Central serous retinopathy
Central serous retinopathy (CSR), also known as central serous chorioretinopathy (CSC or CSCR), is an eye disease that causes visual impairment, often temporary, usually in one eye.[1][2] When the disorder is active it is characterized by leakage of fluid under the retina that has a propensity to accumulate under the central macula. This results in blurred or distorted vision (metamorphopsia). A blurred or gray spot in the central visual field is common when the retina is detached. Reduced visual acuity may persist after the fluid has disappeared.[1]
| Central serous retinopathy | |
|---|---|
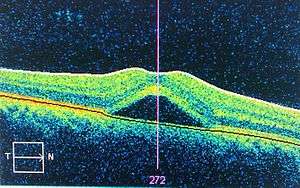 | |
| An occurrence of central serous retinopathy of the fovea centralis imaged using Optical coherence tomography. | |
| Specialty | Ophthalmology |
The disease is considered of unknown cause. It mostly affects white males in the age group 20 to 50 (male:female ratio 6:1)[3] and occasionally other groups. The condition is believed to be exacerbated by stress or corticosteroid use.[4]
Causes
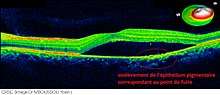
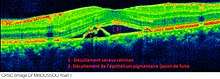
CSR is a fluid detachment of macula layers from their supporting tissue. This allows choroidal fluid to leak beneath the retina. The buildup of fluid seems to occur because of small breaks in the retinal pigment epithelium.
CSR is sometimes called idiopathic CSR which means that its cause is unknown. Nevertheless, stress appears to play an important role. An oft-cited but potentially inaccurate conclusion is that persons in stressful occupations, such as airplane pilots, have a higher incidence of CSR.
CSR has also been associated with cortisol and corticosteroids. Persons with CSR have higher levels of cortisol.[5] Cortisol is a hormone secreted by the adrenal cortex which allows the body to deal with stress, which may explain the CSR-stress association. There is extensive evidence to the effect that corticosteroids (e.g. cortisone), commonly used to treat inflammations, allergies, skin conditions and even certain eye conditions, can trigger CSR, aggravate it and cause relapses.[6][7][8] In a study documented by Indian Journal of Pharmacology, a young male was using Prednisolone and began to display subretinal fluid indicative of CSR. With the discontinuation of the steroid drop the subretinal fluid resolved and did not show any sign of recurrence. Thus indicating the steroid was the probable cause of the CSR.[9] A study of 60 persons with Cushing's syndrome found CSR in 3 (5%).[10] Cushing's syndrome is characterized by very high cortisol levels. Certain sympathomimetic drugs have also been associated with causing the disease.[11]
Evidence has also implicated helicobacter pylori (see gastritis) as playing a role.[12][13] It would appear that the presence of the bacteria is well correlated with visual acuity and other retinal findings following an attack.
Evidence also shows that sufferers of MPGN type II kidney disease can develop retinal abnormalities including CSR caused by deposits of the same material that originally damaged the glomerular basement membrane in the kidneys.[14]
Diagnosis
The diagnosis usually starts with a dilated examination of the retina, followed with confirmation by optical coherence tomography and fluorescein angiography. The angiography test will usually show one or more fluorescent spots with fluid leakage. In 10%-15% of the cases these will appear in a "classic" smoke stack shape. Differential diagnosis should be immediately performed to rule out retinal detachment, which is a medical emergency.
A clinical record should be taken to keep a timeline of the detachment. An Amsler grid can be useful in documenting the precise area of the visual field involved. The affected eye will sometimes exhibit a refractive spectacle prescription that is more far-sighted than the fellow eye due to the decreased focal length caused by the raising of the retina.
Indocyanine green angiography can be used to assess the health of the retina in the affected area which can be useful in making a treatment decision.
Treatment
Most eyes with CSR undergo spontaneous resorption of subretinal fluid within 3–4 months. Recovery of visual acuity usually follows. Treatment should be considered if resorption does not occur within 3–4 months,[15] spontaneously or as the result of counselling.[1]
Any ongoing corticosteroid treatment should be tapered and stopped, where possible. It is important to check current medication, including nasal sprays and creams, for ingredients of corticosteroids, if found seek advice from a medical practitioner for an alternative.
