Rotavirus
On this Page
Rotavirus
- First identified as cause of diarrhea in 1973
- Most common cause of severe gastroenteritis in infants and children
- Nearly universal infection by age 5 years
- Responsible for up to 500,000 diarrheal deaths each year worldwide
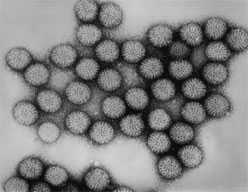
Diarrheal disease has been recognized in humans since antiquity. Until the early 1970s, a bacterial, viral, or parasitic etiology of diarrheal disease in children could be detected in fewer than 30% of cases. In 1973, Bishop and colleagues observed a virus particle in the intestinal tissue of children with diarrhea by using electron micrography. This virus was subsequently called “rotavirus” because of its similarity in appearance to a wheel (rota is Latin for wheel). By 1980, rotavirus was recognized as the most common cause of severe gastroenteritis in infants and young children in the United States. It is now known that infection with rotavirus is nearly universal, with almost all children infected by 5 years of age. Prior to vaccine implemenation, rotavirus was responsible for 20-60 deaths per year in the United States and up to 500,000 deaths from diarrhea worldwide. A vaccine to prevent rotavirus gastroenteritis was first licensed in August 1998 but was withdrawn in 1999 because of its association with intussusception. Second-generation vaccines were licensed in 2006 and 2008.
Rotavirus
- Reovirus (RNA)
- VP7 and VP4 proteins define virus serotype and induce neutralizing antibody
- From 1996-2005, five predominant strains in U.S. (G1-G4, G9) accounted for 90% of isolates
- G1 strain accounts for 75% of infections
- Very stable and may remain viable for weeks or months if not disinfected
Rotavirus
Rotavirus is a double-stranded RNA virus of the family Reoviridae. The virus is composed of three concentric shells that enclose 11 gene segments. The outermost shell contains two important proteins—VP7, or G-protein, and VP4, or P-protein. VP7 and VP4 define the serotype of the virus and induce neutralizing antibody that is probably involved in immune protection. From 1996 through 2005, five strains of rotavirus (G1-4, G9) accounted for 90% of isolates from children younger than 5 years in the United States. Of these, the G1 strain accounted for more than 75% of isolates.
Rotavirus is very stable and may remain viable in the environment for weeks or months if not disinfected.
Rotaviruses cause infection in many species of mammals, including cows and monkeys. These animal strains are antigenically distinct from those causing human infection, and they rarely cause infection in humans.
Rotavirus Pathogenesis
- Entry through mouth
- Replication in epithelium of small intestine
- In severe infections — rotavirus antigen detectable in serum
- Infection leads to isotonic diarrhea
Rotavirus Immunity
- Antibody against VP7 and VP4 probably important for protection
- First infection usually does not lead to permanent immunity
- Reinfection can occur at any age
- Subsequent infections generally less severe
Rotavirus Clinical Features
- Short incubation period (usually less than 48 hours)
- First infection after age 3 months generally most severe
- May be asymptomatic or result in severe dehydrating diarrhea with fever and vomiting
- Gastrointestinal symptoms generally resolve in 3 to 7 days
Rotavirus Complications
- Severe diarrhea
- Dehydration
- Electrolyte imbalance
- Metabolic acidosis
- Immunodeficient children may have more severe or persistent disease
Pathogenesis
The virus enters the body through the mouth. Viral replication occurs in the villous epithelium of the small intestine. Recent evidence indicates that up to two-thirds of children with severe rotavirus gastroenteritis show the presence of rotavirus antigen in serum (antigenemia). Infection may result in decreased intestinal absorption of sodium, glucose, and water, and decreased levels of intestinal lactase, alkaline phosphatase, and sucrase activity, and may lead to isotonic diarrhea.
The immune correlates of protection from rotavirus are poorly understood. Serum and mucosal antibodies against VP7 and VP4 are probably important for protection from disease. Cell-mediated immunity probably plays a role in recovery from infection and in protection.
Recovery from a first rotavirus infection usually does not lead to permanent immunity. After a single natural infection, 38% of children are protected against any subsequent rotavirus infection, 77% are protected against rotavirus diarrhea, and 87% are protected against severe diarrhea. Reinfection can occur at any age. Subsequent infections confer progressively greater protection and are generally less severe than the first.
