Lesson 1: Introduction to Epidemiology
Section 4: Core Epidemiologic Functions
In the mid-1980s, five major tasks of epidemiology in public health practice were identified: public health surveillance, field investigation, analytic studies, evaluation, and linkages. (17) A sixth task, policy development, was recently added. These tasks are described below.
Public health surveillance
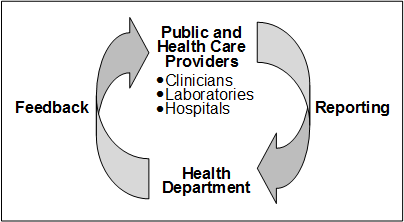
Public health surveillance is the ongoing, systematic collection, analysis, interpretation, and dissemination of health data to help guide public health decision making and action. Surveillance is equivalent to monitoring the pulse of the community. The purpose of public health surveillance, which is sometimes called “information for action,” (18) is to portray the ongoing patterns of disease occurrence and disease potential so that investigation, control, and prevention measures can be applied efficiently and effectively. This is accomplished through the systematic collection and evaluation of morbidity and mortality reports and other relevant health information, and the dissemination of these data and their interpretation to those involved in disease control and public health decision making.
Morbidity and mortality reports are common sources of surveillance data for local and state health departments. These reports generally are submitted by health-care providers, infection control practitioners, or laboratories that are required to notify the health department of any patient with a reportable disease such as pertussis, meningococcal meningitis, or AIDS. Other sources of health-related data that are used for surveillance include reports from investigations of individual cases and disease clusters, public health program data such as immunization coverage in a community, disease registries, and health surveys.
Most often, surveillance relies on simple systems to collect a limited amount of information about each case. Although not every case of disease is reported, health officials regularly review the case reports they do receive and look for patterns among them. These practices have proven invaluable in detecting problems, evaluating programs, and guiding public health action.
While public health surveillance traditionally has focused on communicable diseases, surveillance systems now exist that target injuries, chronic diseases, genetic and birth defects, occupational and potentially environmentally-related diseases, and health behaviors. Since September 11, 2001, a variety of systems that rely on electronic reporting have been developed, including those that report daily emergency department visits, sales of over-the-counter medicines, and worker absenteeism.(19, 20) Because epidemiologists are likely to be called upon to design and use these and other new surveillance systems, an epidemiologist's core competencies must include design of data collection instruments, data management, descriptive methods and graphing, interpretation of data, and scientific writing and presentation.
Field investigation
As noted above, surveillance provides information for action. One of the first actions that results from a surveillance case report or report of a cluster is investigation by the public health department. The investigation may be as limited as a phone call to the health-care provider to confirm or clarify the circumstances of the reported case, or it may involve a field investigation requiring the coordinated efforts of dozens of people to characterize the extent of an epidemic and to identify its cause.
The objectives of such investigations also vary. Investigations often lead to the identification of additional unreported or unrecognized ill persons who might otherwise continue to spread infection to others. For example, one of the hallmarks of investigations of persons with sexually transmitted disease is the identification of sexual partners or contacts of patients. When interviewed, many of these contacts are found to be infected without knowing it, and are given treatment they did not realize they needed. Identification and treatment of these contacts prevents further spread.
For some diseases, investigations may identify a source or vehicle of infection that can be controlled or eliminated. For example, the investigation of a case of Escherichia coli O157:H7 infection usually focuses on trying to identify the vehicle, often ground beef but sometimes something more unusual such as fruit juice. By identifying the vehicle, investigators may be able to determine how many other persons might have already been exposed and how many continue to be at risk. When a commercial product turns out to be the culprit, public announcements and recalling the product may prevent many additional cases.
Symbol of EIS
Occasionally, the objective of an investigation may simply be to learn more about the natural history, clinical spectrum, descriptive epidemiology, and risk factors of the disease before determining what disease intervention methods might be appropriate. Early investigations of the epidemic of SARS in 2003 were needed to establish a case definition based on the clinical presentation, and to characterize the populations at risk by time, place, and person. As more was learned about the epidemiology of the disease and communicability of the virus, appropriate recommendations regarding isolation and quarantine were issued.(21)
Field investigations of the type described above are sometimes referred to as “shoe leather epidemiology,” conjuring up images of dedicated, if haggard, epidemiologists beating the pavement in search of additional cases and clues regarding source and mode of transmission. This approach is commemorated in the symbol of the Epidemic Intelligence Service (EIS), CDC's training program for disease detectives — a shoe with a hole in the sole.
Analytic studies
Surveillance and field investigations are usually sufficient to identify causes, modes of transmission, and appropriate control and prevention measures. But sometimes analytic studies employing more rigorous methods are needed. Often the methods are used in combination — with surveillance and field investigations providing clues or hypotheses about causes and modes of transmission, and analytic studies evaluating the credibility of those hypotheses.
Clusters or outbreaks of disease frequently are investigated initially with descriptive epidemiology. The descriptive approach involves the study of disease incidence and distribution by time, place, and person. It includes the calculation of rates and identification of parts of the population at higher risk than others. Occasionally, when the association between exposure and disease is quite strong, the investigation may stop when descriptive epidemiology is complete and control measures may be implemented immediately. John Snow's 1854 investigation of cholera is an example. More frequently, descriptive studies, like case investigations, generate hypotheses that can be tested with analytic studies. While some field investigations are conducted in response to acute health problems such as outbreaks, many others are planned studies.
The hallmark of an analytic epidemiologic study is the use of a valid comparison group. Epidemiologists must be skilled in all aspects of such studies, including design, conduct, analysis, interpretation, and communication of findings.
- Design includes determining the appropriate research strategy and study design, writing justifications and protocols, calculating sample sizes, deciding on criteria for subject selection (e.g., developing case definitions), choosing an appropriate comparison group, and designing questionnaires.