Oral medications
Spironolactone is a mineralocorticoid receptor antagonist that has been proven to help reduce the fluid associated with CSR. In a study noted by Acta Ophthalmologica, spironolactone improved visual acuity in CSR patients over the course of 8 weeks.[16]
Epleronone is another mineralocorticoid receptor antagonist that has been proven to reduce the subretinal fluid that is present with CSR. In a study noted in International Journal of Ophthalmology, results showed Epleronone decreased the subretinal fluid both horizontally and vertically over time. Though after stopping the medication, the fluid also appeared to return and patients needed further treatment.[17]
Low dosage ibuprofen has been shown to quicken recovery in some cases.[18]
Topical treatment
Though no topical treatment has been proven to be effective in the treatment of CSR. Some doctors have attempted to use nonsteroidal topical medications to reduce the subretinal fluid associated with CSR. The nonsteroidal topical medications that are sometimes used to treat CSR are, Ketorolac, Diclofenac, or Bromfenac.[19]
Lifestyle changes
People who have irregular sleep patterns, type A personalities, sleep apnea, or systemic hypertension are more susceptible to CSR, as stated in Medscape. “The pathogenesis here is thought to be elevated circulating cortisol and epinephrine, which affect the autoregulation of the choroidal circulation.” [20] With management of these lifestyle patterns and associated cortisol and epinephrine levels, it has been shown that the fluid associated with CSR can spontaneously resolve. Melatonin has been shown to help regulate sleep in people who have irregular sleep patterns (such as 3rd shift workers, or overnight employees), in turn better regulating cortisol and epinephrine levels to manage CSR.
Laser treatment
Laser photocoagulation, which effectively burns the leak area shut, may be considered in cases where there is little improvement in a 3- to 4-month duration, and the leakage is confined to a single or a few sources of leakage at a safe distance from the fovea. Laser photocoagulation is not indicated for cases where the leak is very near the central macula or for cases where the leakage is widespread and its source is difficult to identify. Laser photocoagulation can permanently damage vision where applied. Carefully tuned lasers can limit this damage.[21] Even so, laser photocoagulation is not a preferred treatment for leaks in the central vision and is considered an outdated treatment by some doctors.[15] Foveal attenuation has been associated with more than 4 months' duration of symptoms, however a better long-term outcome has not been demonstrated with laser photocoagulation than without photocoagulation.[1]
In chronic cases, transpupillary thermotherapy has been suggested as an alternative to laser photocoagulation where the leak is in the central macula.[22]
Photodynamic therapy (PDT) with verteporfin has shown promise as an effective treatment with minimal complications.[23] Follow-up studies have confirmed the treatment's long-term effectiveness[24] including its effectiveness for the chronic variant of the disease.[25] Indocyanine green angiography can be used to predict how the patient will respond to PDT.[15][26]
Yellow micropulse laser has shown promise in very limited trials.[4]
A Cochrane review seeking to compare the effectiveness of various treatment for CSR found low quality evidence that half-dose PDT treatment resulted in improved visual acuity and less recurrence of CSR in patients with acute CSR, compared to patients in the control group.[27] The review also found benefits in micropulse laser treatments, where patients with acute and chronic CSR had improved visual acuity compared to control patients.[27]
Prognosis
The prognosis for CSR is generally excellent. While immediate vision loss may be as poor as 20/200 in the affected eye, clinically, over 90% of patients regain 20/25 vision or better within 45 days.[1] Once the fluid has resolved, either spontaneously or through treatment, distortion is reduced and visual acuity improves as the eye heals. However, some visual abnormalities can remain even where visual acuity is measured at 20/20. Lasting problems include decreased night vision, reduced color discrimination, and localized distortion caused by scarring of the sub-retinal layers.[28]
Complications include subretinal neovascularization and pigment epithelial detachment.[29]
The disease can re-occur causing progressive vision loss. There is also a chronic form, titled as type II central serous retinopathy, which occurs in approximately 5% of cases. This exhibits diffuse rather than focalized abnormality of the pigment epithelium, producing a persistent subretinal fluid. The serous fluid in these cases tends to be shallow rather than dome shaped. Prognosis for this condition is less favorable and continued clinical consultation is advised.
See also
References
- Wang, Maria; Munch, Inger Christine; Hasler, Pascal W.; Prünte, Christian; Larsen, Michael (2008). "Central serous chorioretinopathy". Acta Ophthalmologica. 86 (2): 126–45. doi:10.1111/j.1600-0420.2007.00889.x. PMID 17662099.