Clinical Features
The incubation period for rotavirus diarrhea is short, usually less than 48 hours. The clinical manifestations of infection vary and depend on whether it is the first infection or reinfection. The first infection after 3 months of age is generally the most severe. Infection may be asymptomatic, may cause self-limited watery diarrhea, or may result in severe dehydrating diarrhea with fever and vomiting. Up to one-third of infected children may have a temperature greater than 102°F (39°C). The gastrointestinal symptoms generally resolve in 3 to 7 days.
The clinical features and stool characteristics of rotavirus diarrhea are nonspecific, and similar illness may be caused by other pathogens. As a result, confirmation of a diarrheal illness as rotavirus requires laboratory testing.
Complications
Rotavirus infection in infants and young children can lead to severe diarrhea, dehydration, electrolyte imbalance, and metabolic acidosis. Children who are immunocompromised because of congenital immunodeficiency or because of bone marrow or solid organ transplantation may experience severe or prolonged rotavirus gastroenteritis and may have evidence of abnormalities in multiple organ systems, particularly the kidney and liver.
Laboratory Diagnosis
The most widely available method for confirmation of rotavirus infection is detection of rotavirus antigen in stool by enzyme-linked immunoassay (EIA). Several commercial test kits are available that detect an antigen common to human rotaviruses. These kits are simple to use, inexpensive, and very sensitive. Other techniques (such as electron microscopy, reverse transcription polymerase chain reaction, nucleic acid hybridization, sequence analysis, and culture) are used primarily in research settings. Rotavirus antigen has also been identified in the serum of patients 3-7 days after disease onset, but at present, routine diagnostic testing is based primarily on testing of fecal specimens.
Epidemiology
Rotavirus Epidemiology
- Reservoir
- Human —GI tract and stool
- Transmission
- Fecal-oral, fomites
- Temporal pattern
- Fall and winter (temperate areas)
- Communicability
- 2 days before to 10 days after onset of symptoms
Occurrence
Rotavirus occurs throughout the world. The incidence of rotavirus is similar in developed and developing countries, suggesting that improved sanitation alone is not sufficient to prevent the infection.The prevalence of specific rotavirus strains varies by geographic area.
Reservoir
The reservoir of rotavirus is the gastrointestinal tract and stool of infected humans. Although rotavirus infection occurs in many nonhuman mammals, transmission of animal rotaviruses to humans is believed to be rare and probably does not lead to clinical illness. Although immunodeficient persons may shed rotavirus for a prolonged period, a true carrier state has not been described.
Transmission
Rotaviruses are shed in high concentration in the stool of infected persons. Transmission is by fecal-oral route, both through close person-to-person contact and by fomites (such as toys and other environmental surfaces contaminated by stool). Transmission of rotavirus through contaminated water or food appears to be uncommon.
Temporal Pattern
In temperate climates, disease is more prevalent during fall and winter. In the United States in the prevaccine period, annual epidemic peaks usually progressed from the Southwest during November and December to the Northeast by April and May. Following vaccine introduction, the seasons have become shorter with overall less notable differences in timing by geographic region. In tropical climates, the disease is less seasonal than in temperate areas.
Communicability
Rotavirus is highly communicable, as evidenced by the nearly universal infection of children by age 5 years in the prevaccine era. Infected persons shed large quantities of virus in their stool beginning 2 days before the onset of diarrhea and for up to 10 days after onset of symptoms. Rotavirus may be detected in the stool of immunodeficient persons for more than 30 days after infection. Spread within families, institutions, hospitals, and child care settings is common.
Rotavirus Disease in the United States Pre and Post Vaccine Introduction
Rotavirus Disease in the United States
- Estimated 3 million cases per year*
- 95% of children infected by 5 years of age
- Annually* responsible for:
- more than 400,000 physician visits
- more than 200,000 emergency dept visits
- 55,000 to 70,000 hospitalizations
- 20 to 60 deaths
- Annual direct and indirect costs are estimated at approximately $1 billion
- Highest incidence among children 3 to 35 months
of age
*Prevaccine era
Rotavirus infection is not nationally notifiable in the United States. Estimates of incidence and disease burden are based on special surveys, cohort studies, and hospital discharge data.
In the prevaccine era an estimated 3 million rotavirus infections occurred every year in the United States and 95% of children experienced at least one rotavirus infection by age 5 years. Rotavirus infection was responsible for more than 400,000 physician visits, more than 200,000 emergency department (ED) visits, 55,000 to 70,000 hospitalizations, and 20 to 60 deaths each year in children younger than 5 years. Annual direct and indirect costs were estimated at approximately $1 billion, primarily due to the cost of time lost from work to care for an ill child.
