Stargardt disease
Stargardt disease is the most common inherited single-gene retinal disease.[1] It usually has an autosomal recessive inheritance caused by mutations in the ABCA4 gene. Rarely it has an autosomal dominant inheritance due to defects with ELOVL4 or PROM1 genes. It is characterised by macular degeneration that begins in childhood, adolescence or adulthood, resulting in progressive loss of vision.[2][2]
| Stargardt disease | |
|---|---|
| Other names | Stargardt macular dystrophy & degeneration, juvenile macular degeneration, fundus flavimaculatus |
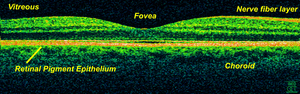 | |
| Optical coherence tomography is used for diagnosis of Stargardt's disease. | |
| Specialty | Ophthalmology |
| Symptoms | Blurred vision |
| Usual onset | Childhood |
| Duration | Lifelong |
| Causes | Genetic |
| Diagnostic method | Slit-lamp |
| Treatment | None |
Signs and symptoms
Presentation usually occurs in childhood or adolescence, though there is no upper age limit for presentation. The main symptom is loss of visual acuity, uncorrectable with glasses. This is manifest as the loss of the ability to see fine details when reading or seeing distant objects. Symptoms typically develop before age 20 (median age of onset: ~17 years old),[3] and include: wavy vision, blind spots, blurriness, loss of depth perception, sensitivity to glare, impaired colour vision,[3] and difficulty adapting to dim lighting (delayed dark adaptation). There is a wide variation between individuals in the symptoms experienced as well as the rate of deterioration in vision. Peripheral vision is usually less affected than fine, central (foveal) vision.
Genetics
Historically from Stargardt’s first description of his eponymous disease until recently, the diagnosis was based on looking at the phenotype using examination and investigation of the eye. Since the advent of genetic testing, the picture has become more complex. What was thought to be one disease is, in fact, probably at least three different diseases, each related to a different genetic change. Therefore it is currently a little confusing to define what Stargardt's disease is. It is certainly caused by defects in the ABCA4 gene, but whether changes to other genes such as PROM1 or ELOVL4, or missense mutations play a role remains to be seen.
The carrier frequency in the general population of ABCA4 alleles is 5 to 10%.[4] Different combinations of ABCA4 genes will result in widely different age of onset and retinal pathology. The severity of the disease is inversely proportional to ABCA4 function and it is thought that ABCA4 related disease has a role to play in other diseases such as retinitis pigmentosa, cone-rod dystrophies and age-related macular degeneration (AMD).[5]
- STGD1: By far the most common form of Stargardt disease is the recessive form caused by mutations in the ABCA4 gene.[6]
- STGD4: A rare dominant defect in the PROM1 gene.[7][5]
- STGD3: A rare dominant form of Stargardt disease caused by mutations in the ELOVL4 gene.
- Late-onset Stargardt disease is associated with missense mutations outside known functional domains of ABCA4.[5]
Pathophysiology
In STGD1, the genetic defect causes malfunction of the ATP-binding cassette transporter (ABCA4) protein of the visual phototransduction cycle. Defective ABCA4 leads to improper shuttling of vitamin A throughout the retina, and accelerated formation of toxic vitamin A dimers (also known as bisretinoids), and associated degradation byproducts. Vitamin A dimers and other byproducts are widely accepted as the cause of STGD1. As such, slowing the formation of vitamin A dimers might lead to a treatment for Stargardt. When vitamin A dimers and byproducts damage the retinal cells, fluorescent granules called lipofuscin in the retinal pigmented epithelium of the retina[8] appear, as a reflecting such damage.
In STGD4, a butterfly pattern of dystrophy is caused by mutations in a gene that encodes a membrane bound protein that is involved in the elongation of very long chain fatty acids (ELOVL4)[9]
Diagnosis
Diagnosis is firstly clinical through history and examination usually with a Slit-lamp. If characteristic features are found the investigations undertaken will depend on locally available equipment and may include Scanning laser ophthalmoscopy which highlights areas of autofluorescence which are associated with retinal pathology. Spectral-domain optical coherence tomography, electroretinography and microperimetry are also useful for diagnostic and prognostic purposes. These investigations may be followed by genetic testing but this is not essential until treatment is available. Fluorescein angiography is used less often than in the past.
