C. neoformans Infection Statistics
How common are C. neoformans infections?
C. neoformans infections are extremely rare among people who have healthy immune systems; however, C. neoformans is a major cause of illness in people living with HIV/AIDS, with an estimated 220,000 cases of cryptococcal meningitis occurring worldwide each year.1
C. neoformans infections in the United States
Before antiretroviral therapy was discovered, fungal and other opportunistic infections were a major problem for people with advanced HIV/AIDS. Since then, the numbers of fungal infections and deaths due to fungal infections in people with advanced HIV/AIDS have decreased substantially in the US and other developed countries.2,3 For example, one study showed that the incidence of cryptococcosis in AIDS patients in the US decreased by approximately 90% in the 1990s.2 The decrease in opportunistic infections is primarily because earlier diagnosis of HIV and initiation of antiretroviral therapy (ART) helps keep people with HIV from reaching the stage where their immune systems leave them most vulnerable to fungal infections and other infections.4 However, fungal diseases, particularly cryptococcosis, are still a concern for people living with HIV/AIDS in the US.
Nationally representative estimates for the incidence of cryptococcosis are difficult to establish because cryptococcosis is only reportable in a few states. Results from active, population-based surveillance in two US locations in the year 2000 indicated that the annual incidence of cryptococcosis among persons with AIDS was between 2 and 7 cases per 1,000, and the overall incidence was 0.4 to 1.3 cases per 100,000 population; the case-fatality ratio was approximately 12%.2 More recently, an analysis of stored serum samples from HIV-infected persons with low CD4 counts enrolled in studies in the US during 1986–2012 found the prevalence of cryptococcal antigenemia to be 2.9%, indicating that the prevalence of cryptococcal infection among HIV patients in the US may be high enough to consider targeted screening.5
C. neoformans infections worldwide
Although the widespread availability of antiretroviral therapy (ART) in developed countries has helped improve the immune systems of many HIV patients so that they don’t become vulnerable to infection with Cryptococcus, cryptococcal meningitis is still a major problem in resource-limited countries where HIV prevalence is high and access to healthcare is limited. An estimated 220,000 cases of cryptococcal meningitis occur among people with HIV/AIDS worldwide each year, resulting in nearly 181,000 deaths.1 Most cryptococcal meningitis cases occur in sub-Saharan Africa (Figure 1). Throughout much of sub-Saharan Africa, Cryptococcus is now the most common cause of meningitis in adults. Cryptococcal meningitis is therefore one of the leading causes of death in HIV/AIDS patients in sub-Saharan Africa, where it may kill more people each year than tuberculosis.
Figure 1: global burden of HIV-related cryptococcal meningitis
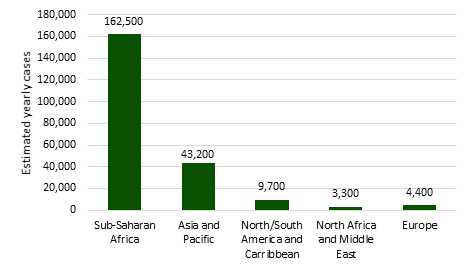
Adapted from R Rajasingham et al., Lancet Infectious Diseases 2017.
References
- Rajasingham R, Smith RM, Park BJ, Jarvis JN, Govender NP, Chiller TM, et al. Global burden of disease of HIV-associated cryptococcal meningitis: an updated analysis. Lancet Infect Dis 2017 May 5.
- Mirza SA, Phelan M, Rimland D, Graviss E, Hamill R, Brandt ME, et al. The changing epidemiology of cryptococcosis: an update from population-based active surveillance in 2 large metropolitan areas, 1992-2000. Clin Infect Dis. 2003 Mar 15;36(6):789-94.
- Kaplan JE, Hanson D, Dworkin MS, Frederick T, Bertolli J, Lindegren ML, et al. Epidemiology of human immunodeficiency virus-associated opportunistic infections in the United States in the era of highly active antiretroviral therapy. Clin Infect Dis. 2000 Apr;30 Suppl 1:S5-14.
- Haddad NE, Powderly WG. The changing face of mycoses in patients with HIV/AIDS. The AIDS reader. 2001 Jul;11(7):365-8, 75-8.
- McKenney J, Smith RM, Chiller TM, Detels R, French A, Margolick J, et al. Prevalence and correlates of cryptococcal antigen positivity among AIDS patients – United States, 1986-2012. MMWR. 2014 Jul 11;63(27):585-7.
- Page last reviewed: November 28, 2015
- Page last updated: July 20, 2017
- Content source:


 ShareCompartir
ShareCompartir