In the prevaccine era, rotavirus accounted for 30% to 50% of all hospitalizations for gastroenteritis among U.S. children younger than 5 years of age; the incidence of clinical illness was highest among children 3 to 35 months of age. Infants younger than 3 months of age have relatively low rates of rotavirus infection, probably because of passive maternal antibody, and possibly breastfeeding. Rotavirus infection of adults is usually asymptomatic but may cause diarrheal illness.
Rotavirus activity has been monitored through data on routine testing for rotavirus performed at a set of clinical laboratories across the country. Rotavirus activity in the United States decreased significantly after introduction of rotavirus vaccine in 2006. The 2010-2011 rotavirus season was 8 weeks shorter in duration than the prevaccine baseline. The threshold for the start of the rotavirus season was never achieved nationally during the 2011-2012 season. During these seasons, nationally, the number of positive rotavirus tests declined 74-90% compared with the prevaccine baseline and the total number of tests performed annually declined 28%-36%. The annual proportion positive at the 25 consistently reporting laboratories remained below 10% in both seasons compared with a prevaccine baseline median of 26%. A pattern of biennial increases in rotavirus activity emerged during the 5 postvaccine seasons from 2007-2012, but activity remained substantially below prevaccine levels.
The reduction in rotavirus disease burden in the United States following vaccine introduction has been documented in many different evaluations, including those using data on hospitalizations and emergency room care for diarrhea among young children. Following RV5 introduction in 2006, an estimated 40,000 to 60,000 fewer diarrhea-associated hospitalizations occurred in 2008 in the United States among young children, compared with the prevaccine period. In this season, there was evidence that disease reduction also occurred among children too old to have received vaccine, suggesting indirect protection to unvaccinated and previously uninfected children. Diarrhea hospitalizations during the 2009 rotavirus season were also lower than in the prevaccine period, but greater than the number in 2008, suggesting no indirect benefit in 2009.
Rotavirus Vaccines
Rotavirus Vaccines
- RV5 (RotaTeq)
- contains five reassortant rotaviruses developed from human and bovine parent rotavirus strains
- vaccine viruses suspended in a buffer solution
- contains no preservatives or thimerosal
- RV1 (Rotarix)
- contains one strain of live attenuated human rotavirus (type G1PA[8])
- provided as a lyophilized powder that is reconstituted before administration
- contains no preservatives or thimerosal
The first rotavirus vaccines were derived from either bovine (cow) or rhesus (monkey) origin. Studies demonstrated that these live oral vaccines could prevent rotavirus diarrhea in young children, but efficacy varied widely. Because immunity to G (VP7) or P (VP4) proteins was associated with disease protection and recovery, new live virus vaccines were developed that incorporated G proteins or both G and P proteins for each of the predominant serotypes.
In 1998, a rhesus-based tetravalent rotavirus vaccine (RRV-TV, Rotashield) was licensed and recommended for routine immunization of U.S. infants. However, RRV-TV was withdrawn from the U.S. market within 1 year of its introduction because of its association with intussusception. The risk of intussusception was most elevated (more than a 20-fold increase) within 3 to 14 days after receipt of the first dose of RRV-TV, with a smaller (approximately 5-fold) increase in risk within 3 to 14 days after the second dose. Overall, the risk associated with the first dose of RRV-TV was estimated to be about one case per 10,000 vaccine recipients. Some researchers have suggested that the relative risk of intussusception associated with the first dose of RRV-TV increased with increasing age at vaccination.
Characteristics
There are currently two rotavirus vaccines licensed for use in the United States. RV5 (RotaTeq) is a live oral vaccine manufactured by Merck and licensed by the Food and Drug Administration in February 2006. RV5 contains five reassortant rotaviruses developed from human and bovine parent rotavirus strains. Each 2-mL vial of vaccine contains approximately 2 x 106 infectious units of each of the five reassortant strains. The vaccine viruses are suspended in a buffer solution that contains sucrose, sodium citrate, sodium phosphate monobasic monohydrate, sodium hydroxide, polysorbate 80, and tissue culture media. Trace amounts of fetal bovine serum might be present. The vaccine contains no preservatives or thimerosal.
Fecal shedding of vaccine virus was evaluated in a subset of persons enrolled in the phase III trials. Vaccine virus was shed by 9% of 360 infants after dose 1, but none of 249 and 385 infants after doses 2 and 3, respectively. Shedding was observed as early as 1 day and as late as 15 days after a dose. The potential for transmission of vaccine virus was not assessed in trials. In a post-licensure evaluation in the United States, stool samples were collected from infants for 9 days following the first dose. Rotavirus antigen was detected in stool of 21% of 103 infants, as early as day 3 post vaccination and as late as day 9.
