Nilotinib
Nilotinib, sold under the brand name Tasigna, is a medication used to treat chronic myelogenous leukemia (CML) which has the Philadelphia chromosome.[2] It may be used both in initial cases of chronic phase CML as well as in accelerated and chronic phase CML that has not responded to imatinib.[2][3] It is taken by mouth.[3]
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Tasigna |
| Other names | AMN107 |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a608002 |
| License data | |
| Pregnancy category | |
| Routes of administration | By mouth |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 30%[1] |
| Protein binding | 98%[1] |
| Metabolism | Liver (mostly CYP3A4-mediated)[1] |
| Elimination half-life | 15-17 hours[1] |
| Excretion | Faeces (93%)[1] |
| Identifiers | |
IUPAC name
| |
| CAS Number |
|
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| PDB ligand | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.166.395 |
| Chemical and physical data | |
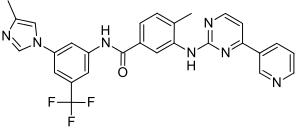
| Formula | C28H22F3N7O |
| Molar mass | 529.5245 g/mol g·mol−1 |
| 3D model (JSmol) | |
SMILES
| |
InChI
| |
| | |
Common side effects may include low platelets, low white blood cells, anemia, rashes, vomiting, diarrhea, and joint pains.[3] Other serious side effects may include QT prolongation, sudden death, pancreatitis, and liver problems.[3] It is not safe for use during pregnancy.[3] Nilotinib is a Bcr-Abl tyrosine kinase inhibitor and works by interfering with signalling within the cancer cell.[3]
Nilotinib was approved for medical use in the United States in 2007.[3] It is on the World Health Organization's List of Essential Medicines, the safest and most effective medicines needed in a health system.[4] In the United Kingdom it costs the NHS £2,432.85 per month as of 2018.[5] In the United States this amount costs US$14,367.94 as of 2019.[6]
Medical uses
It is used to treat Philadelphia chromosome (Ph+)-positive chronic myelogenous leukaemia.[1]
Adverse effects
Nilotinib has a number of adverse effects including headache, fatigue, gastrointestinal problems such as nausea, vomiting, diarrhea and constipation, muscle and joint pain, rash and other skin conditions, flu-like symptoms, and reduced blood cell count. Less typical side effects are those of the cardiovascular system, such as high blood pressure, various types of arrhythmia, and prolonged QT interval. Nilotinib can also affect the body's electrolyte and glucose balance.[7] Though lung-related adverse effects are rare when compared with imatinib and dasatinib, there is a case report of acute respiratory failure from diffuse alveolar hemorrhage in a people taking nilotinib.[8]
Nilotinib carries a black box warning in the United States for possible heart complications.[9][10] Contraindications include long QT syndrome, hypokalaemia, hypomagnesaemia, pregnancy, planned pregnancy, lactation and galactose/lactose intolerance.[1][11]
Cautions include:[1]
- Myelosuppression
- Tumour lysis syndrome
- Liver impairment
- History of pancreatitis
- Check serum lipase periodically in order to detect pancreatitis
- Total gastrectomy
- Avoid pregnancy or impregnating women
Dose reduction has been recommended in people with liver problems which involves recommendation of lower starting dose and monitoring of any hepatic function abnormalities.[12]
Hepatitis B virus reactivation may also occur.[5]
Interactions
Nilotinib has been reported as a substrate for OATP1B1 and OATP1B3. Interaction of nilotinib with OATP1B1 and OATP1B3 may alter its hepatic disposition and can lead to transporter mediated drug-drug interactions.[12] Nilotinib is an inhibitor of OATP-1B1 transporter but not for OATP-1B3.[13]
It is a substrate for CYP3A4 and hence grapefruit juice and other CYP3A4 inhibitors[14] will increase its action and inducers like St. John's wort[15] will decrease it. Patients report that pomegranates and starfruit may also interfere.
Food should not be eaten two hours before or one hour afterwards because it unpredictably increases its bioavailability, approximately doubling it.
