Chorioamnionitis
Chorioamnionitis also known as intra-amniotic infection (IAI)[1] is an inflammation of the fetal membranes (amnion and chorion) due to a bacterial infection. It typically results from bacteria ascending from the vagina into the uterus and is most often associated with prolonged labor. The risk of developing chorioamnionitis increases with each vaginal examination that is performed in the final month of pregnancy, including during labor.[2]
| Chorioamnionitis | |
|---|---|
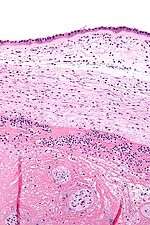 | |
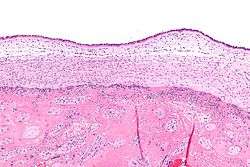
| Micrograph showing chorioamnionitis. The clusters of blue dots are inflammatory cells (neutrophils, eosinophils and lymphocytes). H&E stain. | |
| Specialty | Obstetrics and gynaecology |
Anatomy
The amniotic sac consists of two parts:
- The outer membrane is the chorion. It is closest to the mother and physically supports the much thinner amnion.
- The inner membrane is the amnion. It is in direct contact with the amniotic fluid, which surrounds the fetus.
Diagnosis
Signs and symptoms
Chorioamnionitis is diagnosed clinically in the setting of maternal fever (≥38°C or ≥100.4 °F) and at least two of the following: [3]
- Maternal leukocytosis (>15,000 cells/mm³)
- Maternal tachycardia (>100 bpm)
- Fetal tachycardia (>160 bpm)
- Uterine tenderness
- Foul odor of amniotic fluid[4]
Exclusions:
- Maternal upper respiratory infection.
- Maternal urinary tract infection.
Pathologic
Chorioamnionitis can be diagnosed from a histologic examination of the fetal membranes.
Infiltration of the chorionic plate by neutrophils is diagnostic of (mild) chorioamnionitis. More severe chorioamnionitis involves subamniotic tissue and may have fetal membrane necrosis and/or abscess formation.
Severe chorioamnionitis may be accompanied by vasculitis of the umbilical blood vessels (due to the fetus' inflammatory cells) and, if very severe, funisitis (inflammation of the umbilical cord's connective tissue).
Treatment
Antibiotic Treatment consists of:
- Standard: Ampicillin 2g IV every 6 hours + Gentamicin 1.5 mg/kg every 8 hours
- Alternative: Ampicillin-Sulbactam 3g IV every 5 hours, Ticarcillin-Clavulanate 3.1g IV every 4 hours, Cefoxitine 2g IV every 6 hours
- Cesarean Delivery: Ampicillin 2g IV every 6 hours + Gentamicin 1.5 mg/kg every 8 hours + Clindamycin 900 mg every 8 hours or Metronidazole 500 mg IV every 6 hours
- Penicillin-Allergy: Vancomycin 1g IV every 12 hours + Gentamicin 1.5 mg/kg every 8 hours
However, there is not enough evidence to support the most efficient antimicrobial regimen,[5] starting the treatment during the intrapartum period is more effective than starting it postpartum; it shortens the hospital stay for the mother and the neonate.[6] However, completion of treatment/cure is only considered after delivery.[4]
Associations
Chorioamnionitis is a risk factor for premature birth, periventricular leukomalacia and cerebral palsy.[7]
See also
Notes
- "Intra–Amniotic Infection". Merckmanuals.com/. Retrieved 20 December 2014.
- Seaward, P. G., Hannah, M. E., Myhr, T. L., et al. (1997). International Multicentre Term Prelabor Rupture of Membranes Study: evaluation of predictors of clinical chorioamnionitis and postpartum fever in patients with prelabor rupture of membranes at term. Am J Obstet Gynecol, 177(5), 1024-1029.
- Elmar Peter Sakala, MD, MA, MPH, FACOG. Professor of GYNOB, Loma Linda University of medicine, California. Codirector of Student Clerkship. Dept of GYNOB
- "UpToDate". Uptodate.com. Retrieved 2 July 2018.
- Hopkins, L; Smaill, F (2002). "Antibiotic regimens for management of intraamniotic infection". The Cochrane Database of Systematic Reviews (3): CD003254. doi:10.1002/14651858.CD003254. PMC 6669261. PMID 12137684.
- Chapman, E; Reveiz, L; Illanes, E; Bonfill Cosp, X (19 December 2014). "Antibiotic regimens for management of intra-amniotic infection". The Cochrane Database of Systematic Reviews (12): CD010976. doi:10.1002/14651858.CD010976.pub2. PMID 25526426.
- Wu YW, Colford JM (2000). "Chorioamnionitis as a risk factor for cerebral palsy: A meta-analysis". JAMA. 284 (11): 1417–24. doi:10.1001/jama.284.11.1417. PMID 10989405.
References
- Excess Digital Exams Raise Risk of Chorioamnionitis, Ob. Gyn. News, August 15, 1997
- Centers for disease control and prevention (2002) Prevention of perinatal group B Streptococcal disease: revised guidelines from CDC. MMWR 51:RR-11:1–28
External links
| Classification | |
|---|---|
| External resources |
- Overview at Cleveland Clinic.
- Cerebral palsy inflammation link (29 November 2003) at BBC.