RV1 (Rotarix), a live oral vaccine manufactured by GlaxoSmithKline, was licensed by the FDA in April 2008. RV1 contains one strain of live attenuated human strain 89-12 (type G1P1A[8]) rotavirus. RV1 is provided as a lyophilized powder that is reconstituted before administration. Each 1-mL dose of reconstituted vaccine contains at least 106 median cell culture infective units of virus. The vaccine contains amino acids, dextran, Dulbecco’s modified Eagle medium, sorbitol and sucrose. The diluent contains calcium carbonate, sterile water and xanthan. The vaccine contains no preservatives or thimerosal.
Fecal shedding of rotavirus antigen was evaluated in all or a subset of infants from seven studies in various countries. After dose 1, rotavirus antigen shedding was detected by EIA in 50% to 80% (depending on the study) of infants at approximately day 7 and 0 to 24% at approximately day 30. After dose 2, rotavirus antigen shedding was detected in 4% to 18% of infants at approximately day 7, and 0 to 1.2% at approximately day 30. The potential for transmission of vaccine virus was assessed in a clinical trial among twin pairs (with one twin receiving the vaccine and the other not receiving vaccine) in the Dominican Republic. This study showed evidence of vaccine strain transmission in 19% of the unvaccinated twins, and seroconversion in 21% of the unvaccinated twins.
Rotavirus Vaccine Efficacy
- Any rotavirus gastroenteritis: 74%-87%
- Severe gastroenteritis: 85%-98%
Both vaccines significantly reduced physician visits for diarrhea, and reduced rotavirus-related hospitalization
Porcine circovirus type 1 has been detected in RV1 and porcine circovirus type 1 and type 2 DNA fragments have been detected in RV5. There is no evidence that the virus is a safety risk or causes illness in humans.
Vaccine Efficacy
In the main Phase III RV5 clinical efficacy evaluation, conducted in Finland and United States, the efficacy of the three-dose series against G1-G4 rotavirus gastroenteritis of any severity was 74%, and against severe G1-G4 rotavirus gastroenteritis (defined by severity of fever, vomiting, diarrhea and changes in behavior) was 98% during the first full rotavirus season after vaccination. In a large healthcare utilization study evaluating children during the first 2 years of life, RV5 vaccine reduced the incidence of office visits for G1-G4 rotavirus gastroenteritis by 86%, ED visits for that outcome by 94%, and hospitalizations for that outcome by 96%.
The main Phase III clinical efficacy trials of RV1 were conducted in Latin America and Europe. In the Latin American study, the efficacy of the 2-dose series against severe (a clinical definition) rotavirus gastroenteritis to age 1 year was 85%. In the European study, the efficacy against severe rotavirus gastroenteritis (based on a clinical scoring system that evaluated fever, vomiting, diarrhea, dehydration and treatment) was 96% through the first rotavirus season, and against any rotavirus gastroenteritis was 87%. In the European study, RV1 reduced hospitalization for rotavirus gastroenteritis by 96% through the second season.
RV5 was introduced in the United States in 2006 and RV1 was introduced in 2008; hence most post-introduction data from the United States are based on RV5. Several RV5 case-control vaccine effectiveness evaluations have been performed in the United States and have demonstrated the 3-dose series is highly effective (~85% or greater) against rotavirus disease resulting in emergency department care/hospitalization in young children. US vaccine effectiveness evaluations for RV1 are being completed.
Duration of Immunity
The duration of immunity from rotavirus vaccine is not precisely known. In the main clinical trials described above, good efficacy was demonstrated through 2 rotavirus seasons or to age 2 years (depending on the study design) for both vaccines. In case-control vaccine effectiveness evaluations conducted in the United States after vaccine introduction, high effectiveness for RV5 has been demonstrated during the first 3 years of life against rotavirus disease resulting in emergency department care/hospitalization. US vaccine effectiveness evaluations for RV1 are being completed. In low-income countries, rotavirus vaccine efficacy or effectiveness has generally been lower in the second year of life compared with the first year.