- Quillen, DA; Gass, DM; Brod, RD; Gardner, TW; Blankenship, GW; Gottlieb, JL (1996). "Central serous chorioretinopathy in women". Ophthalmology. 103 (1): 72–9. doi:10.1016/s0161-6420(96)30730-6. PMID 8628563.
- https://www.nature.com/articles/s41433-019-0381-7
- André Maia (February 2010). "A New Treatment for Chronic Central Serous Retinopathy". Retina Today. Archived from the original on 2012-08-09. Retrieved 2013-08-11. Cite journal requires
|journal=(help) - Garg, S P; Dada, T.; Talwar, D.; Biswas, N R (1997). "Endogenous cortisol profile in patients with central serous chorioretinopathy". British Journal of Ophthalmology. 81 (11): 962–4. doi:10.1136/bjo.81.11.962. PMC 1722041. PMID 9505819.
- Pizzimenti, Joseph J.; Daniel, Karen P. (2005). "Central Serous Chorioretinopathy After Epidural Steroid Injection". Pharmacotherapy. 25 (8): 1141–6. doi:10.1592/phco.2005.25.8.1141. PMID 16207106.
- Bevis, Timothy; Ratnakaram, Ramakrishna; Smith, M Fran; Bhatti, M Tariq (2005). "Visual loss due to central serous chorioretinopathy during corticosteroid treatment for giant cell arteritis". Clinical and Experimental Ophthalmology. 33 (4): 437–9. doi:10.1111/j.1442-9071.2005.01017.x. PMID 16033370.
- Fernández Hortelano, A; Sádaba, LM; Heras Mulero, H; García Layana, A (2005). "Coroidopatía serosa central como complicación de epitelitis en tratamiento con corticoides" [Central serous chorioretinopathy as a complication of epitheliopathy under treatment with glucocorticoids]. Archivos de la Sociedad Española de Oftalmología (in Spanish). 80 (4): 255–8. doi:10.4321/S0365-66912005000400010. PMID 15852168.
- Shah SP, Desai CK, Desai MK, Dikshit RK (2011). "Steroid-induced central serous retinopathy". Indian J Pharmacol. 43 (5): 607–8. doi:10.4103/0253-7613.84985. PMC 3195140. PMID 22022013.
- Bouzas, Evrydiki A.; Scott, MH; Mastorakos, G; Chrousos, GP; Kaiser-Kupfer, MI (1993). "Central Serous Chorioretinopathy in Endogenous Hypercortisolism". Archives of Ophthalmology. 111 (9): 1229–33. doi:10.1001/archopht.1993.01090090081024. PMID 8363466.
- Michael, John C; Pak, John; Pulido, Jose; De Venecia, Guillermo (2003). "Central serous chorioretinopathy associated with administration of sympathomimetic agents". American Journal of Ophthalmology. 136 (1): 182–5. doi:10.1016/S0002-9394(03)00076-X. PMID 12834690.
- Ahnoux-Zabsonre, A.; Quaranta, M.; Mauget-Faÿsse, M. (2004). "Prévalence de l'Helicobacter pylori dans la choriorétinopathie séreuse centrale et l'épithéliopathie rétinienne diffuse" [Prevalence of Helicobacter pylori in central serous chorioretinopathy and diffuse retinal epitheliopathy: a complementary study]. Journal Français d'Ophtalmologie (in French). 27 (10): 1129–33. doi:10.1016/S0181-5512(04)96281-X. PMID 15687922.
- Cotticelli, L; Borrelli, M; d'Alessio, AC; Menzione, M; Villani, A; Piccolo, G; Montella, F; Iovene, MR; Romano, M (2006). "Central serous chorioretinopathy and Helicobacter pylori". European Journal of Ophthalmology. 16 (2): 274–8. doi:10.1177/112067210601600213. PMID 16703546.
- Colville, Deb; Guymer, Robyn; Sinclair, Roger A; Savige, Judy (2003). "Visual impairment caused by retinal abnormalities in mesangiocapillary (membranoproliferative) glomerulonephritis type II ('dense deposit disease')". American Journal of Kidney Diseases. 42 (2): E2–5. doi:10.1016/S0272-6386(03)00665-6. PMID 12900843.
- Boscia, Francesco (April 2010). "When to Treat and Not to Treat Patients With Central Serous Retinopathy". Retina Today. Archived from the original on 2012-10-17.
