Diabetes and pregnancy
For pregnant women with diabetes, some particular challenges exist for both mother and child. If the woman has diabetes as an intercurrent disease in pregnancy, it can cause early labor, birth defects, and larger than average infants.
Planning in advance is emphasized if one wants to become pregnant and has type 1 diabetes mellitus or type 2 diabetes mellitus. Stringent blood glucose control is needed before pregnancy.
Physiology
During a normal pregnancy, many maternal physiological changes occur and there is an increase in insulin needs[1] due to increased hormonal secretions that regulate blood glucose levels, glucose-'drain' to the fetus, slowed emptying of the stomach, increased excretion of glucose by the kidneys and resistance of cells to insulin.
Risks for the child
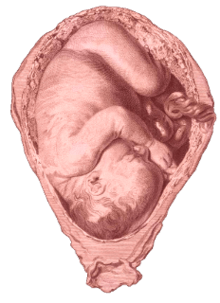
The risks of maternal diabetes to the developing fetus include miscarriage, growth restriction, growth acceleration, fetal obesity (macrosomia), mild neurological deficits,[2] polyhydramnios and birth defects.[3]In some studies 4% to 11% of infants born to type 1 diabetic women had defects compared to 1.2% to 2.1% of infants born in the general population.[4] The cause is, e.g., oxidative stress, by activating protein kinase C[5] that leads to apoptosis of some cells.[5] A hyperglycemic maternal environment has also been associated with neonates that are at greater risk for development of negative health outcomes such as future obesity, insulin resistance, type 2 diabetes mellitus, and metabolic syndrome.[6]
During the first trimester, besides increased birth defect risks, having a miscarriage is also increased due to abnormal development in the early stages of pregnancy.[7]
When blood glucose is not controlled, shortly after birth, the infant's lungs may be under developed and can cause respiratory problems.[3] Hypoglycemia can occur after birth if the mother's blood sugar was high close to the time of delivery, which causes the baby to produces extra insulin of its own.
Mild neurological and cognitive deficits in offspring — including increased symptoms of ADHD, impaired fine and gross motor skills, and impaired explicit memory performance — have been linked to pregestational type 1 diabetes and gestational diabetes.[8][9][10] Prenatal iron deficiency has been suggested as a possible mechanism for these problems.[11]
Birth defects are not currently an identified risk for the child of women with gestational diabetes, since those primarily occur in the latter part of pregnancy, where vital organs already have taken their most essential shape.
Importance of blood glucose level during pregnancy
High blood sugar levels are harmful to the mother and her fetus. Experts advise diabetics to maintain blood sugar level close to normal range for 2 to 3 months before planning for pregnancy. Managing blood sugar close to normal before and during pregnancy helps to protect the health of mother and the baby.
Insulin may be needed for type 2 diabetics instead of oral diabetes medication. Extra insulin may be needed for type 1 diabetics during pregnancy. Doctors may advise to check blood sugar more often to maintain near-normal blood sugar levels.
Diabetes pregnancy management
Blood glucose levels in pregnant woman should be regulated as strictly as possible. Higher levels of glucose early in pregnancy are associated with teratogenic effects on the developing fetus.[12] A Cochrane review published in 2016 was designed to find out the most effective blood sugar range to guide treatment for women who develop gestational diabetes mellitus in their pregnancy. The review concluded that quality scientific evidence is not yet available to determine the best blood sugar range for improving health for pregnant women with diabetes and their babies.[13]
During the first weeks of pregnancy less insulin is required due to tight blood sugar control as well as the extra glucose needed for the growing fetus.[14] At this time basal and bolus insulin may need to be reduced to prevent hypoglycemia. Frequent testing of blood sugar levels is recommended to maintain control. As the fetus grows and weight is gained throughout the pregnancy, the body produces more hormones which may cause insulin resistance and the need for more insulin.[14] At this time it is important for blood sugar levels to remain in range as the baby will produce more of its own insulin to cover its mother's higher blood sugar level which can cause fetal macrosomia.[15] During delivery, which is equivalent to exercise, insulin needs to be reduced again or hyperglycemia can occur. After the baby is delivered and the days following, there are no more hormones from the placenta which demanded more insulin, therefore insulin demand is decreased and gradually returns to normal requirements.[3]
Diabetes mellitus may be effectively managed by appropriate meal planning, increased physical activity and properly-instituted insulin treatment. Some tips for controlling diabetes in pregnancy include:
- Cut down sweets, eats three small meals and one to three snacks a day, maintain proper mealtimes, and include balanced fiber intake in the form of fruits, vegetables and whole-grains.