Vaccination Schedule and Use
Rotavirus Vaccine Recommendations
- Similar estimates of efficacy and safety between RV1
and RV5 - No preference for one vaccine over the other
- Routine vaccination of all infants without a contraindication
- 2 (RV1) or 3 (RV5) oral doses beginning at 2 months of age
- may be started as early as 6 weeks of age
- For both rotavirus vaccines
- maximum age for first dose is 14 weeks 6 days*
- minimum interval between doses is 4 weeks
- maximum age for any dose is 8 months 0 days
- ACIP did not define a maximum interval between doses
- No rotavirus vaccine should be administered to infants older than 8 months 0 days**
- It is not necessary to restart the series or add doses because of a prolonged interval between doses
*This is an off-label recommendation for both vaccines, because the labeled maximum age for the first dose of RV5 is 12 weeks
**This is an off-label recommendation for both vaccines, because the labeled maximum age for RV1 is 24 weeks, and the labeled maximum age for RV5 is 32 weeks
Revised ACIP recommendations for the use of rotavirus vaccine were published in MMWR in February 2009. Because of similar estimates of efficacy and safety, neither The Advisory Committee on Immunization Practices (ACIP) nor the Academies of Pediatrics or Family Physicians state a preference for one vaccine over the other.
ACIP recommends routine rotavirus vaccination of all infants without a contraindication. The vaccine should be administered as a series of either two (at ages 2 and 4 months) or three (at ages 2, 4, and 6 months) oral doses, for RV1 and RV5, respectively. The vaccination series for both vaccines may be started as early as 6 weeks of age. The minimum interval between doses is 4 weeks. Rotavirus vaccine should be given at the same visit as other vaccines given at these ages.
The ACIP developed age recommendations that vary from those of the manufacturers. ACIP recommendations state that the maximum age for the first dose of both vaccines is 14 weeks 6 days. This is an off-label recommendation for RV5 since the product information states a maximum age of 12 weeks. The minimum interval between doses of both rotavirus vaccines is 4 weeks. The maximum age for any dose of either rotavirus vaccine is 8 months 0 days. No rotavirus vaccine should be administered to infants older than 8 months 0 days of age. This is an off-label recommendation for both vaccines, because the labeled maximum age for RV1 is 24 weeks, and the labeled maximum age for RV5 is 32 weeks.
ACIP did not define a maximum interval between doses. It is preferable to adhere to the recommended interval of 8 weeks. But if the interval is prolonged, the infant can still receive the vaccine as long as it can be given on or before the 8-month birthday. It is not necessary to restart the series or add doses because of a prolonged interval between doses.
There are few data on the safety or efficacy of giving more than one dose, even partial doses close together. ACIP recommends that providers do not repeat the dose if the infant spits out or regurgitates the vaccine. Any remaining doses should be administered on schedule. Doses of rotavirus vaccine should be separated by at least 4 weeks.
ACIP recommends that the rotavirus vaccine series should be completed with the same product whenever possible. However, vaccination should not be deferred if the product used for a prior dose or doses is not available or is not known. In this situation, the provider should continue or complete the series with the product that is available. If any dose in the series was RV5 (RotaTeq) or the vaccine brand used for any prior dose in the series is not known, a total of three doses of rotavirus vaccine should be administered.
Breastfeeding does not appear to diminish immune response to rotavirus vaccine. Infants who are being breastfed should be vaccinated on schedule.
Infants documented to have had rotavirus gastroenteritis before receiving the full course of rotavirus vaccinations should still begin or complete the 2- or 3-dose schedule following the age recommendations, because the initial infection may provide only partial protections against subsequent rotavirus disease.
Contraindications and Precautions to Vaccination
Rotavirus Vaccine Recommendations
- ACIP recommends that providers do not repeat the dose if the infant spits out or regurgitates the vaccine
- Any remaining doses should be administered on schedule
- Doses of rotavirus vaccine should be separated by at least 4 weeks.
- Complete the series with the same product whenever possible
- If product used for a prior dose or doses is not available or not known, continue or complete the series with the product that is available
- If any dose in the series was RV5 (RotaTeq) or the vaccine brand used for any prior dose is not known, a total of 3 doses of rotavirus vaccine should be administered
- Infants documented to have had rotavirus gastroenteritis before receiving the full course of rotavirus vaccinations should still begin or complete the 2- or 3-dose schedule
Rotavirus Vaccine Contraindications
- Severe allergic reaction to a vaccine component (including latex) or following a prior dose of vaccine
- latex rubber is contained in the RV1 oral applicator
- History of intussusception
- Severe combined immunodeficiency (SCID)
Rotavirus vaccine is contraindicated for infants who are known to have had a severe (anaphylactic) allergic reaction to a vaccine component or following a prior dose of rotavirus vaccine. Latex rubber is contained in the RV1 oral applicator, so infants with a severe allergy to latex should not receive RV1. The RV5 dosing tube is latex free.
