Information for Healthcare Professionals about C. neoformans Infection
Clinical features
Depending on the virulence of the yeast strain and the immune status of the host, C. neoformans can either cause no infection, latent infection, or symptomatic disease. Because C. neoformans enters the body through the respiratory route, infection can present as pneumonia-like illness, with symptoms such as cough, fever, chest pain, and weight loss. C. neoformans can also disseminate to the central nervous system (CNS) and cause meningoencephalitis. Symptoms of a CNS infection may include fever, headache, lethargy, and mental status changes.
Etiologic agent
Cryptococcus neoformans
Reservoir
Worldwide distribution in soil, decaying wood, tree hollows, and bird droppings.
Transmission
C. neoformans infection is acquired through inhalation of basidiospores or desiccated yeast cells from the environment. The infection may be cleared, become latent, cause pulmonary infection, or disseminate to other parts of the body, typically the central nervous system.
Sequelae
C. neoformans meningitis may lead to permanent neurologic damage. Mortality rate varies by geographic location and access to medical care.
Diagnosis
- Culture: The gold standard for diagnosing cryptococcal infection; culture is traditionally identify Cryptococcus from human body samples.
- Microscopy: India Ink can be performed on CSF to quickly visualize Cryptococcus cells under a microscope; however, it can have limited sensitivity. Histopathology for detection of narrow-based budding yeasts in tissue can also be used.
- Antigen detection: Can be used on CSF or serum for detection of early, asymptomatic cryptococcal infection in HIV-infected patients; higher sensitivity than microscopy or culture.
- Latex agglutination (LA)
- Enzyme immunoassay (EIA)
- Lateral flow assay (LFA)
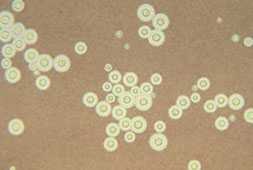
Photomicrograph of Cryptococcus neoformans
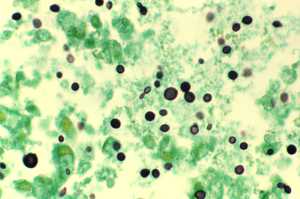
Grocott methenamine silver (GMS) stain showing Cryptococcus in lung tissue
Treatment
Fluconazole is the recommended treatment for asymptomatic or mild-to-moderate pulmonary infections. For severe pulmonary or central nervous system infections, amphotericin B in combination with flucytosine is the preferred initial treatment; after that, patients usually need to take fluconazole for an extended time to clear the infection.
The World Health Organization has also developed guidelines for the diagnosis, prevention, and management of cryptococcal disease in HIV-infected adults, adolescents, and children, with a focus on resource-limited settings.
Risk groups
Immunocompromised persons such those with advanced HIV/AIDS (CD4<100 cells/mm), organ transplant recipients, and persons taking corticosteroids or other immunosuppressive medications.
Surveillance and statistics
In the US, cryptococcosis is reportable in a few states. Check with your local, state, or territorial public health department for more information about disease reporting requirements and procedures in your area. Click here for cryptococcosis statistics.
- Page last reviewed: November 28, 2015
- Page last updated: November 28, 2015
- Content source:


 ShareCompartir
ShareCompartir