- Lee J.Y. (2016). "Spironolactone in the treatment of nonresolving central serous chorioretinopathy: a comparative analysis". Acta Ophthalmologica. 94. doi:10.1111/j.1755-3768.2016.0285.
- Singh RP, Sears JE, Bedi R, Schachat AP, Ehlers JP, Kaiser PK (2015). "Oral eplerenone for the management of chronic central serous chorioretinopathy". Int J Ophthalmol. 8 (2): 310–4. doi:10.3980/j.issn.2222-3959.2015.02.17. PMC 4413566. PMID 25938046.
- Pecora, JL (10 November 1978). "Ibuprofen in the treatment of central serous chorioretinopathy". Ann Ophthalmol. 10 (11): 1481–3. PMID 727624.
- "Retinal Physician - Central Serous Chorioretinopathy and Topical NSAIDs". Retinal Physician. Archived from the original on 30 August 2017. Retrieved 15 October 2017.
- "Central Serous Chorioretinopathy: Background, Pathophysiology, Epidemiology". 16 March 2017. Archived from the original on 16 October 2017. Retrieved 15 October 2017 – via eMedicine. Cite journal requires
|journal=(help) - Roider, Johann; Brinkmann, R; Wirbelauer, C; Laqua, H; Birngruber, R (1999). "Retinal Sparing by Selective Retinal Pigment Epithelial Photocoagulation". Archives of Ophthalmology. 117 (8): 1028–34. doi:10.1001/archopht.117.8.1028. PMID 10448745.
- Wei, SY; Yang, CM (2005). "Transpupillary thermotherapy in the treatment of central serous chorioretinopathy". Ophthalmic Surgery, Lasers & Imaging. 36 (5): 412–5. doi:10.3928/1542-8877-20050901-11. PMID 16238041.
- Ober, Michael D.; Yannuzzi, Lawrence A.; Do, Diana V.; Spaide, Richard F.; Bressler, Neil M.; Jampol, Lee M.; Angelilli, Allison; Eandi, Chiara M.; Lyon, Alice T. (2005). "Photodynamic Therapy for Focal Retinal Pigment Epithelial Leaks Secondary to Central Serous Chorioretinopathy". Ophthalmology. 112 (12): 2088–94. doi:10.1016/j.ophtha.2005.06.026. PMID 16325707.
- Chan, Wai-Man; Lai, Timothy Y.Y.; Lai, Ricky Y.K.; Liu, David T.L.; Lam, Dennis S.C. (2008). "Half-Dose Verteporfin Photodynamic Therapy for Acute Central Serous Chorioretinopathy". Ophthalmology. 115 (10): 1756–65. doi:10.1016/j.ophtha.2008.04.014. PMID 18538401.
- Karakus SH, Basarir B, Pinarci EY, Kirandi EU, Demirok A (May 2013). "Long-term results of half-dose photodynamic therapy for chronic central serous chorioretinopathy with contrast sensitivity changes". Eye (Lond). 27 (5): 612–20. doi:10.1038/eye.2013.24. PMC 3650272. PMID 23519277.
- Inoue, Ryo; Sawa, Miki; Tsujikawa, Motokazu; Gomi, Fumi (2010). "Association Between the Efficacy of Photodynamic Therapy and Indocyanine Green Angiography Findings for Central Serous Chorioretinopathy". American Journal of Ophthalmology. 149 (3): 441–6.e1–2. doi:10.1016/j.ajo.2009.10.011. PMID 20172070.
- Salehi M, Wenick AS, Law HA, Evans JR, Gehlbach P (2015). "Interventions for central serous chorioretinopathy: a network meta-analysis". Cochrane Database Syst Rev. 12 (12): CD011841. doi:10.1002/14651858.CD011841.pub2. PMC 5030073. PMID 26691378.
- Baran, Nergis V; Gurlu, Vuslat P; Esgin, Haluk (2005). "Long-term macular function in eyes with central serous chorioretinopathy". Clinical and Experimental Ophthalmology. 33 (4): 369–72. doi:10.1111/j.1442-9071.2005.01027.x. PMID 16033348.
- Kanyange, ML; De Laey, JJ (2002). "Long-term follow-up of central serous chorioretinopathy (CSCR)". Bulletin de la Societe Belge d'Ophtalmologie (284): 39–44. PMID 12161989.
External links
| Classification | |
|---|---|
| External resources |