- Increased physical activity - walking, swimming/aquaerobics, etc.
- Monitor blood sugar level frequently, doctors may ask to check the blood glucose more often than usual.
- The blood sugar level should be below 95 mg/dl (5.3 mmol/l) on awakening, below 140 mg/dl (7.8 mmol/l) one hour after a meal and below 120 mg/dl (6.7 mmol/l) two hours after a meal.
- Each time when checking the blood sugar level, keep a proper record of the results and present to the health care team for evaluation and modification of the treatment. If blood sugar levels are above targets, a perinatal diabetes management team may suggest ways to achieve targets.
- Many may need extra insulin during pregnancy to reach their blood sugar target. Insulin is not harmful for the baby.
Breast feeding
Breast feeding is good for the child even with a mother with diabetes mellitus. Some women wonder whether breast feeding is recommended after they have been diagnosed with diabetes mellitus. Breast feeding is recommended for most babies, including when mothers may be diabetic. In fact, the child's risk for developing type 2 diabetes mellitus later in life may be lower if the baby was breast-fed. It also helps the child to maintain a healthy body weight during infancy. However, the breastmilk of mothers with diabetes has been demonstrated to have a different composition than that of non-diabetic mothers, containing elevated levels of glucose and insulin and decreased polyunsaturated fatty acids.[16] Although benefits of breast-feeding for the children of diabetic mothers have been documented, ingestion of diabetic breast milk has also been linked to delayed language development on a dose-dependent basis.[16]
In some cases, pregnant women with diabetes may be encouraged to express and store their colostrum during pregnancy, in case their blood sugar is too low for feeding the baby breast milk after birth.[17] There is no evidence on the safety or potential benefits when pregnant women with diabetes express and store breast milk prior to the baby's birth.[17]
Classification
The White classification, named after Priscilla White[18] who pioneered research on the effect of diabetes types on perinatal outcome, is widely used to assess maternal and fetal risk. It distinguishes between gestational diabetes (type A) and diabetes that existed before pregnancy (pregestational diabetes). These two groups are further subdivided according to their associated risks and management.[19]
There are 2 classes of gestational diabetes (diabetes which began during pregnancy):
- Class A1: gestational diabetes; diet controlled
- Class A2: gestational diabetes; medication controlled
The second group of diabetes which existed before pregnancy can be split up into these classes:
- Class B: onset at age 20 or older or with duration of less than 10 years
- Class C: onset at age 10-19 or duration of 10–19 years
- Class D: onset before age 10 or duration greater than 20 years
- Class E: overt diabetes mellitus with calcified pelvic vessels
- Class F: diabetic nephropathy
- Class R: proliferative retinopathy
- Class RF: retinopathy and nephropathy
- Class H: ischemic heart disease
- Class T: prior kidney transplant
An early age of onset or long-standing disease comes with greater risks, hence the first three subtypes.
Footnotes
- "Insulin in Obstetrics: a main parameter in the management of pregnancy" (PDF). 1998.
- Ornoy A, Wolf A, Ratzon N, Greenbaum C, Dulitzky M (July 1999). "Neurodevelopmental outcome at early school age of children born to mothers with gestational diabetes". Archives of Disease in Childhood: Fetal and Neonatal Edition. 81 (1): F10–4. doi:10.1136/fn.81.1.F10. PMC 1720965. PMID 10375355.
