Pneumocystis pneumonia
Definition
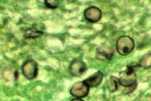
Pneumocystis jirovecii in the lung of an HIV/AIDS patient.
Pneumocystis pneumonia (PCP) is a serious infection caused by the fungus Pneumocystis jirovecii.
Most people who get PCP have a medical condition that weakens their immune system, like HIV/AIDS, or take medicines that lower the body’s ability to fight germs and sickness. In the United States, people with HIV/AIDS are less likely to get PCP today than before the availability of antiretroviral therapy (ART). However, PCP is still a substantial public health problem.1-3 Much of the information we have about PCP and its treatment comes from caring for patients with HIV/AIDS.
Scientists have changed both the classification and the name of this organism since it first appeared in patients with HIV in the 1980s. Pneumocystis jirovecii used to be classified as a protozoan but is now considered a fungus.4 Pneumocystis jirovecii used to be called Pneumocystis carinii. When scientists renamed P. carinii to P. jirovecii, some people considered using the abbreviation “PJP,” but to avoid confusion, Pneumocystis jirovecii pneumonia is still abbreviated “PCP.”5
Symptoms
The symptoms of PCP include1,6
- Fever
- Cough
- Difficulty breathing
- Chest pain
- Chills
- Fatigue (tiredness)
In people with HIV/AIDS, PCP symptoms usually develop over several weeks and include a mild fever. In people who have weakened immune systems for reasons other than HIV/AIDS, PCP symptoms usually develop over a few days, often with a high fever.6,7
Contact your healthcare provider if you have symptoms that you think are related to PCP.
Risk & Prevention
Who gets PCP?
PCP is extremely rare in healthy people, but the fungus that causes this disease can live in their lungs without causing symptoms. In fact, up to 20% of adults might carry this fungus at any given time, and the immune system removes the fungus after several months.8
Most people who get PCP have weakened immune systems, meaning that their bodies don’t fight infections well. About 40% of people who get PCP have HIV/AIDS.7 The other 60% of people who get PCP are usually taking medicine that lowers the body’s ability to fight germs or sickness or have other medical conditions, such as7
- Solid organ transplant
- Blood cancer
- Inflammatory diseases or autoimmune diseases (for example, lupus or rheumatoid arthritis)
- Stem cell transplant
How can I prevent PCP?
There is no vaccine to prevent PCP. A healthcare provider might prescribe medicine to prevent PCP for people who are more likely to develop the disease. The medicine most commonly used to prevent PCP is called trimethoprim/sulfamethoxazole (TMP/SMX), which is also known as co-trimoxazole and by several different brand names, including Bactrim, Septra, and Cotrim. Other medicines are available for people who cannot take TMP/SMX.
Medicine to prevent PCP is recommended for some people infected with HIV, stem cell transplant patients, and some solid organ transplant patients.9-13 Healthcare providers might also prescribe medicine to prevent PCP in other patients, such as people who are taking long-term, high-dose corticosteroids.
Sources
PCP spreads from person to person through the air.14-16 Some healthy adults can carry the Pneumocystis fungus in their lungs without having symptoms, and it can spread to other people, including those with weakened immune systems.8
Many people are exposed to Pneumocystis as children, but they likely do not get sick because their immune systems prevent the fungus from causing an infection.17 In the past, scientists believed that people who had been exposed to Pneumocystis as children could later develop PCP from that childhood infection if their immune systems became weakened.8,18 However, it is more likely that people get PCP after being exposed to someone else who has PCP or who is carrying the fungus in their lungs without having symptoms.
Diagnosis & Testing
PCP is diagnosed using a sample from a patient’s lungs. The sample is usually mucus that is either coughed up by the patient (called sputum) or collected by a procedure called bronchoalveolar lavage. Sometimes, a small sample of lung tissue (a biopsy) is used to diagnose PCP. The patient’s sample is sent to a laboratory, usually to be examined under a microscope. Polymerase chain reaction (PCR) can also be used to detect Pneumocystis DNA in different types of samples. A blood test to detect β-D-glucan (a part of the cell wall of many different types of fungi) can also help diagnose PCP.19
Treatment
PCP must be treated with prescription medicine. Without treatment, PCP can cause death. The most common form of treatment is trimethoprim/sulfamethoxazole (TMP/SMX), which is also known as co-trimoxazole and by several different brand names, including Bactrim, Septra, and Cotrim. This medicine is given by mouth or through a vein for 3 weeks.
TMP/SMX can cause side effects such as rash and fever. Other medicines are available for patients who cannot take TMP/SMX.
Statistics
Before the beginning of the HIV/AIDS epidemic in the 1980s, PCP was uncommon. In fact, clusters of PCP were one of the first signs that the HIV/AIDS epidemic was beginning in the United States.20 PCP soon became one of the main AIDS-defining illnesses in the United States. In the late 1980s, an estimated 75% of people living with AIDS developed PCP.21 Since then, PCP in people living with HIV/AIDS has decreased substantially due to antiretroviral therapy (ART) and preventive treatment with TMP/SMX.2,22,23 However, PCP is still a serious health concern for people living with HIV/AIDS or other conditions that weaken the immune system. It is an opportunistic infection, which means an infection that occurs more frequently and is more severe in people with weakened immune systems. In a study of HIV-infected patients in the United States and Canada, PCP was the most common opportunistic infection during 2008–2010.24 The exact number of cases of PCP in the United States is difficult to determine because there is no national surveillance for the disease. PCP is also a common opportunistic infection among people living with HIV/AIDS in developing countries.25
More Resources
References
- Harris JR, Balajee SA, Park BJ. Pneumocystis jirovecii pneumonia: current knowledge and outstanding public health issues. Curr Fung Infect Rep 2010;4:229-37.