Some postmarketing studies of the currently licensed vaccines have detected an increased risk for intussusception following rotavirus vaccine administration, particularly during the first week following the first dose of vaccine. As a result, in October 2011, ACIP added a history of intussusception as a contraindication to rotavirus vaccination.
In response to reported cases of vaccine-acquired rotavirus infection in infants with severe combined immunodeficiency (SCID) following rotavirus vaccine administration, ACIP added SCID as a contraindication to rotavirus vaccination in June 2010.
For children with known or suspected altered immunocompetence, ACIP advises consultation with an immunologist or infectious diseases specialist before administration of rotavirus vaccine. Children who are immunocompromised because of congenital immunodeficiency, or hematopoietic stem cell or solid organ transplantation sometimes experience severe, prolonged, and even fatal wild-type rotavirus gastroenteritis.
Limited data are available from clinical trials on the safety of rotavirus vaccines in infants known to be HIV-infected; these infants were clinically asymptomatic or mildly symptomatic (clinical stages I and II according to WHO classification) when vaccinated. The limited data available do not indicate that rotavirus vaccines have a substantially different safety profile in HIV-infected infants that are clinically asymptomatic or mildly symptomatic compared with infants that are not HIV infected. Two other considerations support vaccination of HIV-exposed or infected infants in the United States. First, the HIV diagnosis might not be established in infants born to HIV-infected mothers by the time they reach the age of the first rotavirus vaccine dose. Only 3% percent or less of HIV-exposed infants in the United States will be determined to be HIV infected. Second, vaccine strains of rotavirus are considerably attenuated.
Rotavirus vaccine should generally not be administered to infants with acute, moderate or severe gastroenteritis, or other acute illness until the condition improves. However, infants with mild acute gastroenteritis or other mild acute illness can be vaccinated, particularly if a delay in vaccination will postpone the first dose of vaccine beyond 15 weeks 0 days of age.
Rotavirus Vaccine Precautions*
- Altered immunocompetence, (except severe combined immunodeficiency, which is a contraindication)
- Limited data do not indicate a different safety profile in HIV-infected versus HIV-uninfected infants
- HIV diagnosis not established in infants due for rotavirus vaccine
- Vaccine strains of rotavirus are attenuated
- These considerations support rotavirus vaccination of HIV-exposed or infected infants
- Acute, moderate or severe gastroenteritis or other acute illness
*The decision to vaccinate if a precaution is present should be made on a case-by-case risk and benefit basis.
Rotavirus Vaccine - Conditions Not Considered to be Precautions
- Pre-existing chronic gastrointestinal conditions
- no data available
- ACIP considers the benefits of vaccination to outweigh the theoretic risks
Rotavirus Vaccine and Preterm Infants
- ACIP supports vaccination of a preterm infant if:
- chronological age is at least 6 weeks
- clinically stable; and
- vaccine is administered at time of discharge or after discharge from neonatal intensive care unit or nursery
Available data suggest that preterm infants (i.e., infants born at less than 37 weeks’ gestation) are at increased risk for hospitalization from rotavirus during the first 1 to 2 years of life. In clinical trials, rotavirus vaccine appeared to be generally well tolerated in preterm infants, although relatively small numbers of preterm infants were evaluated. ACIP considers the benefits of rotavirus vaccination of preterm infants to outweigh the risks of adverse events. ACIP supports vaccination of a preterm infant according to the same schedule and precautions as a full-term infant, provided the following conditions are met: the infant’s chronological age is at least 6 weeks, the infant is clinically stable, and the vaccine is administered at the time of discharge or after discharge from the neonatal intensive care unit or nursery. Infants living in households with persons who have or are suspected of having an immunodeficiency disorder or impaired immune status can be vaccinated. ACIP believes that the indirect protection of the immunocompromised household member provided by vaccinating the infant in the household, and thereby preventing wild-type rotavirus disease, outweighs the small risk for transmitting vaccine virus to the immunocompromised household member.
Infants living in households with pregnant women should be vaccinated according to the same schedule as infants in households without pregnant women. Because the majority of women of childbearing age have pre-existing immunity to rotavirus, the risk for infection by the attenuated vaccine virus is considered to be very low. It is prudent for all members of the household to employ measures such as good hand washing after changing a diaper or otherwise coming in contact with the feces of the vaccinated infant.