Treatment
At present there is no treatment. However, ophthalmologists recommend measures that could slow the rate of progression of the disease. There are no prospective clinical trials to support the recommendations but they are based on scientific understanding of the mechanisms underlying the disease pathology. There are three strategies doctors recommend for potential harm reduction: reducing retinal exposure to damaging ultra violet light, avoiding foods rich in Vitamin A with the hope of lowering lipofuscin accumulation and maintaining good general health and diet.
Ultra-violet light has more energy and is more damaging colour than visible light. In an effort to mitigate this, some ophthalmologists may recommend that the patient wears a broad-brimmed hat or sunglasses when they are outdoors. Sometimes, doctors also instruct their patients to wear yellow-tinted glasses (which filter out blue light) when indoors and in artificial light or in front of a digital screen.
Foods, especially carrots, and vitamin supplements rich in vitamin A are considered to be harmful. Foods with a high vitamin A content are often yellow or orange in color, such as squash, pumpkin, and sweet potato but some, such as liver, are not.
Smoking, being overweight, and eating unhealthily may also contribute to more rapid degeneration. On the other hand, the consumption of oily fish, in a diet similar to that which doctors recommend for age related macular degeneration, can be used to slow the progression of the disease.
Prognosis
The long-term prognosis for patients with Stargardt disease is widely variable and depends on the age of onset and genetic alleles. The majority of people will progress to legal blindness.[10] Stargardt disease has no impact on general health and life expectancy is normal.[11] Some patients, usually those with the late onset form, can maintain a relatively high visual acuity over several years.[12]
Epidemiology
A 2017 prospective epidemiologic study which recruited 81 patients with STGD over 12 months reported an incidence of between 1 and 1.28 per 10 000 individuals. The median age of presentation was 27 years (range 5-64 years), most (90%) were symptomatic, with a median visual acuity of Snellen equivalent 20/66.[13]
History
Karl Stargardt (1875 – 1927) was a German ophthalmologist born in Berlin. He studied medicine at the University of Kiel, qualifying in 1899. He later became head of the Bonn University’s ophthalmology clinic, followed by a post as chair of ophthalmology at the University of Marburg. In 1909 he described 7 patients with a recessively inherited macular dystrophy, now known as Stargardt’s disease.[14][15][16]
Research
There are early stage clinical trials involving several potential therapeutic areas, gene therapy, stem cell therapy, drug therapy and artificial retinas. In general all are testing the safety and benefits of their respective therapies in phase I or II trials. These studies are designed to evaluate the safety, dose and effectiveness in small number of people in Phase I with Phase II evaluating similar criteria in a larger population but including a greater insight into potential side effects.
Gene therapy is designed to insert a copy of a corrected gene into retinal cells. The hope is to return cell function back to normal and the treatment has the potential to stop disease progression. This therapy will not restore impaired vision back to normal. The research is being undertaken by a partnership between Sanofi and Oxford BioMedica. A Lentiviral vector is used to deliverer normal genes to the eye via a subretinal injection. The therapy is known as SAR422459 and it is in Phase I/II trials at present (2018).[17]
Stem-cell therapy involves injecting cells with the potential to mature into differentiated and functioning retinal cells. This therapy has the potential stop disease progression and in the long term improve vision. To improve vision this technique will need to replicate the complex multi-layered and neurally anatomy of the retina. There are a number of research groups working with stem cells one of which is Ocata Therapeutics.[18]
Alkeus Pharma is evaluating the potential of deuterated vitamin A as the drug ALK-001. The hope is that the deuterated vitamin A will reduce the build-up of toxic vitamin A metabolites in the retina and therefore slow rate of visual deterioration. To create deuterated vitamin A some of the hydrogen atoms are replaced with the isotope deuterium which has an extra neutron and is therefore twice the standard atomic weight of hydrogen. Patients taking this drug will need to have a diet with very low levels of naturally occurring Vitamin A. A Phase II clinical trial is taking place using ALK-001 that should report in January 2019.[19][20]
Retinal implants are in the early stages of development and their use could be of benefit to many people with Visual impairment though implanting and maintaining an electrical device within the eye that interfaces with the optic nerve presents many challenges. An example of a device is made by Argus retinal prosthesis, the camera is an external device held on spectacles, the camera signal is processed and then fed via wires into the retina to terminate in some electrodes that interface with the optic nerve.[21]
References
- Clinical Characteristics and Current Therapies for Inherited Retinal Degenerations Jose ́ -Alain Sahel
- "Stargardt disease : Definition(s) from the Unified Medical Language System ® Diseases Database". diseasesdatabase.com. Retrieved 5 February 2018.