- Kaplan JE, Hanson D, Dworkin MS, et al. Epidemiology of human immunodeficiency virus-associated opportunistic infections in the United States in the era of highly active antiretroviral therapy. Clin Infect Dis 2000;30 Suppl 1:S5-14.
- Morris A, Lundgren JD, Masur H, et al. Current epidemiology of Pneumocystis pneumonia. Emerging infectious diseases 2004;10:1713-20.
- Edman JC, Kovacs JA, Masur H, Santi DV, Elwood HJ, Sogin ML. Ribosomal RNA sequence shows Pneumocystis carinii to be a member of the fungi. Nature 1988;334:519-22.
- Stringer JR, Beard CB, Miller RF, Wakefield AE. A new name (Pneumocystis jiroveci) for Pneumocystis from humans. Emerging infectious diseases 2002;8:891-6.
- Kovacs JA, Hiemenz JW, Macher AM, et al. Pneumocystis carinii pneumonia: a comparison between patients with the acquired immunodeficiency syndrome and patients with other immunodeficiencies. Annals of internal medicine 1984;100:663-71.
- Roux A, Canet E, Valade S, et al. Pneumocystis jirovecii pneumonia in patients with or without AIDS, France. Emerging infectious diseases 2014;20:1490-7.
- Medrano FJ, Montes-Cano M, Conde M, et al. Pneumocystis jirovecii in general population. Emerging infectious diseases 2005;11:245-50.
- Guidelines for the Prevention and Treatment of Opportunistic Infections in HIV-Infected Adults and Adolescents. 2017, at https://aidsinfo.nih.gov/guidelines/html/4/adult-and-adolescent-oi-prevention-and-treatment-guidelines/0.)
- Guidelines for the Prevention and Treatment of Opportunistic Infections in HIV-Exposed and HIV-Infected Children. 2017, at https://aidsinfo.nih.gov/guidelines/html/5/pediatric-oi-prevention-and-treatment-guidelines/0.)
- Tomblyn M, Chiller T, Einsele H, et al. Guidelines for preventing infectious complications among hematopoietic cell transplantation recipients: a global perspective. Biology of blood and marrow transplantation 2009;15:1143-238.
- Stern A, Green H, Paul M, Vidal L, Leibovici L. Prophylaxis for Pneumocystis pneumonia (PCP) in non-HIV immunocompromised patients. The Cochrane database of systematic reviews 2014:CD005590.
- Fishman JA. Prevention of infection caused by Pneumocystis carinii in transplant recipients. Clin Infect Dis 2001;33:1397-405.
- Gianella S, Haeberli L, Joos B, et al. Molecular evidence of interhuman transmission in an outbreak of Pneumocystis jirovecii pneumonia among renal transplant recipients. Transplant infectious disease 2010;12:1-10.
- Mori S, Cho I, Sugimoto M. A cluster of Pneumocystis jirovecii infection among outpatients with rheumatoid arthritis. J Rheumatol 2010;37:1547-8.
- Schmoldt S, Schuhegger R, Wendler T, et al. Molecular evidence of nosocomial Pneumocystis jirovecii transmission among 16 patients after kidney transplantation. Journal of clinical microbiology 2008;46:966-71.
- Pifer LL, Hughes WT, Stagno S, Woods D. Pneumocystis carinii infection: evidence for high prevalence in normal and immunosuppressed children. Pediatrics 1978;61:35-41.
- Wakefield AE, Lindley AR, Ambrose HE, Denis CM, Miller RF. Limited asymptomatic carriage of Pneumocystis jiroveci in human immunodeficiency virus-infected patients. The Journal of infectious diseases 2003;187:901-8.
- Karageorgopoulos DE, Qu JM, Korbila IP, Zhu YG, Vasileiou VA, Falagas ME. Accuracy of beta-D-glucan for the diagnosis of Pneumocystis jirovecii pneumonia: a meta-analysis. Clinical microbiology and infection 2013;19:39-49.
- CDC. Pneumocystis pneumonia–Los Angeles. MMWR Morbidity and mortality weekly report 1981;30:250-2.
- Hay JW, Osmond DH, Jacobson MA. Projecting the medical costs of AIDS and ARC in the United States. Journal of acquired immune deficiency syndromes 1988;1:466-85.
- Buchacz K, Baker RK, Palella FJ, Jr., et al. AIDS-defining opportunistic illnesses in US patients, 1994-2007: a cohort study. Aids 2010;24:1549-59.
- Kelley CF, Checkley W, Mannino DM, Franco-Paredes C, Del Rio C, Holguin F. Trends in hospitalizations for AIDS-associated Pneumocystis jirovecii Pneumonia in the United States (1986 to 2005). Chest 2009;136:190-7.
- Buchacz K, Lau B, Jing Y, et al. Incidence of AIDS-Defining Opportunistic Infections in a Multicohort Analysis of HIV-infected Persons in the United States and Canada, 2000-2010. The Journal of infectious diseases 2016;214:862-72.
- de Armas Rodriguez Y, Wissmann G, Muller AL, et al. Pneumocystis jirovecii pneumonia in developing countries. Parasite 2011;18:219-28.
- Page last reviewed: April 26, 2017
- Page last updated: April 26, 2017
- Content source:


 ShareCompartir
ShareCompartir