Adverse Events Following Vaccination
Intussusception
The phase III clinical trials of both vaccines were very large (>60,000 infants each) to be able to study the occurrence of intussusception in vaccine compared with placebo recipients, and no increased risk for intussusception was observed for either vaccine. However, post-licensure monitoring is necessary to evaluate for a possible risk of intussusception at a lower level than that able to be evaluated in the clinical trials. Post-licensure evaluations of RV1 in Mexico identified a low-level increased risk of intussusception in week 1 after dose 1 (approximately 1 to 3 excess intussusception cases per 100,000 first doses). In Australia, a possible risk was identified with both RV5 and RV1, although based on small numbers of cases. US data on RV5 available through February 2010 from the Vaccine Safety Datalink (VSD) did not identify an increased risk of intussusception, but were not able to exclude a risk of the magnitude observed in these other settings. The VSD was unable to assess RV1 at that time because too few doses had been administered. Monitoring in the United States is ongoing. Parents and health care providers should be aware of a possible low-level increased risk of intussusception following rotavirus vaccine.
Adverse Reactions Following Vaccination
Immunosuppressed Household Contacts of Rotavirus Vaccine Recipients
- Infants living in households with persons who have or are suspected of having an immunodeficiency disorder or impaired immune status can be vaccinated
- Protection provided by vaccinating the infant outweighs the small risk of transmitting vaccine virus
Pregnant Household Contacts of Rotavirus Vaccine Recipients
- Infants living in households with pregnant women should be vaccinated
- majority of women of childbearing age have preexisting immunity to rotavirus
- risk for infection by vaccine virus is considered to be very low
Rotavirus Vaccine Adverse Events
- Intussusception
- Postlicensure-evaluation RV1 — 1-3 excess cases per 100,000 first doses, possible risk for RV5 cases too small to confirm
- VAERS — reports show events cluster in 3-6 days following RV5
- Vaccine Safety Datalink — no increased risk of intussusception — unable to assess RV1
In the subset of infants in RV5 clinical trials that were studied in detail for potential adverse events, for the first week after any dose, RV5 recipients had a small but statistically significant increased rate of diarrhea (18.1% in RV5 group, 15.3% in placebo group) and vomiting (11.6% in RV5, 9.9% in placebo). During the 42-day period following any dose, statistically significantly greater rates of diarrhea, vomiting, otitis media, nasopharyngitis and bronchospasm occurred in RV5 recipients compared with placebo recipients.
In the subset of infants in RV1 clincial studies with details on adverse events, for the first week after vaccination, Grade 3 (i.e., those that prevented normal everyday activities) cough or runny nose occurred at a slightly but statsitically higher rate in the RV1 group (3.6 %) compared with placebo group (3.2%). During the 31 day period after vaccination, the following unsolicited adverse events occurred at a statsticially higher incidence among vaccine recipients: irritability (11.4% in RV1 group, 8.7% in placebo group) and flatulence (2.2% in RV1 group, 1.3% in placebo group).
Post-marketing strain surveillance in the United States and other countries has occasionally detected RV5 vaccine reassortant strains in stool samples of children with diarrhea. In some of these reports, the reassortant virus seemed to be the likely cause of the diarrheal illness.
Vaccine Storage and Handling
Rotavirus vaccine should be maintained at refrigerator temperature: 35°F-46°F (2°C-8°C). For complete information on best practices and recommendations please refer to CDC’s Vaccine Storage and Handling Toolkit[4.33 MB, 109 pages].
Rotavirus Surveillance
Rotavirus Vaccine Adverse Reactions
- RV5
- Diarrhea 18.1%
- Vomiting 11.6%
- Also greater rates of otitis media, nasopharyngitis and bronchospasm
- RV1
- Irritability 11.4%
- Cough or runny nose 3.6%
- Flatulence 2.2%
Rotavirus gastroenteritis is not a reportable disease in the United States. Methods of surveillance for rotavirus disease at the national level include review of national hospital discharge databases for rotavirus-specific or rotavirus-compatible diagnoses, surveillance for rotavirus disease at sites that participate in the New Vaccine Surveillance Network, and reports of rotavirus detection from a sentinel system of laboratories. Special evaluations (e.g.,. case control and retrospective cohort methods) have been used to measure the effectiveness of rotavirus vaccine under routine use in the United States. CDC has established a national strain surveillance system of sentinel laboratories that monitors circulating rotavirus strains.
Acknowledgment
The editors thank Dr. Margaret Cortese, CDC for her assistance in updating this chapter.
Selected References
- American Academy of Pediatrics. Rotavirus infections. In:Pickering LK, Baker CJ, Long SS, eds. RedBook: 2009 Report of the Committee on Infectious Diseases. 28th ed. Elk Grove Village, IL: American Academy of Pediatrics, 2009:576-9.
