Information for Healthcare Professionals about Valley Fever (Coccidioidomycosis)
Clinical features
Symptomatic persons (40% of cases) usually present 1 to 3 weeks after exposure with fatigue, cough, dyspnea, headache, night sweats, myalgias, and rash.1–3 Primary pulmonary disease is often self-limiting, but some patients fail to recover and develop complications or chronic pulmonary disease (approximately 5 to 10% of cases). Disseminated disease occurs in an estimated 1% of cases (higher rates of dissemination are observed in certain risk groups), with bones/joints, soft tissues, and meninges most commonly affected.
Etiologic agent
Coccidioides immitis (typically in California) and Coccidioides posadasii (typically outside of California).4 Clinical differences between the two species have not been observed.
Reservoir and endemic areas
Soil in the southwestern United States, parts of Mexico, and South America. Highly endemic areas include southern Arizona and California’s southern San Joaquin Valley.
Transmission
Coccidioidomycosis is typically acquired via inhalation of airborne arthroconidia, often after disturbance of contaminated soil (e.g., small-scale activities including construction or excavation, or large-scale events such as dust storms and earthquakes). Primary cutaneous coccidioidomycosis,5 solid organ donor-derived coccidioidomycosis,6 and fomite-transmitted coccidioidomycosis 7–8 can also occur but are very uncommon.
Sequelae
In persons who develop progressive, chronic, or disseminated disease, symptoms may persist for months or even longer. Meningitis can lead to permanent neurologic damage. Mortality is high in HIV-infected persons with diffuse lung disease.
Diagnosis
Serologic tests to detect IgM and IgG antibodies are most often used to diagnose coccidioidomycosis.9 Other methods include culture and microscopy.
-
Serology:
-
Enzyme immunoassay (EIA): A very sensitive and commonly used method for diagnosing coccidioidomycosis. Two Coccidioides EIAs are currently available
- Premier ® Coccidioides EIA – Meridian Bioscience, Inc.
- Coccidioides Antibody Enzyme Immunoassay – Immuno Mycologics, Inc. (IMMY)
- Immunodiffusion (ID): detects IgM antibodies; positive early in the course of infection.
- Complement Fixation (CF): detects IgG antibodies and allows for assessment of disease severity.
-
Enzyme immunoassay (EIA): A very sensitive and commonly used method for diagnosing coccidioidomycosis. Two Coccidioides EIAs are currently available
- Culture: Can be performed on tissue and respiratory specimens; however, sputum can be difficult to obtain for culture since patients’ coughs are often non-productive.
- Microscopy: for detection of spherules in tissue or respiratory secretions; low sensitivity.
- Urinary antigen detection: Not widely used, but may have some utility in diagnosing coccidioidomycosis in immunocompromised patients with severe forms of the disease.10
- Polymerase Chain Reaction (PCR): PCR for detection of Coccidioides directly from clinical specimens is still experimental, but promising.11,12

Laboratory culture of Coccidioides immitis
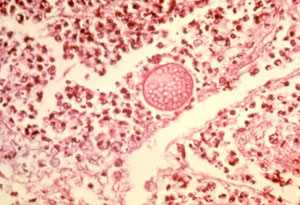
Lung tissue with Coccidioides spherule
Treatment
No evidence from randomized trials exists to determine whether antifungal treatment for uncomplicated coccidioidal infections reduces symptom duration or prevents complications. Some infections will resolve without antifungal treatment. Infectious Diseases Society of America (IDSA) guidelines suggest treatment for primary pulmonary coccidioidomycosis in patients who:
- Are immunosuppressed
- Have severe or significantly debilitating illness
- Have diabetes or are frail because of age or comorbidities
- Are pregnant
- Are of African or Filipino ancestry
Disseminated coccidioidomycosis requires antifungal treatment, typically fluconazole or amphotericin B. For more detailed treatment guidelines, please refer to the Infectious Diseases Society of America’s Practice Guidelines for the Treatment of Coccidioidomycosis.
Risk groups
People in endemic areas, particularly those who have occupations or participate in activities exposing them to dust (e.g., construction or agricultural workers, archaeologists, and military trainees). Risk factors for severe or disseminated coccidioidomycosis include African-American race13 or Filipino ethnicity,14 HIV/AIDS,15 use of immunosuppressive medications,16 organ transplant,17 diabetes mellitus,13 or pregnancy.18
Surveillance and statistics
Coccidioidomycosis is nationally notifiable and is reportable in the following states: Arizona, Arkansas, California, Delaware, Louisiana, Maryland, Michigan, Minnesota, Missouri, Montana, Nebraska, Nevada, New Hampshire, New Mexico, North Dakota, Ohio, Oregon, Rhode Island, South Dakota, Utah, Washington, and Wyoming. Check with your local, state, or territorial public health department for more information about disease reporting requirements and procedures in your area. Click here for coccidioidomycosis statistics.