Pharmacology
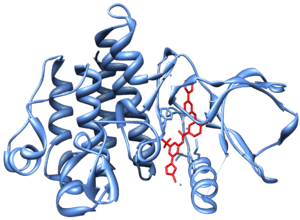
Nilotinib inhibits the kinases BCR-ABL,[16] KIT, LCK, EPHA3, EPHA8, DDR1, DDR2, PDGFRB, MAPK11 and ZAK.[17]
Structurally related to imatinib,[18] It is 10–30 fold more potent than imatinib in inhibiting Bcr-Abl tyrosine kinase activity and proliferation of Bcr-Abl expressing cells.[18][19][20][21]
History
Nilotinib was developed by Novartis.[3] It was developed based on the structure of the Abl-imatinib complex to address imatinib intolerance and resistance.[22][19][20]
It was approved for medical use by the FDA in October 2007,[7] EMA in September 2009,[23] MHRA in November 2007,[24] and TGA in January 2008.[11]
Society and culture
In the United Kingdom it costs the NHS £2,432.85 per month as of 2018.[5] In the United States this amount costs US$14,367.94 as of 2019.[6]
Research
Parkinson's disease
There is weak evidence that nilotinib may be beneficial with Parkinson's disease (PD), with a small clinical trial suggesting it might halt progression and improve symptoms.[25] However, there were significant side effects including infection, liver function tests abnormalities, hallucinations and heart attack, and the benefit in PD disappeared at follow up after drug discontinuation, raising question as to whether it was truly a disease modifying therapy. Nilotinib is currently undergoing phase II studies for treatment of Parkinson's.[26] Scientists and medical professionals have advised caution with over-optimistic interpretation of its effects in Parkinson's due to the significant media hype surrounding the small and early clinical trial.[27][28]
Other
Novartis announced on April 11, 2011 that it was discontinuing a phase III trial of nilotinib as the first-line treatment of gastrointestinal stromal tumor (GIST) based on the recommendation of an independent data monitoring committee. Interim results showed Tasigna is unlikely to demonstrate superiority compared to Novartis's Gleevec (imatinib)*, the current standard of care in this setting.[29]
Low dose nilotinib is also being investigated for use for and Alzheimer's disease, as well as for ALS, dementia and Huntington's disease.[30]
References
- "Tasigna (nilotinib) dosing, indications, interactions, adverse effects, and more". Medscape Reference. WebMD. Retrieved 25 January 2014.
- "Nilotinib". National Cancer Institute. 1 February 2008. Retrieved 14 November 2019.
- "Nilotinib Monograph for Professionals". Drugs.com. Retrieved 14 November 2019.
- "World Health Organization model list of essential medicines: 21st list 2019". 2019. hdl:10665/325771. Cite journal requires
|journal=(help) - British national formulary : BNF 76 (76 ed.). Pharmaceutical Press. 2018. p. 960. ISBN 9780857113382.
- "Tasigna Prices, Coupons & Patient Assistance Programs". Drugs.com. Retrieved 14 November 2019.
- "Complete Nilotinib information from Drugs.com". Drugs.com. Retrieved 25 January 2014.
- Donatelli, Christopher; Chongnarungsin, Daych; Ashton, Rendell (2014). "Acute respiratory failure from nilotinib-associated diffuse alveolar hemorrhage". Leukemia & Lymphoma. 55 (10): 1–6. doi:10.3109/10428194.2014.887714. PMID 24467220.
- "FDA Approves Tasigna for Treatment of Philadelphia Chromosome Positive Chronic Myeloid Leukemia". U.S. Food and Drug Administration. 2007-10-30. Retrieved 2009-08-04.
- "Prescribing information for Tasigna (nilotinib) Capsules" (PDF). NDA 022068. U.S. FDA. 2007-10-29. Retrieved 2009-08-04.
- "TASIGNA® nilotinib" (PDF). TGA eBusiness Services. 21 October 2013. Retrieved 25 January 2014.
- Khurana V, Minocha M, Pal D, Mitra AK (March 2014). "Role of OATP-1B1 and/or OATP-1B3 in hepatic disposition of tyrosine kinase inhibitors". Drug Metabol Drug Interact. 29 (3): 179–90. doi:10.1515/dmdi-2013-0062. PMC 4407685. PMID 24643910.
- Khurana V, Minocha M, Pal D, Mitra AK (May 2014). "Inhibition of OATP-1B1 and OATP-1B3 by tyrosine kinase inhibitors". Drug Metabol Drug Interact. 29 (4): 249–59. doi:10.1515/dmdi-2014-0014. PMC 4407688. PMID 24807167.
- Bailey, David G; Malcolm, J; Arnold, O; David Spence, J (1998-08-01). "Grapefruit juice–drug interactions". British Journal of Clinical Pharmacology. 46 (2): 101–110. doi:10.1046/j.1365-2125.1998.00764.x. ISSN 0306-5251. PMC 1873672. PMID 9723817.
