Comorbidity Statistics
What does “comorbidity” mean?
Comorbidity means more than one disease or condition is present in the same person at the same time. Conditions described as comorbidities are often chronic or long-term conditions. Other names to describe comorbid conditions are coexisting or co-occurring conditions and sometimes also “multimorbidity” or “multiple chronic conditions.”
Comorbidities are common among adults with rheumatic diseases like arthritis.1
The CDC Arthritis Program examines comorbidities in two ways:
- Comorbidities among people with arthritis. Everyone in this group has arthritis and at least one other chronic condition.
- Arthritis among people with other chronic conditions. People with other chronic conditions, such as heart disease or diabetes, who also have arthritis.
Arthritis among people with other chronic conditions
In the total US population, 22.7% of adults have arthritis.2 Arthritis is even more common among people with other chronic conditions. In 2013- 2015, the unadjusted prevalence of arthritis among adults had:
- obesity was 31%.
- diabetes was 47%.
- heart disease was 49%.
Figure 1 shows the age-adjusted estimates for obese, diabetes, and heart disease among adults with arthritis. Age-adjusted prevalence estimates were standardized to the projected 2000 US standard population to allow for comparisons between different groups by accounting for variations in age-distribution. After age-adjustment, adults who were obese, had diabetes, or heart disease were approximately 1.5, 1.7, and 1.9 times more likely than those without the corresponding condition to have arthritis, respectively.
Arthritis Prevalence by Chronic Disease Status, NHIS 2013-2015
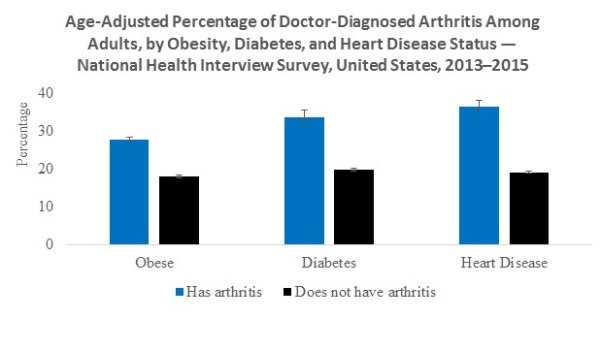
Figure 1. Age-Adjusted Prevalence (95% Confidence Interval) of Doctor-Diagnosed Arthritis Among Adults, by Obesity, Diabetes, and Heart Disease Status
Text Description Available
Data Source: 2013-2015 National Health Interview Survey
Arthritis and heart disease
Arthritis may be a barrier to physical activity among adults with heart disease.3 Being physically active, for example, through aerobic exercise or strength training, can benefit people with arthritis or heart disease and especially those with both conditions.
What are the benefits of increased physical activity for people with heart disease and arthritis?
People with heart disease who are inactive can experience many benefits from becoming more physically active. Benefits of physical activity for people with heart disease can include::
- Lower blood pressure.
- Better physical function.
- Lower low-density lipoprotein cholesterol levels.4,5
Physical inactivity is more common in adults who have both arthritis and heart disease compared with people who only have one or neither condition. Physical inactivity puts people at greater risk for complications from chronic conditions.
Arthritis and diabetes
Arthritis may be a barrier to physical activity among adults with diabetes.6 Being physically active, for example, through aerobic exercise or strength training, can benefit people with arthritis or diabetes and especially those with both conditions.6
What are the benefits of increased physical activity for people with diabetes and arthritis?
People with diabetes who are inactive can experience many benefits from becoming more physically active. Benefits of physical activity for people with diabetes can include:
- Lower blood glucose levels.
- Better weight control.
- Lower blood pressure.
- Improved mood.7
Being physically inactive is an even bigger problem for people with diabetes who also have arthritis. Physical inactivity is more common in adults who have both arthritis and diabetes compared with people who only have one or neither condition. Physical inactivity puts people at greater risk for complications from chronic conditions.
Arthritis and obesity
Arthritis may be a barrier to physical activity among adults who are obese.8 Being physically active, for example, through aerobic exercise or strength training, can benefit people with arthritis or obesity and especially those with both conditions.
What are the benefits of increased physical activity for people who are obese?
People who are obese and physically inactive can experience many benefits from becoming more physically active. Benefits of physical activity for obese people include:
- Better weight control.
- Reduce your risk of diabetes, heart disease, and other comorbidities.
- Improved mood.
