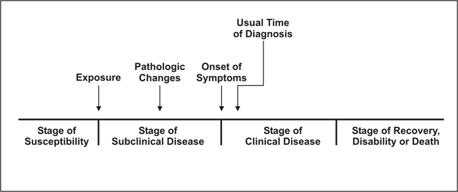
Natural history of disease refers to the progression of a disease process in an individual over time, in the absence of treatment. For example, untreated infection with HIV causes a spectrum of clinical problems beginning at the time of seroconversion (primary HIV) and terminating with AIDS and usually death. It is now recognized that it may take 10 years or more for AIDS to develop after seroconversion.(43) Many, if not most, diseases have a characteristic natural history, although the time frame and specific manifestations of disease may vary from individual to individual and are influenced by preventive and therapeutic measures.
Figure 1.18 Natural History of Disease Timeline
Source: Centers for Disease Control and Prevention. Principles of epidemiology, 2nd ed. Atlanta: U.S. Department of Health and Human Services;1992.
The process begins with the appropriate exposure to or accumulation of factors sufficient for the disease process to begin in a susceptible host. For an infectious disease, the exposure is a microorganism. For cancer, the exposure may be a factor that initiates the process, such as asbestos fibers or components in tobacco smoke (for lung cancer), or one that promotes the process, such as estrogen (for endometrial cancer).
After the disease process has been triggered, pathological changes then occur without the individual being aware of them. This stage of subclinical disease, extending from the time of exposure to onset of disease symptoms, is usually called the incubation period for infectious diseases, and the latency period for chronic diseases. During this stage, disease is said to be asymptomatic (no symptoms) or inapparent. This period may be as brief as seconds for hypersensitivity and toxic reactions to as long as decades for certain chronic diseases. Even for a single disease, the characteristic incubation period has a range. For example, the typical incubation period for hepatitis A is as long as 7 weeks. The latency period for leukemia to become evident among survivors of the atomic bomb blast in Hiroshima ranged from 2 to 12 years, peaking at 6–7 years.(44) Incubation periods of selected exposures and diseases varying from minutes to decades are displayed in Table 1.7.
Table 1.7 Incubation Periods of Selected Exposures and Diseases
| Exposure | Clinical Effect | Incubation/Latency Period |
|---|---|---|
Saxitoxin and similar toxins from shellfish | Paralytic shellfish poisoning (tingling, numbness around lips and fingertips, giddiness, incoherent speech, respiratory paralysis, sometimes death) | few minutes–30 minutes |
Organophosphorus ingestion | Nausea, vomiting, cramps, headache, nervousness, blurred vision, chest pain, confusion, twitching, convulsions | few minutes–few hours |
| Salmonella | Diarrhea, often with fever and cramps | usually 6–48 hours |
SARS-associated corona virus | Severe Acute Respiratory Syndrome (SARS) | 3–10 days, usually 4–6 days |
| Varicella-zoster virus | Chickenpox | 10–21 days, usually 14–16 days |
| Treponema pallidum | Syphilis | 10–90 days, usually 3 weeks |
| Hepatitis A virus | Hepatitis | 14–50 days, average 4 weeks |
| Hepatitis B virus | Hepatitis | 50–180 days, usually 2–3 months |
Human immunodeficiency virus | AIDS | <1 to 15+ years |
Atomic bomb radiation (Japan) | Leukemia | 2–12 years |
Radiation (Japan, Chernobyl) | Thyroid cancer | 3–20+ years |
Radium (watch dial painters) | Bone cancer | 8–40 years |
Although disease is not apparent during the incubation period, some pathologic changes may be detectable with laboratory, radiographic, or other screening methods. Most screening programs attempt to identify the disease process during this phase of its natural history, since intervention at this early stage is likely to be more effective than treatment given after the disease has progressed and become symptomatic.
The onset of symptoms marks the transition from subclinical to clinical disease. Most diagnoses are made during the stage of clinical disease. In some people, however, the disease process may never progress to clinically apparent illness. In others, the disease process may result in illness that ranges from mild to severe or fatal. This range is called the spectrum of disease. Ultimately, the disease process ends either in recovery, disability or death.
For an infectious agent, infectivity refers to the proportion of exposed persons who become infected. Pathogenicity refers to the proportion of infected individuals who develop clinically apparent disease. Virulence refers to the proportion of clinically apparent cases that are severe or fatal.
Because the spectrum of disease can include asymptomatic and mild cases, the cases of illness diagnosed by clinicians in the community often represent only the tip of the iceberg. Many additional cases may be too early to diagnose or may never progress to the clinical stage. Unfortunately, persons with inapparent or undiagnosed infections may nonetheless be able to transmit infection to others. Such persons who are infectious but have subclinical disease are called carriers. Frequently, carriers are persons with incubating disease or inapparent infection. Persons with measles, hepatitis A, and several other diseases become infectious a few days before the onset of symptoms. However carriers may also be persons who appear to have recovered from their clinical illness but remain infectious, such as chronic carriers of hepatitis B virus, or persons who never exhibited symptoms. The challenge to public health workers is that these carriers, unaware that they are infected and infectious to others, are sometimes more likely to unwittingly spread infection than are people with obvious illness.
References (This Section)
- Mindel A, Tenant-Flowers M. Natural history and management of early HIV infection. BMJ 2001;332:1290–93.
- Cobb S, Miller M, Wald N. On the estimation of the incubation period in malignant disease. J Chron Dis 1959;9:385–93.
Previous Page Next Page: Section 10
Image Description
Figure 1.18
Description: Timeline shows state of susceptibility, exposure, subclinical disease in which pathologic changes takes place, onset of symptoms, followed by usual time of diagnosis, clinical disease, followed by recovery, disability, or death. Return to text.
- Page last reviewed: May 18, 2012
- Page last updated: May 18, 2012
- Content source:


 ShareCompartir
ShareCompartir