- Conduct involves securing appropriate clearances and approvals, adhering to appropriate ethical principles, abstracting records, tracking down and interviewing subjects, collecting and handling specimens, and managing the data.
- Analysis begins with describing the characteristics of the subjects. It progresses to calculation of rates, creation of comparative tables (e.g., two-by-two tables), and computation of measures of association (e.g., risk ratios or odds ratios), tests of significance (e.g., chi-square test), confidence intervals, and the like. Many epidemiologic studies require more advanced analytic techniques such as stratified analysis, regression, and modeling.
- Finally, interpretation involves putting the study findings into perspective, identifying the key take-home messages, and making sound recommendations. Doing so requires that the epidemiologist be knowledgeable about the subject matter and the strengths and weaknesses of the study.
Evaluation
Epidemiologists, who are accustomed to using systematic and quantitative approaches, have come to play an important role in evaluation of public health services and other activities. Evaluation is the process of determining, as systematically and objectively as possible, the relevance, effectiveness, efficiency, and impact of activities with respect to established goals.(22)
- Effectiveness refers to the ability of a program to produce the intended or expected results in the field; effectiveness differs from efficacy, which is the ability to produce results under ideal conditions.
- Efficiency refers to the ability of the program to produce the intended results with a minimum expenditure of time and resources.
The evaluation itself may focus on plans (formative evaluation), operations (process evaluation), impact (summative evaluation), or outcomes — or any combination of these. Evaluation of an immunization program, for example, might assess the efficiency of the operations, the proportion of the target population immunized, and the apparent impact of the program on the incidence of vaccine-preventable diseases. Similarly, evaluation of a surveillance system might address operations and attributes of the system, its ability to detect cases or outbreaks, and its usefulness.(23)
Linkages
Epidemiologists working in public health settings rarely act in isolation. In fact, field epidemiology is often said to be a “team sport.” During an investigation an epidemiologist usually participates as either a member or the leader of a multidisciplinary team. Other team members may be laboratorians, sanitarians, infection control personnel, nurses or other clinical staff, and, increasingly, computer information specialists. Many outbreaks cross geographical and jurisdictional lines, so co-investigators may be from local, state, or federal levels of government, academic institutions, clinical facilities, or the private sector. To promote current and future collaboration, the epidemiologists need to maintain relationships with staff of other agencies and institutions. Mechanisms for sustaining such linkages include official memoranda of understanding, sharing of published or on-line information for public health audiences and outside partners, and informal networking that takes place at professional meetings.
Policy development
The definition of epidemiology ends with the following phrase: “…and the application of this study to the control of health problems.” While some academically minded epidemiologists have stated that epidemiologists should stick to research and not get involved in policy development or even make recommendations, (24) public health epidemiologists do not have this luxury. Indeed, epidemiologists who understand a problem and the population in which it occurs are often in a uniquely qualified position to recommend appropriate interventions. As a result, epidemiologists working in public health regularly provide input, testimony, and recommendations regarding disease control strategies, reportable disease regulations, and health-care policy.
 Exercise 1.3
Exercise 1.3
Match the appropriate core function to each of the statements below.
- Public health surveillance
- Field investigation
- Analytic studies
- Evaluation
- Linkages
- Policy development
- ____ Reviewing reports of test results for Chlamydia trachomatis from public health clinics
- ____ Meeting with directors of family planning clinics and college health clinics to discuss Chlamydia testing and reporting
- ____ Developing guidelines/criteria about which patients coming to the clinic should be screened (tested) for Chlamydia infection
- ____ Interviewing persons infected with Chlamydia to identify their sex partners
- ____ Conducting an analysis of patient flow at the public health clinic to determine waiting times for clinic patients
- ____ Comparing persons with symptomatic versus asymptomatic Chlamydia infection to identify predictors
References (This Section)
- Tyler CW, Last JM. Epidemiology. In: Last JM, Wallace RB, editors. Maxcy-Rosenau-Last public health and preventive medicine, 14th ed. Norwalk (Connecticut): Appleton & Lange; 1992. p. 11.
- Orenstein WA, Bernier RH. Surveillance: information for action. Pediatr Clin North Am 1990; 37:709–34.
- Wagner MM, Tsui FC, Espino JU, Dato VM, Sittig DF, Caruana FA, et al. The emerging science of very early detection of disease outbreaks. J Pub Health Mgmt Pract 2001;6:51–9.
- Centers for Disease Control and Prevention. Framework for evaluating public health surveillance systems for early detection of outbreaks: recommendations from the CDC Working Group. MMWR May 7, 2004; 53(RR05);1–11.
- Centers for Disease Control and Prevention. Interim guidance on infection control precautions for patients with suspected severe acute respiratory syndrome (SARS) and close contacts in households. Available from: http://www.cdc.gov/ncidod/sars/ic-closecontacts.htm.
- Beaglehole R, Bonita R, Kjellstrom T. Basic epidemiology. Geneva: World Health Organization; 1993. p. 133.
- Centers for Disease Control and Prevention. Updated guidelines for evaluating public health surveillance systems: recommendations from the Guidelines Working Group. MMWR Recommendations and Reports 2001:50(RR13).
- Rothman KJ. Policy recommendations in epidemiology research papers. Epidemiol 1993; 4: 94–9.
Previous Page Next Page: Section 5
Image Description
Figure 1.3
Description: Surveillance information flows from public and health care providers such as clinicians, laboratories, and hospitals and health departments. Feedback flows from health departments back to public and health care providers. Return to text.
- Page last reviewed: May 18, 2012
- Page last updated: May 18, 2012
- Content source:


 ShareCompartir
ShareCompartir