Antigenic Characterization
“Antigens” are molecular structures on the surface of viruses that are recognized by the immune system and are capable of triggering an immune response (antibody production). On influenza viruses, the major antigens are found on the virus’ surface proteins (see Figure 1).
When someone is exposed to an influenza virus (either through infection or vaccination) their immune system makes specific antibodies against the antigens (surface proteins) on that particular influenza virus. The term “antigenic properties” is used to describe the antibody or immune response triggered by the antigens on a particular virus. “Antigenic characterization” refers to the analysis of virus’ antigenic properties to help assess how related it is to another virus.
CDC antigenically characterizes about 2,000 influenza viruses every year to compare how similar currently circulating influenza viruses are to those that were included in the influenza vaccine, and to monitor for changes in circulating influenza viruses. Antigenic characterization can give an indication of the flu vaccine’s ability to produce an immune response against the influenza viruses circulating in people. This information also helps experts decide what viruses should be included in the upcoming season’s influenza vaccine.
Other information that determines how similar a circulating virus is to a vaccine virus or another virus are the results of serology tests and genetic sequencing.
Figure 1. Influenza Virus Features
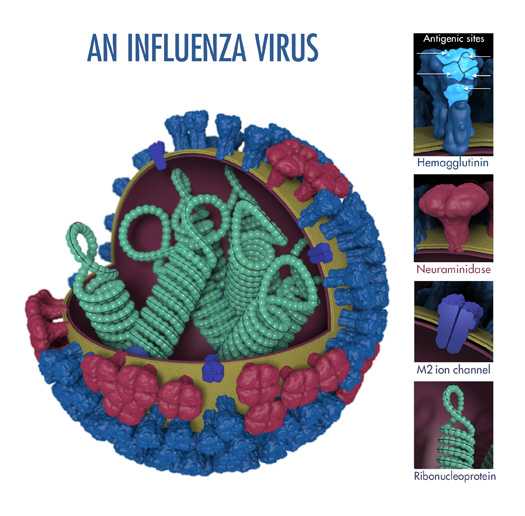
The above image shows the different features of an influenza virus, including the surface proteins hemagglutinin (HA) and neuraminidase (NA). Following influenza infection or receipt of the influenza vaccine, the body’s immune system develops antibodies that recognize and bind to “antigenic sites,” which are regions found on an influenza virus’ surface proteins. By binding to these antigenic sites, antibodies neutralize flu viruses, which prevents them from causing further infection.
The Hemagglutinin Inhibition Assay (HI Test)
Scientists use a test called the hemagglutinin inhibition (HI) assay to antigenically characterize influenza viruses. The HI test works by measuring how well antibodies bind to (and thus inactivate) influenza viruses.
Scientists use the HI test to assess the antigenic similarity between influenza viruses. This test is particularly useful for helping to select the vaccine viruses used in the seasonal flu vaccine. HI test results can tell us whether antibodies developed against vaccination with one virus are antigenically similar enough to another circulating influenza virus to produce an immune response against that circulating virus. Scientists also use the HI test to compare antigenic changes in currently circulating influenza viruses with influenza viruses that have circulated in the past.
The HI test involves three main components: antibodies, influenza virus, and red blood cells that are mixed together in the wells (i.e., cups) of a microtiter plate. (See Image 1.)
Image 1. A Microtiter Plate
A microtiter plate is used to perform the HI test. The plate contains wells (i.e., cup-like depressions that can hold a small amount of liquid) where the solution of antibodies, influenza virus and red blood cells are inserted and allowed to interact. These wells are arranged according to rows and columns (which are identified on the microtiter plate by letters and numbers, respectively). The rows of the plate can be used to test different influenza viruses against the same set of antibodies. The columns can be used to differentiate between greater dilutions of antibodies, like a scale from low to high going from left to right (see Figures 3 and 4 for an example).
The antibodies used in the HI test are obtained by infecting an animal (usually a ferret) that has not been exposed to any influenza virus or vaccine. The animal’s immune system creates antibodies in response to the antigens on the surface of the specific flu virus that was used to infect that animal. To study these antibodies, a sample of blood (serum) is drawn from the animal. The HI test measures how well these antibodies recognize and bind to other influenza viruses (for example, influenza viruses that have been isolated from flu patients). If the ferret antibodies (that resulted from exposure to the vaccine virus) recognize and bind to the influenza virus from a sick patient, this indicates that the vaccine virus is antigenically similar to the influenza virus obtained from the sick patient. This finding has implications for how well the vaccine might work in people. See Flu Vaccine Effectiveness: Questions and Answers for Health Professionals for more information.