- "Stargardt disease/Fundus flavimaculatus - EyeWiki". eyewiki.aao.org. Retrieved 5 February 2018.
- Yatsenko et al. 2001
- "Stargardt disease/Fundus flavimaculatus - EyeWiki".
- http://omim.org/entry/601691
- http://omim.org/entry/604365
- Adler L, 4th; Boyer, NP; Chen, C; Ablonczy, Z; Crouch, RK; Koutalos, Y (2015). The 11-cis Retinal Origins of Lipofuscin in the Retina. Progress in Molecular Biology and Translational Science. 134. pp. e1–12. doi:10.1016/bs.pmbts.2015.07.022. ISBN 9780128010594. PMID 26310175.
- Deutman, August; Hoyng, Carol; van Lith-Verhoeven, Janneke (2006). "Macular dystrophies". Retina (4 ed.). Elsevier Mosby. pp. 1171-4.
- Yanoff, Myron; Duker, Jay S. (2008). Ophthalmology (3rd ed.). Edinburgh: Mosby. pp. 560–562. ISBN 978-0323057516.
- Stargardt Disease from The University of Arizona College of Medicine, Department of Ophthalmology and Vision Science. Retrieved Jan 2012
- Lambertus, Stanley; Lindner, Moritz; Bax, Nathalie M.; Mauschitz, Matthias M.; Nadal, Jennifer; Schmid, Matthias; Schmitz-Valckenberg, Steffen; den Hollander, Anneke I.; Weber, Bernhard H. F. (2016-10-05). "Progression of Late-Onset Stargardt Disease". Investigative Ophthalmology & Visual Science. 57 (13): 5186–5191. doi:10.1167/iovs.16-19833. ISSN 1552-5783. PMID 27699414.
- The Epidemiology of Stargardt Disease in the United Kingdom Kurt Spiteri Cornish, FRCOphth, Jason Ho, FRCOphth, Susan Downes, FRCOphth, Neil W. Scott, PhD, James Bainbridge, PhD, Noemi Lois, MD, PhD © 2017 by the American Academy of Ophthalmolog
- synd/2306 at Who Named It?
- K. B. Stargardt (1909), "Über familiäre, progressive Degeneration in der Makulagegend des Auges", Albrecht von Graefes Archiv für Ophthalmologie (in German), 71 (3), pp. 534–550, doi:10.1007/BF01961301
- Stargardt, K. (1909). "Über familiäre, progressive Degeneration in der Maculagegend des Auges". Albrecht von Græfe's Archiv für Ophthalmologie. 71 (3): 534–550. doi:10.1007/BF01961301.
- https://www.clinicaltrials.gov/ct2/show/NCT01367444?term=SAR422459&rank=1
- Schwartz, SD; Regillo, CD; Lam, BL; Eliott, D; Rosenfeld, PJ; Gregori, NZ; Hubschman, JP; Davis, JL; Heilwell, G; Spirn, M; Maguire, J; Gay, R; Bateman, J; Ostrick, RM; Morris, D; Vincent, M; Anglade, E; Del Priore, LV; Lanza, R (7 February 2015). "Human embryonic stem cell-derived retinal pigment epithelium in patients with age-related macular degeneration and Stargardt's macular dystrophy: follow-up of two open-label phase 1/2 studies". Lancet. 385 (9967): 509–16. doi:10.1016/s0140-6736(14)61376-3. PMID 25458728.
- https://www.clinicaltrials.gov/ct2/show/NCT02402660
- "Alkeus Pharma - Stargardt disease: The leading cause of juvenile macular degeneration".
- Chuang, AT; Margo, CE; Greenberg, PB (July 2014). "Retinal implants: a systematic review". The British Journal of Ophthalmology. 98 (7): 852–6. doi:10.1136/bjophthalmol-2013-303708. PMID 24403565.
External links
| Classification |
|---|