Microperimetry
Microperimetry, sometimes called Fundus related perimetry, is a type of visual field test[1] which uses one of several technologies to create a "retinal sensitivity map" of the quantity of light perceived in specific parts of the retina[2] in people who have lost the ability to fixate on an object or light source. The main difference with traditional perimetry instruments is that, microperimetry includes a system to image the retina and an eye tracker to compensate eye movements during visual field testing.
Usage
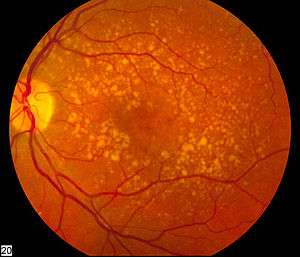
Visual field testing is widely used to monitor pathologies affecting the periphery of vision such as glaucoma.[3] During a conventional test, patients are asked to look steady (fixate) at a visual target, while light stimuli are projected at varying intensities in different retinal locations. This process is not, however, considered accurate in the evaluation of pathologies affecting the central part of the retina (macula and fovea centralis) patients with these pathologies are often unable to fixate reliably. By contrast, fundus perimetry, produces reliable results even in patients with unstable or eccentric fixation.,[4] or advance macular degeneration.
When central vision is compromised, as in the case of macular scotoma, patients develop an eccentric or extra-foveal vision,[5] normally with unstable fixation.[6] The retinal area used by eccentric viewers to substitute the foveal vision is known as the Preferred Retinal Locus (PRL)[7] In Microperimetry systems, the fundus (eye) is imaged in real time, while an eye tracker compensates eye movements during stimuli projection, allowing correct matching between expected and projected stimulus position onto the retina. Simultaneously, the eye tracker plots the retinal movement during fixation attempt defining the PRL zone as well as fixation stability.[8] Some microperimetry instruments calculate 2 different PRL zones during the examination.[9] To create the fundus image an infrared telecamera is used, as in the case of the "Nidek-MP1", or a Scanning Laser Ophthalmoscope (SLO),[10] as in the case of the "Centervue-MAIA".
Microperimetry with Biofeedback
In patients with central vision loss, microperimetry experts are able to analyse the eccentric retina in order to find zones with good retinal sensitivity. Once the best retinal area is selected, patients are asked to move their gaze towards that direction, while audio signals guide them to the desired target. This process is called biofeedback, and is based on the theory of brain plasticity.[11] With several training sessions, some patients are able to gain better use of their peripheral vision.[3]
References
- Glaucoma Diagnosis, Structure and function, pp. 83-92. Edited by Robert N. Weinreb and Erik L. Greve. 2004 Kugler Publications, The Hague, The Netherlands
- Visual Fields, pp. 1-5. Edited by Oxford University Press. David B. Henson.
- Markowitz, Samuel N.; Reyes, Sophia V. (2013-10-01). "Microperimetry and clinical practice: an evidence-based review". Canadian Journal of Ophthalmology. 48 (5): 350–357. doi:10.1016/j.jcjo.2012.03.004. ISSN 0008-4182. PMID 24093179.
- Rohrschneider K.; Bultmann S.; Springer C. (2008). "Use of fundus perimetry (microperimetry) to quantify macular sensitivity". Progress in Retinal and Eye Research. 27 (5): 536–548. doi:10.1016/j.preteyeres.2008.07.003. PMID 18723109.
- Schuchard R. A. (2005). "Preferred retinal loci and macular scotoma characteristics in patients with age-related macular degeneration". Can J Ophthalmol. 40 (3): 303–12. doi:10.1016/s0008-4182(05)80073-0. PMID 15947800.
- Fujii GY, de Juan E, Sunness J, Humayun MS, Pieramici DJ, Chang TS (2002). "Patient selection for macular translocation surgery using the scanning laser ophthalmoscope". Ophthalmology. 109 (9): 1737–1744. doi:10.1016/S0161-6420(02)01120-X. PMID 12208725.
- Schacknow, Paul N.; Samples, John R. (2010-06-10). The Glaucoma Book: A Practical, Evidence-Based Approach to Patient Care. Springer. ISBN 9780387767000.
- Midena E.; Radin P. P.; Pilotto E.; Ghirlando A.; Convento E.; Varano M. (2004). "Fixation pattern and macular sensitivity in eyes with subfoveal choroidal neovascularization secondary to age-related macular degeneration. A microperimetry study". Semin. Ophthalmol. 19 (1–2): 55–61. doi:10.1080/08820530490882896. PMID 15590535.
- Morales M. U.; Saker S.; Mehta R. L.; Rubinstein M.; Amoaku W. M. (2013). "Preferred retinal locus profile during prolonged fixation attempts". Can J Ophthalmol. 48 (5): 368–374. doi:10.1016/j.jcjo.2013.05.022. PMID 24093182.
- Vujosevic S.; Smolek M. K.; Lebow K. A.; Notaroberto N.; Pallikaris A.; Casciano M. (2011). "Detection of macular function changes in early (AREDS 2) and intermediate (AREDS 3) age-related macular degeneration". Ophthalmologica. 225 (3): 155–160. doi:10.1159/000320340. PMID 21150232.
- Tarita-Nistor L.; Gonzalez E. G.; Markowitz S. N.; Steinbach M. J. (2009). "Plasticity of fixation in patients with central vision loss". Vis. Neurosci. 26 (5–6): 487–494. doi:10.1017/s0952523809990265. PMID 20003597.
Further reading
- Midena, Edoardo (2013-12-12). Microperimetry and Multimodal Retinal Imaging. Springer Science & Business Media. ISBN 9783642403002.