Testing & Diagnosis
On This Page
Assessing Need for Testing
All pregnant women in US states, the District of Columbia, and territories should be screened [PDF – 250 KB] for possible Zika virus exposure and symptoms at each prenatal care visit. Possible exposure to Zika virus that might warrant testing includes:
- Recent travel to or residence in an area with risk of Zika (during pregnancy or the periconceptional period [the 6 weeks before last menstrual period or 8 weeks before conception]), or
- Sex (vaginal, anal, or oral sex) or sharing sex toys without a condom during pregnancy with a person who traveled to or lives in an area with risk of Zika.
In addition, now that Zika is no longer newly introduced in the Americas, healthcare providers should ask patients about potential exposure to Zika before their current pregnancy to help guide decisions about testing and interpretation of test results.
Testing for Zika Virus
Zika virus testing is performed at CDC, at several state, local, and territorial health departments, and at some commercial laboratories. Several tests are available to help determine if a person is infected with Zika virus. Healthcare providers should contact their state or local health department to facilitate testing. See the Testing for Zika Virus webpage for information on how to submit specimens for Zika testing.
Laboratory evidence of a confirmed recent Zika virus infection includes
- Detection of Zika virus or Zika virus RNA or antigen in any body fluid or tissue specimen; or
- Positive or equivocal Zika virus or dengue virus IgM test on serum with a positive titer for Zika virus (≥10) from plaque reduction neutralization testing (PRNT) together with negative PRNT titer (i.e., <10) for dengue virus. Interpretation of serologic results has been described and published in an MMWR article.
When to Test
| If your patient… | Testing recommendation |
|---|---|
| Was exposed to Zika AND has symptoms of Zika virus infection or a history or symptoms at any time during her pregnancy | She should be tested for Zika as soon as possible.
|
| Lives in or frequently travels to an area with risk of Zika but does not have symptoms of Zika virus infection. | She should be offered testing three times during pregnancy using RNA NAT testing. |
| Traveled to or had sex without a condom with a partner who lived in or traveled to an area with risk of Zika but does not have symptoms of Zika virus infection | Testing is not routinely recommended. Testing should be considered using a shared decision-making model that includes pretest counseling, individualized risk assessment, clinical judgment, patient preferences, and the jurisdiction’s recommendations.
|
| Was exposed to Zika AND had birth defects potentially associated with Zika detected on a prenatal ultrasound | Concurrent RNA NAT testing and Zika virus IgM testing is recommended. If amniocentesis is being done for clinical care, healthcare providers should also test the amniotic fluid for Zika genetic material. Testing of placental and fetal tissues may also be considered if results of maternal Zika virus testing are not definitive. |
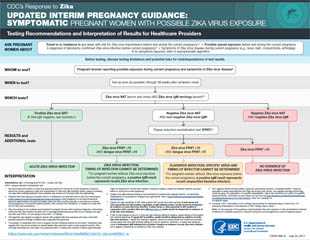
Testing Symptomatic Pregnant Women
Pregnant women who report signs or symptoms consistent with Zika virus disease (acute onset of fever, rash, arthralgia, conjunctivitis) should be tested for Zika virus infection. For symptomatic pregnant women who live in or traveled to an area with risk of Zika or had sex without a condom with a partner who lived in or traveled to an area with risk of Zika, concurrent testing of serum and urine by RNA NAT and Zika virus IgM testing of serum is recommended as soon as possible up through 12 weeks after symptoms began.
- A positive RNA NAT result on both serum and urine, regardless of IgM results, should be interpreted as an acute maternal Zika virus infection.
- A positive RNA NAT result on either serum or urine, in conjunction with a positive Zika IgM, should be interpreted as evidence of acute Zika virus infection.
- A negative RNA NAT result in conjunction with a non-negative Zika virus IgM test result should be followed by plaque reduction neutralization test (PRNT). See laboratory interpretation [PDF – 3 pages] in the absence of PRNT testing.
Testing Asymptomatic Pregnant Women
Asymptomatic pregnant women with ongoing possible Zika virus exposure (i.e., residence in or frequent travel to an area with risk of Zika) should be offered RNA NAT testing three times during pregnancy. Although there is no way to determine the timing of testing of asymptomatic pregnant women with only NAT testing, testing at the initiation of prenatal care with two additional tests performed during the course of the pregnancy, coinciding with prenatal visits should be considered. For this group, testing for Zika virus IgM antibodies is no longer routinely recommended because of the emerging evidence on persistence of Zika IgM antibodies, which could make it difficult for healthcare providers to use these test results to determine whether an infection occurred during the current pregnancy versus prior to conception.
Asymptomatic pregnant women with recent possible exposure to Zika but no ongoing exposure should no longer receive routine testing. Testing should be considered using a shared decision-making model that includes pretest counseling, individualized risk assessment, clinical judgment, patient preferences, and the jurisdiction’s recommendations. If testing is conducted, similar concurrent NAT and IgM testing should be used as is recommended for testing symptomatic pregnant women; however, timeframes for testing should be calculated based on the last possible exposure to Zika. When deciding whether or not to advise testing, healthcare providers should consider factors such as length of possible exposure, type and location of exposure as well potential symptoms, protective measures taken, preferences and concerns, and jurisdiction recommendations.
Note: Jurisdictions may take into account local epidemiologic considerations (e.g., seasonality, geography, and mosquito surveillance and control factors) in making recommendations for Zika virus testing for this group of pregnant women; therefore, testing recommendations for this group of pregnant women may differ by jurisdiction. Please contact your state, tribal, local, or territorial health department for jurisdiction specific guidance.