- Walsh, John (2006). Pumping Insulin. San Diego, California: Torrey Pines Press. p. 288. ISBN 978-1-884804-86-1.
- Walsh, John (2006). Pumping Insulin. Sand Diego, California: Torrey Pines Press. p. 289. ISBN 978-1-884804-86-1.
- Author: Gäreskog, Mattias Title: Teratogenicity Involved in Experimental Diabetic Pregnancy
- Calkins, Kara; Sherin Devaskar (2011). "Fetal Origins of Adult Disease". Curr Probl Pediatr Adolesc Health Care. 41 (6): 158–176. doi:10.1016/j.cppeds.2011.01.001. PMC 4608552. PMID 21684471.
- "First Trimester complications in pregnancy with diabetes". September 2016.
- Nomura Y, Marks DJ, Grossman B, Yoon M, Loudon H, Stone J, Halperin JM (January 2012). "Exposure to Gestational Diabetes Mellitus and Low Socioeconomic Status: Effects on Neurocognitive Development and Risk of Attention-Deficit/Hyperactivity Disorder in Offspring". Archives of Pediatrics & Adolescent Medicine. 166 (4): 337–43. doi:10.1001/archpediatrics.2011.784. PMC 5959273. PMID 22213602.
- Ornoy A, Ratzon N, Greenbaum C, Wolf A, Dulitzky M (2001). "School-age children born to diabetic mothers and to mothers with gestational diabetes exhibit a high rate of inattention and fine and gross motor impairment". Journal of Pediatric Endocrinology & Metabolism : JPEM. 14 Suppl 1: 681–9. doi:10.1515/jpem.2001.14.s1.681. PMID 11393563.
- DeBoer T, Wewerka S, Bauer PJ, Georgieff MK, Nelson CA (August 2005). "Explicit memory performance in infants of diabetic mothers at 1 year of age". Developmental Medicine and Child Neurology. 47 (8): 525–31. doi:10.1017/s0012162205001039. PMC 2829746. PMID 16108452.
- Georgieff MK (March 2006). "The effect of maternal diabetes during pregnancy on the neurodevelopment of offspring". Minnesota Medicine. 89 (3): 44–7. PMID 16669433.
- J Obstet Gynaecol Can 2007;29(11):927–934 http://sogc.org/wp-content/uploads/2013/01/guiJOGC200CPG0711.pdf Archived 2017-08-09 at the Wayback Machine
- Martis, R; Brown, J; Alsweiler, J; Crawford, T; Crowther, CA (2016). "Different intensities of glycaemic control for women with gestational diabetes mellitus". Cochrane Database of Systematic Reviews. 4: CD011624. doi:10.1002/14651858.CD011624.pub2. PMID 27055233.
- Scheiner, Gary (2004). Think like a Pancreas. Da Capo Press. p. 173. ISBN 978-156924-436-4.
- "Infant of Diabetic Mother". Children's Hospital of Philadelphia. 2014-08-24.
- Rodekamp E, Harder T, Kohlhoff R, Dudenhausen JW, Plagemann A (2006). "Impact of breast-feeding on psychomotor and neuropsychological development in children of diabetic mothers: role of the late neonatal period". Journal of Perinatal Medicine. 34 (6): 490–6. doi:10.1515/JPM.2006.095. PMID 17140300.
- East, Christine E.; Dolan, Willie J.; Forster, Della A. (2014-07-30). "Antenatal breast milk expression by women with diabetes for improving infant outcomes" (PDF). The Cochrane Database of Systematic Reviews (7): CD010408. doi:10.1002/14651858.CD010408.pub2. ISSN 1469-493X. PMID 25074749.
- White P (November 1949). "Pregnancy complicating diabetes". Am. J. Med. 7 (5): 609–16. doi:10.1016/0002-9343(49)90382-4. PMID 15396063.
- Gabbe S.G., Niebyl J.R., Simpson J.L. OBSTETRICS: Normal and Problem Pregnancies. Fourth edition. Churchill Livingstone, New York, 2002. ISBN 0-443-06572-1