As previously mentioned, the influenza viruses used in the HI test are taken from samples from sick people. CDC and other WHO collaborating centers collect specimens from people all over the world to track which influenza viruses are infecting humans and how they are evolving.
For the HI test, red blood cells (RBC) are taken from animals (usually turkeys or guinea pig). They are used in the HI test because influenza viruses bind to them. Normally, RBCs in a solution will sink to the bottom of the assay well and form a red dot at the bottom (Figure 2A). However, when an influenza virus is added to the RBC solution, the virus’ hemagglutinin (HA) surface proteins will bind to multiple RBCs. When influenza viruses bind to the RBCs, the red cells form a lattice structure (Figure 2B). This keeps the RBCs suspended in solution instead of sinking to the bottom and forming the red dot. The process of the influenza virus binding to RBCs to form the lattice structure is called “hemagglutination.”
Figure 2. Components of the HI Assay
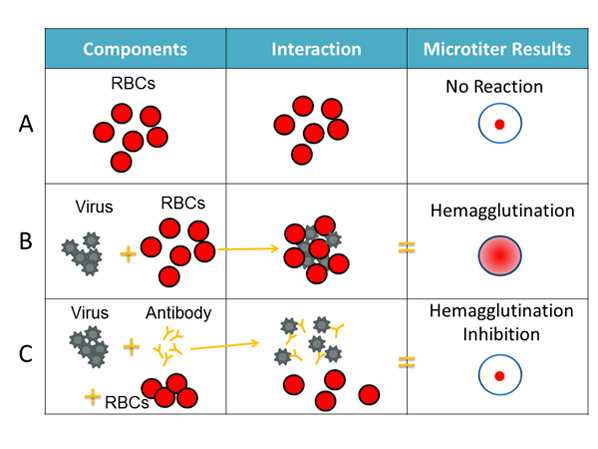
The HI test involves the interaction of red blood cells (RBCs), antibody and influenza virus. Row A shows that in the absence of virus, RBCs in a solution will sink to the bottom of a microtiter plate well and look like a red dot. Row B shows that influenza viruses will bind to red blood cells when placed in the same solution. This is called hemagglutination and is represented by the formation of the lattice structure, depicted in the far right column under “Microtiter Results.” Row C shows how antibodies that are antigenically similar to a virus being tested will recognize and bind to that influenza virus. This prevents the virus and RBCs from binding, and therefore, hemagglutination does not occur (i.e., hemagglutination inhibition occurs instead).
When antibodies are pre-mixed with influenza virus followed by RBCs, the antibodies will bind to influenza virus antigens that they recognize, covering the virus so that its HA surface proteins can no longer bind to RBCs (Figure 2C). The reaction between the antibody and the virus inhibits (i.e., prevents) hemagglutination from occurring, which results in hemagglutination inhibition (as shown in Figure 2C). This is why the assay is called a “hemagglutinin inhibition (HI) test.” Hemagglutination (as depicted in Figure 2B) occurs when antibodies do not recognize and bind to the influenza viruses in the solution, and as a result, the influenza viruses bind to the red blood cells in the solution, forming the lattice structure. When the antibodies do recognize and bind to the influenza viruses in the solution, this shows that the vaccine virus (like the one the ferrets were infected with) has produced an immune response against the influenza virus obtained from the sick patient. When this happens, the influenza virus being tested is said to be “antigenically like” the influenza virus that created the antibodies (from ferrets).
Antibodies do not recognize and bind to antigens from influenza viruses that are antigenically different. If the antibodies do not bind to the antigens on the surface of the influenza virus from the sick patient using the HI assay, hemagglutination occurs. This indicates that the vaccine virus has not caused an immune response against the influenza virus obtained from the sick patient.
Top of PageAssessing Antigenic Similarity Using the HI Test
The HI test assesses the degree of antigenic similarity between two viruses using a scale based on greater dilutions of antibodies. As previously mentioned, the HI test is performed using a microtiter plate. The microtiter plate contains rows and columns of wells (i.e., cups) where RBCs, influenza virus and antibodies (developed against a comparison virus, such as a vaccine virus) are mixed. Dilutions are marked across the top of the microtiter plate. These dilutions function as a scale for assessing antigenic similarity and immune response. By testing the ability of greater dilutions of antibody to prevent hemagglutination, scientists measure how well those antibodies recognize and bind to (and therefor inactivate) an influenza virus. The higher the dilution, the fewer antibodies are needed to block hemagglutination, the more antigenically similar the two viruses being compared are to each other. The highest dilution of antibody that results in hemagglutinin inhibition is considered a virus’s HI titer (Figure 3). Higher HI titers are associated with greater antigenic similarity. Greater antigenic similarity suggests that vaccination would produce an immune response against the test virus.