- CDC. Prevention of rotavirus gastroenteritis among infants and children. Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR 2009;58(No. RR-2):1-24.
- CDC. Addition of severe combined immunodeficiency as a contraindication for administration of rotavirus vaccine. MMWR 2010;59(No. 22):687-8.
- CDC. Addition of history of intussusception as a contraindication for rotavirus vaccination. MMWR 2010;59(No. 22);687-8.
- Cortes JE, Curns AT, Tate JE, Cortese MM, Patel MM, Zhou F, Parashar UD. Rotavirus vaccine and health care utilization for diarrhea in U.S. children. N Engl J Med. 2011 Sep 22;365(12):1108-17
- Cortese MM, Leblanc J, White KE, Jerris RC, Stinchfield P, Preston KL, Meek J, Odofin L, Khizer S, Miller CA, Buttery V, Mijatovic-Rustempasic S, Lewis J, Parashar UD, Immergluck LC. Leveraging state immunization information systems to measure the effectiveness of rotavirus vaccine. Pediatrics. 2011 Dec;128(6):e1474-81.
- Curns AT, Steiner CA, Barrett M, Hunter K, Wilson E, Parashar UD. Reduction in acute gastroenteritis hospitalizations among US children after introduction of rotavirus vaccine: analysis of hospital discharge data from 18 US states. J Infect Dis. 2010 Jun 1;201(11):1617-24.
- Fischer TK, Viboud C, Parashar U, et al. Hospitalizations and deaths from diarrhea and rotavirus among children <5 years of age in the United States, 1993-2003. J Infect Dis 2007;195:1117-25.
- Haber P, Patel M, Pan Y, et. Al. Intusussception after rotavirus vaccines reported to U.S. VAERS, 2006-2012. Pediatrics, 2013 May; 131:1042-1049.
- Parashar UD, Hummelman EG, Bresee JS, et al. Global illness and deaths caused by rotavirus disease in children. Emerg Infect Dis 2003;9:565-72.
- Patel MM, López-Collada VR, Bulhões MM, et al. Intussusception risk and health benefits of rotavirus vaccination in Mexico and Brazil. N Engl J Med. 2011 Jun 16;364(24):2283-92.
- Patel MM, Glass R, Desai R, Tate JE, Parashar UD. Fulfilling the promise of rotavirus vaccines: how far have we come since licensure? Lancet Infect Dis. 2012 Jul;12(7):561-70.
- Payne DC, Staat MA, Edwards KM, Szilagyi PG, Weinberg GA, Hall CB, Chappell J, Curns AT, Wikswo M, Tate JE, Lopman BA, Parashar UD; New Vaccine Surveillance Network (NVSN). Direct and indirect effects of rotavirus vaccination upon childhood hospitalizations in 3 US Counties, 2006-2009. Clin Infect Dis. 2011 Aug 1;53(3):245-53.
- Shui IM, Baggs J, Patel M, Parashar UD, Rett M, Belongia EA, Hambidge SJ, Glanz JM, Klein NP, Weintraub E. Risk of intussusception following administration of a pentavalent rotavirus vaccine in US infants. JAMA. 2012 Feb 8;307(6):598-604. doi: 10.1001/jama.2012.97.
- Staat MA, Payne DC, Donauer S, Weinberg GA, Edwards KM, Szilagyi PG, Griffin MR, Hall CB, Curns AT, Gentsch JR, Salisbury S, Fairbrother G, Parashar UD; New Vaccine Surveillance Network (NVSN). Effectiveness of pentavalent rotavirus vaccine against severe disease. Pediatrics. 2011 Aug;128(2):e267-75. doi: 10.1542/peds.2010-3722.
- Tate J, Mutue J, Panozzo C, et al. Sustained decline in rotavirus detections in the United States following the introduction of rotavirus vaccine in 2006. Pediatric Inf Dis 2011, 30:530-4.
- Vesikari T, Matson DO, Dennehy P, et al. Safety and efficacy of a pentavalent human-bovine (WC3) reassortant rotavirus vaccine. N Engl J Med 2006;354:23-33.
- Vesikari T, Karvonen A, Prymula R, et al. Efficacy of human rotavirus vaccine against rotavirus gastroenteritis during the first 2 years of life in European infants: randomized, double-blind controlled study. Lancet 2007;370:1757-63.
- Page last reviewed: November 15, 2016
- Page last updated: September 8, 2015
- Content source:


 ShareCompartir
ShareCompartir