Areas for further research
- Determining the optimal treatment regimen for primary pulmonary coccidioidomycosis
- Identifying host factors associated with increased risk for dissemination in select racial/ethnic groups to target prevention efforts
- Understanding the factors associated with increasing incidence in endemic areas
- Determining the influence of climate change on Coccidioides’ geographic distribution
- Developing improved methods for detection of Coccidioides in environmental samples
- Creating an effective vaccine
Other resources
-
Continuing Medical Education activity: “Valley Fever: Timely Diagnosis, Early Assessment, and Proper Management.”
- CDC is working to improve awareness about Valley fever (coccidioidomycosis) among healthcare providers. CDC partnered with experts from the University of Arizona and the University of California, Davis to provide provide online continuing education for physicians and nurses.
- MMWR: Summary of Notifiable Diseases, United States
- Valley Fever Center for Excellence Tutorial for Primary Care Professionals [PDF-40 Pages]
- The most recent case definition published by the Council of State and Territorial Epidemiologists (CSTE)
References
- Galgiani JN, Ampel NM, Blair JE, et al. Coccidioidomycosis. Clin Infect Dis 2005;41:1217-23.
- Crum NF, Lederman ER, Stafford CM, Parrish JS, Wallace MR. Coccidioidomycosis: a descriptive survey of a reemerging disease. Clinical characteristics and current controversies. Medicine 2004;83:149-75.
- Thompson GR, 3rd. Pulmonary coccidioidomycosis. Semin Respir Crit Care Med 2011;32:754-63.
- Fisher MC, Koenig GL, White TJ, Taylor JW. Molecular and phenotypic description of Coccidioides posadasii sp. nov., previously recognized as the non-California population of Coccidioides immitis. Mycologia. 2002 Jan-Feb;94(1):73-84.
- Chang A, Tung RC, McGillis TS, Bergfeld WF, Taylor JS. Primary cutaneous coccidioidomycosis. J Am Acad Dermatol. 2003 Nov;49(5):944-9.
- Dierberg KL, Marr KA, Subramanian A, Nace H, Desai N, Locke JE, et al. Donor-derived organ transplant transmission of coccidioidomycosis. Transpl Infect Dis. 2012 Jun;14(3):300-4.
- Dweik M, Baethge BA, Duarte AG. Coccidioidomycosis pneumonia in a nonendemic area associated with infliximab. South Med J. 2007 May;100(5):517-8.
- Stagliano D, Epstein J, Hickey P. Fomite-transmitted coccidioidomycosis in an immunocompromised child. The Pediatric infectious disease journal. 2007 May;26(5):454-6.
- Ampel NM. The diagnosis of coccidioidomycosis. F1000 Med Rep. 2010
- Durkin M, P C, T K, R M, BM K, D B, et al. Diagnosis of Coccidioidomycosis with Use of the Coccidioides Antigen Enzyme Immunoassay. Clin Infect Dis. 2008;47:e69-73.
- Binnicker MJ, Buckwalter SP, Eisberner JJ, Stewart RA, McCullough AE, Wohlfiel SL, et al. Detection of Coccidioides species in clinical specimens by real-time PCR. J Clin Microbiol. 2007 Jan;45(1):173-8.
- Sheff KW, York ER, Driebe EM, et al. Development of a rapid, cost-effective TaqMan Real-Time PCR Assay for identification and differentiation of Coccidioides immitis and Coccidioides posadasii. Med Mycol 2009;48:466-469.
- Rosenstein NE, Emery KW, Werner SB, Kao A, Johnson R, Rogers D, et al. Risk factors for severe pulmonary and disseminated coccidioidomycosis: Kern County, California, 1995-1996. Clin Infect Dis. 2001 Mar 1;32(5):708-15.
- Crum NF, Lederman ER, Stafford CM, Parrish JS, Wallace MR. Coccidioidomycosis: a descriptive survey of a reemerging disease. Clinical characteristics and current controversies. Medicine 2004;83:149-75.
- Woods CW, McRill C, Plikaytis BD, Rosenstein NE, Mosley D, Boyd D, et al. Coccidioidomycosis in human immunodeficiency virus-infected persons in Arizona, 1994-1997: incidence, risk factors, and prevention. J Infect Dis. 2000 Apr;181(4):1428-34.
- Bergstrom L, Yocum DE, Ampel NM, Villanueva I, Lisse J, Gluck O, et al. Increased risk of coccidioidomycosis in patients treated with tumor necrosis factor alpha antagonists. Arthritis and rheumatism. 2004 Jun;50(6):1959-66.
- Blair JE, Logan JL. Coccidioidomycosis in solid organ transplantation. Clin Infect Dis. 2001 Nov 1;33(9):1536-44.
- Bercovitch RS, Catanzaro A, Schwartz BS, Pappagianis D, Watts DH, Ampel NM. Coccidioidomycosis during pregnancy: a review and recommendations for management. Clin Infect Dis. 2011 Aug;53(4):363-8.
- Page last reviewed: January 26, 2017
- Page last updated: May 22, 2017
- Content source:


 ShareCompartir
ShareCompartir