Figure 3. HI Titer Assay
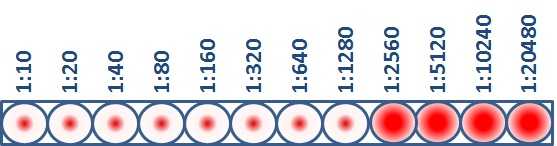
This virus sample has an HI titer of 1280, which means that the greatest dilution of antibody that still blocked hemagglutination from occurring was at 1280 dilution. At this dilution, the antibodies were still capable of recognizing and binding to the antigens on the virus.
Figure 4. Antigenic Characterization Assay
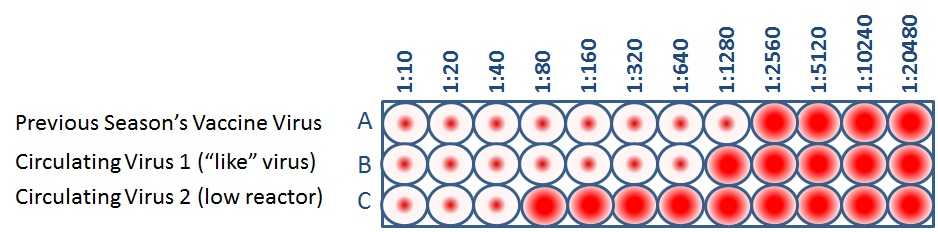
When CDC antigenically characterizes influenza viruses to inform decisions on the formulation of the seasonal flu vaccine, the HI test is used to compare currently circulating viruses (B&C) with vaccine viruses (A). This allows scientists to quickly determine if a virus used in the seasonal flu vaccine is antigenically similar enough to circulating influenza viruses to produce an immune response against them.
Public health experts consider influenza viruses to be antigenically similar or “like” each other if their HI titers differ by two dilutions or less. (This is equivalent to a two-well (i.e., a four-fold dilution) or less difference). Using figure 4 as an example, when circulating virus 1 is compared to a vaccine virus, circulating virus 1 differs by one dilution (a 2-fold difference) and therefore is “like” the previous season’s vaccine virus. However, circulating virus 2 differs by five dilutions (a 32-fold difference) and therefore is not like the previous season’s vaccine virus. Circulating viruses that are antigenically dissimilar (i.e., not “like”) the reference panel are considered “low reactors.”
Limitations
Antigenic characterization gives important information about whether vaccine made using the vaccine virus will protect against circulating influenza viruses, but there are several limitations to antigenic characterization test methodology, which are described below.
Egg Adaptations
Right now, most flu vaccines are made using viruses grown in eggs. As human influenza viruses adapt to grow in eggs, genetic changes can occur in the viruses. These are called “egg-adapted” changes. Some egg-adapted changes may have antigenic (or immunogenic) implications while others may not.
Time from Vaccine Virus Selection to Delivery of Vaccine
Using current vaccine production technology, it takes about 6-8 months from the time that the vaccine virus is chosen to the time when influenza vaccines become widely available. Because influenza viruses are constantly changing, circulating influenza viruses may change during the time between when vaccine viruses are chosen (i.e., February for the Northern Hemisphere flu vaccine) and when the next season begins. If these changes are antigenically significant, it could mean that antibodies created through vaccination may not recognize and inactivate circulating viruses. New technologies to shorten the manufacturing time for production of influenza vaccine could reduce the chances of significant antigenic changes occurring before people can be vaccinated.
Use of Animals
Use of the HI test to assess the similarity of circulating influenza viruses to vaccine viruses involves obtaining antibodies from animals (particularly ferrets). The ferrets used for making antibodies for the HI test are “immunologically naïve,” which means that they have never been exposed to an influenza virus before and have no antibodies against influenza until after they are infected. When ferrets are infected with a live influenza virus they typically produce strong antibody responses against the influenza virus used to infect the ferret but little to no antibody against other influenza strains. As a result, HI tests (when conducted using immunologically naïve ferrets) are the most sensitive method available for detecting antigenic differences between influenza viruses.
Top of Page- Page last reviewed: September 27, 2017
- Page last updated: September 27, 2017
- Content source:
- Centers for Disease Control and Prevention, National Center for Immunization and Respiratory Diseases (NCIRD)
- Page maintained by: Office of the Associate Director for Communication, Digital Media Branch, Division of Public Affairs


 ShareCompartir
ShareCompartir