- Komoroski, Bernard J.; Zhang, Shimin; Cai, Hongbo; Hutzler, J. Matthew; Frye, Reginald; Tracy, Timothy S.; Strom, Stephen C.; Lehmann, Thomas; Ang, Catharina Y. W. (2004-05-01). "Induction and inhibition of cytochromes P450 by the St. John's wort constituent hyperforin in human hepatocyte cultures". Drug Metabolism and Disposition. 32 (5): 512–518. doi:10.1124/dmd.32.5.512. ISSN 0090-9556. PMID 15100173.
- Weisberg E, Manley P, Mestan J, Cowan-Jacob S, Ray A, Griffin JD (June 2006). "AMN107 (nilotinib): a novel and selective inhibitor of BCR-ABL". Br. J. Cancer. 94 (12): 1765–9. doi:10.1038/sj.bjc.6603170. PMC 2361347. PMID 16721371.
- Manley, PW; Drueckes, P; Fendrich, G; Furet, P; Liebetanz, J; Martiny-Baron, G; Mestan, J; Trappe, J; et al. (2010). "Extended kinase profile and properties of the protein kinase inhibitor nilotinib". Biochimica et Biophysica Acta. 1804 (3): 445–53. doi:10.1016/j.bbapap.2009.11.008. PMID 19922818.
- Manley, P.; Cowan-Jacob, S.; Mestan, J. (2005). "Advances in the structural biology, design and clinical development of Bcr-Abl kinase inhibitors for the treatment of chronic myeloid leukaemia". Biochimica et Biophysica Acta. 1754 (1–2): 3–13. doi:10.1016/j.bbapap.2005.07.040. PMID 16172030.
- Jabbour, E.; Cortes, J.; Kantarjian, H. (2009). "Nilotinib for the treatment of chronic myeloid leukemia: An evidence-based review". Core Evidence. 4: 207–213. doi:10.2147/CE.S6003. PMC 2899790.
- Olivieri, A.; Manzione, L. (2007). "Dasatinib: a new step in molecular target therapy". Annals of Oncology. 18 Suppl 6: vi42–vi46. doi:10.1093/annonc/mdm223. PMID 17591830.
- Breccia, M.; Alimena, G. (2010). "Nilotinib: a second-generation tyrosine kinase inhibitor for chronic myeloid leukemia". Leukemia Research. 34 (2): 129–134. doi:10.1016/j.leukres.2009.08.031. PMID 19783301.
- Manley, P.; Stiefl, N.; Cowan-Jacob, S.; Kaufman, S.; Mestan, J.; Wartmann, M.; Wiesmann, M.; Woodman, R.; Gallagher, N. (2010). "Structural resemblances and comparisons of the relative pharmacological properties of imatinib and nilotinib". Bioorganic & Medicinal Chemistry. 18 (19): 6977–6986. doi:10.1016/j.bmc.2010.08.026. PMID 20817538.
- "Tasigna : EPAR - Product Information" (PDF). European Medicines Agency. Novartis Europharm Ltd. 18 October 2013. Retrieved 25 January 2014.
- "Tasigna 150mg Hard Capsules - Summary of Product Characteristics (SPC)". electronic Medicines Compendium. Novartis Pharmaceuticals UK Ltd. 9 September 2013. Retrieved 25 January 2014.
- Pagan, F.; Hebron, M.; Valadez, E. H.; Torres-Yaghi, Y.; Huang, X.; Mills, R. R.; Wilmarth, B. M.; Howard, H.; Dunn, C.; Carlson, A.; Lawler, A.; Rogers, S. L.; Falconer, R. A.; Ahn, J.; Li, Z.; Moussa, C. (2016). "Nilotinib Effects in Parkinson's disease and Dementia with Lewy bodies". Journal of Parkinson's Disease. 6 (3): 503–17. doi:10.3233/JPD-160867. PMC 5008228. PMID 27434297.
- Dash, Deepa (2019). "Anticancer Drugs for Parkinson's Disease: Is It a Ray of Hope or Only Hype?". Annals of Indian Academy of Neurology. 22 (1): 13–16. doi:10.4103/aian.AIAN_177_18. PMC 6327695. PMID 30692753.
- Robledo, I.; Jankovic, J. (2017). "Media hype: Patient and scientific perspectives on misleading medical news". Movement Disorders. 32 (9): 1319–1323. doi:10.1002/mds.26993. PMID 28370445.
- Wyse, R. K.; Brundin, P.; Sherer, T. B. (2016). "Nilotinib - Differentiating the Hope from the Hype". Journal of Parkinson's Disease. 6 (3): 519–22. doi:10.3233/JPD-160904. PMC 5044778. PMID 27434298.
- "Global Novartis News Archive".
- "Cancer drug prevents build-up of toxic brain protein". MedicalXpress.com. 10 May 2013. Retrieved 11 April 2017.