- Strengthen muscles and bones.9
Physical inactivity is more common in adults who have both arthritis and obesity compared with people who only have one or neither condition. Physical inactivity puts people at greater risk for complications from chronic conditions.
What can people who have arthritis and comorbidities do?
The CDC Arthritis Program recommends self-management education programs and physical activity programs for all people with arthritis. These programs teach people skills to take charge of their conditions and engage in effective, joint-friendly physical activity. These programs also have proven benefits for other chronic conditions. For information on about these programs, visit the CDC Arthritis Program’s Intervention Programs page.
Public Health Chronic Disease Management Strategies
Self-management education programs are a proven approach
Comorbidities can complicate disease management and treatment. Fortunately, there are evidence-based strategies that address the effects of arthritis and other chronic diseases. These strategies help individuals and health professionals with comprehensive disease management.
Health care providers can also help improve patients’ quality-of-life by referring them to chronic disease self-management education programs that address the effects of arthritis and other chronic conditions.
Learn about CDC recommended intervention programs that are proven to improve the quality of life of people with arthritis.
Keeping people with arthritis and comorbidities physically active
Being physically active is an essential part of preventing and managing many chronic conditions, including arthritis, heart disease, diabetes, and obesity. However, most adults face the following common barriers to physical activity:
- Lack of time.
- Competing responsibilities.
- Lack of motivation.
- Difficulty finding an enjoyable activity.
Adults with arthritis may face the following additional, disease-specific barriers:
- Concerns about aggravating arthritis pain.
- Fear about causing further joint damage.
- Uncertainty about which types and amounts of activity are safe for their joints.
Health care providers can help people overcome arthritis-specific barriers to physical activity by providing appropriate advice and referrals to evidence-based physical activity programs that are designed for adults with arthritis. Learn more about the importance of physical activity for people with arthritis.
Learn about intervention programs, such as self-management education programs and physical activity programs, that are designed to teach people the skills they need to take charge of their conditions and engage in effective, joint-friendly physical activity.
Related Links
References
1. Theis KA, Brady TJ, Helmick CG. No One Dies of Old Age Anymore: A Coordinated Approach to Comorbidities and the Rheumatic Diseases. Arthritis Care Res (Hoboken). 2017;69(1):1-4. DOI: 10.1002/acr.23114
2. Barbour KE, Helmick CG, Boring MA, Brady TJ. Prevalence of Doctor-Diagnosed Arthritis and Arthritis-Attributable Activity Limitation — United States, 2013—2015. Morb Mortal Wkly Rep. 2017 March 7. [Epub ahead of print].
3. Bolen J, Murphy L, Greenlund K, Helmick CG, Hootman J, Brady TJ, et al. Arthritis as a potential barrier to physical activity among adults with heart disease — United States, 2005 and 2007. Morb Mortal Wkly Rep. 2009;58(7):165–169. html; pdf [1.25MB].
4. U.S. Department of Health and Human Services. 2008 physical activity guidelines for Americans. Hyattsville, MD: U.S. Department of Health and Human Services; 2008. Available at http://www.health.gov/paguidelines.
5. Smith SC Jr, Allen J, Blair SN, et al. AHA/ACC guidelines for secondary prevention for patients with coronary and other atherosclerotic vascular disease: 2006 update. Circulation. 2006;113:23:63–72. Free access html pdf [611KB]
6. Bolen J, Hootman J, Helmick CG, Murphy L, Langmaid G, Caspersen CJ. Arthritis as a Potential Barrier to Physical Activity Among Adults with Diabetes — United States, 2005 and 2007. Morb Mortal Wkly Rep. 2008;57(18):486–489. html; pdf [1.25MB]
7. Diabetes Diet, Eating, and Physical Activity Webpage. National Institute of Diabetes and Digestive and Kidney Diseases website. https://www.niddk.nih.gov/health-information/diabetes/overview/diet-eating-physical-activity. Accessed February 2, 2017.
8. Hootman JM, Murphy LB, Helmick CG, Barbour KE. Arthritis as a potential barrier to physical activity among adults with obesity—United States, 2007 and 2009. Morb Mortal Wkly Rep. 2011;60(19):614-618. PubMed PMID: 21597454. abstract
9. Physical Activity and Health Webpage. Centers for Disease Control and Prevention website. https://www.cdc.gov/physicalactivity/basics/pa-health/index.htm. Accessed February 2, 2017.
- Page last reviewed: March 6, 2017
- Page last updated: June 8, 2017
- Content source:
- Maintained By:


 ShareCompartir
ShareCompartir