Testing Pregnant or Postpartum Women with Possible Zika Virus Exposure who Have a Fetus with Prenatal Ultrasound Findings or an Infant with Physical Exam Findings Consistent with Possible Zika Virus-Associated Birth Defects
For pregnant women exposed to Zika whose fetus has birth defects potentially associated with Zika detected on ultrasound or whose infant has physical exam findings consistent with possible Zika-virus associated birth defects, concurrent testing of serum and urine by RNA NAT and Zika virus IgM testing of serum is recommended, following the algorithm for symptomatic pregnant women. If amniocentesis is performed as part of clinical care, healthcare providers should consider RNA NAT testing of amniocentesis specimens and results should be interpreted within the context of the limitations of amniotic fluid testing. It is unknown how sensitive or specific RNA NAT testing of amniotic fluid is for congenital Zika virus infection or what proportion of infants born after infection will have abnormalities.
Testing Partners of Pregnant Women
CDC recommends Zika virus testing for anyone who is not pregnant who has been exposed to Zika and who also has Zika symptoms, including sex partners of pregnant women. See CDC’s webpage for testing recommendations for non-pregnant people.
Testing does not determine how likely a person is to pass Zika virus through sex. Because Zika virus can remain in some fluids (e.g., semen) longer than blood, someone might have a negative blood test, but still carry Zika in their genital secretions.
Further, intermittent shedding in semen can occur with other viruses and the pattern of Zika virus shedding in semen is unknown. In addition, the detection of Zika virus RNA in semen might not indicate the presence of infectious virus in semen. Testing semen and vaginal fluids for Zika virus is not currently available outside of the research setting. Studies are underway to better understand the performance of these tests, the persistence of Zika virus in these fluids, and how best to interpret the results.
Testing Information
For more information on diagnostic testing for Zika, see Testing for Zika.
Specimens
Zika virus RNA NAT and serology assays can be performed on maternal serum. Zika virus RNA NAT can also be performed on maternal whole blood, amniotic fluid, plasma, and urine. Other testing that can be performed includes the following: 1) histopathologic examination and immunohistochemical staining of the placenta and umbilical cord, and 2) Zika virus testing of frozen placental tissue and cord tissue. For a number of reasons, the use of cord blood to diagnose Zika virus infection is not recommended. It is important to work closely with your state or local health department to ensure the appropriate test is ordered and interpreted correctly.
Testing Challenges
RNA NAT testing may not demonstrate Zika virus RNA in a woman with Zika virus infection if the period of viremia has passed. IgM testing should be performed; however, cross-reactivity with related flaviviruses (e.g., dengue and yellow fever viruses) is common. PRNT can be performed to measure virus-specific neutralizing antibodies to Zika virus, but neutralizing antibodies may still yield cross-reactive results in persons who were previously infected with another flavivirus, such as dengue, or has been vaccinated against yellow fever or Japanese encephalitis.
New data suggest that, similar to some other flavivirus infections, Zika virus IgM antibodies may remain in the body for months after infection, making it difficult to use Zika virus IgM tests to determine if women might have been infected before or after they became pregnant. IgM tests are also susceptible to false positives and cross-reactivity with other flaviviruses, especially when an individual has been vaccinated against or previously infected with a related flavivirus. In addition, as the prevalence of Zika virus disease declines, the lower prevalence increases the probability that positive test results are false positives. This new information is particularly relevant for pregnant women who live in or frequently travel to areas with risk of Zika.
Ordering Tests
Each clinical scenario is unique, and healthcare providers should consider all available information when ordering a test for Zika virus infection, including patient travel history or possible exposure through sexual contact, history of flavivirus infection, vaccination history, ultrasound findings, and the presence of symptoms.
All laboratory testing requests and results reports for pregnant women should clearly indicate pregnancy status. This will facilitate prioritization of testing, ascertainment of pregnancies affected by Zika, and consistent interpretation of laboratory results.
Healthcare providers should work closely with the state, local, or territorial health department to ensure that the appropriate test is ordered and interpreted correctly. In addition, CDC maintains a 24/7 Zika consultation service for health officials and healthcare providers caring for pregnant women. To contact the service, email ZIKAMCH@cdc.gov.
More Information
- UPDATE: Interim Guidance for Health Care Providers Caring for Pregnant Women with Possible Zika Virus (MMWR, July 24, 2017)
- HAN Advisory: Prolonged IgM Antibody Response in People Infected with Zika Virus: Implications for Interpreting Serologic Testing Results for Pregnant Women (May 5, 2017)
- HAN Advisory: CDC Guidance for Travel and Testing of Pregnant Women and Women of Reproductive Age for Zika Virus Infection Related to the Investigation for Local Mosquito-borne Zika Virus Transmission in Brownsville, Cameron County, Texas (December 14, 2016)
- HAN Advisory: CDC Updates Guidance for Pregnant Women and Women and Men of Reproductive Age for Zika Virus Infection Related to the Ongoing Investigation of Local Mosquito-borne Zika Virus Transmission in Miami-Dade County, Florida (October 19, 2016)
- HAN Advisory: CDC Guidance for Travel and Testing of Pregnant Women and Women of Reproductive Age for Zika Virus Infection Related to the Investigation for Local Mosquito-borne Zika Virus Transmission in Miami-Dade and Broward Counties, Florida (Aug. 1, 2016)
- Interim Guidance for Health Care Providers Caring for Pregnant Women with Possible Zika Virus Exposure – United States, July 2016
- Page last reviewed: October 3, 2017
- Page last updated: October 3, 2017
- Content source:



 ShareCompartir
ShareCompartir