Superior laryngeal nerve
The superior laryngeal nerve is a branch of the vagus nerve. It arises from the middle of the inferior ganglion of vagus nerve and in its course receives a branch from the superior cervical ganglion of the sympathetic nervous system.
| Superior laryngeal nerve | |
|---|---|
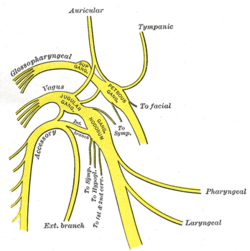 Plan of upper portions of glossopharyngeal, vagus, and accessory nerves. ("Laryngeal" labeled at lower right.) | |
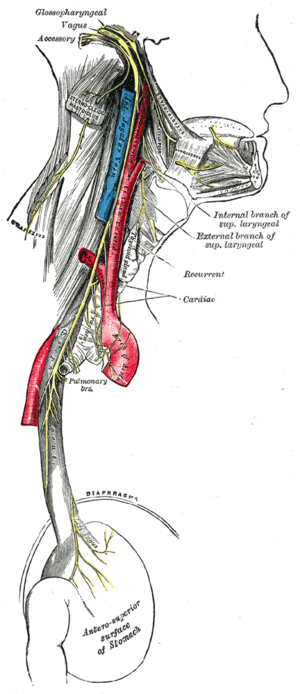 Course and distribution of the glossopharyngeal, vagus, and accessory nerves. (Branches visible in upper right.) | |
| Details | |
| From | Vagus nerve |
| Innervates | larynx |
| Identifiers | |
| Latin | nervus laryngeus superior |
| TA | A14.2.01.160 |
| FMA | 6239 |
| Anatomical terms of neuroanatomy | |
The cricothyroid muscles are innervated by the superior laryngeal nerve. All other intrinsic laryngeal muscles are innervated by the recurrent laryngeal nerve.
The superior laryngeal nerve consists of two branches: the internal laryngeal nerve (sensory), which supplies sensory fibers to the laryngeal mucosa, and the external laryngeal nerve (motor), which innervates the cricothyroid muscle.
The recurrent laryngeal nerve gets its name from the fact that it loops below the aorta on its way to the intrinsic muscles of the larynx. The left recurrent laryngeal nerve passes under and around the aorta on its way to the larynx, whereas the right recurrent laryngeal nerve passes under and around the subclavian artery. Because the aorta is inferior to the subclavian artery, the left recurrent laryngeal nerve is a bit longer than the right recurrent laryngeal nerve. However, there is no discernible effect on the timing of neural impulses to the muscles these two nerves serve. By comparison with the recurrent laryngeal nerves, the superior laryngeal nerve takes a more direct route on the way to the cricothyroid muscles.[1]
Structure
The superior laryngeal nerve descends, by the side of the pharynx, behind the internal carotid artery, and divides into two branches —the external laryngeal nerve and the internal laryngeal nerve.
The external laryngeal nerve is the smaller, external branch. It descends on the larynx, beneath the sternothyroid muscle, to supply the cricothyroid muscle. The external branch functions to tense the vocal cords by activating the cricothyroid muscle, increasing pitch. The external laryngeal nerve gives branches to pharyngeal plexus and the superior portion of the inferior pharyngeal constrictor, and communicates with the superior cardiac nerve behind the common carotid artery.
The internal laryngeal nerve is the internal branch. It descends to the thyrohyoid membrane, piercing it in company with the superior laryngeal artery, and is distributed to the mucous membrane of the larynx. Of these sensory branches, some are distributed to the epiglottis, the base of the tongue, and the epiglottic glands; others pass posteriorly, in the aryepiglottic fold, to supply the mucous membrane surrounding the entrance of the larynx, and the mucous lining of the larynx as far down as the vocal folds.
A filament descends beneath the mucous membrane on the inner surface of the thyroid cartilage and joins the recurrent nerve. Above the vocal folds the sensory innervation of the larynx is via the internal laryngeal nerve. Below the vocal folds it is by way of branches of the recurrent laryngeal nerve. The vocal fold itself receives dual innervation from both nerves.
Clinical significance
A superior laryngeal nerve palsy changes the pitch of the voice and causes an inability to make explosive sounds due to paralysis of the cricothyroid muscle. If no recovery is evident three months after the palsy initially presents, the damage is most likely to be permanent. A bilateral palsy presents as a tiring and hoarse voice. Damage to the superior laryngeal nerve leaves the vocal cord abducted and poses an aspiration risk. It can be injured in surgery involving the removal of the thyroid gland (thyroidectomy).[2][3] Understanding the most common anatomic variations of the distal portion of the external laryngeal nerve and its relation to the inferior constrictor muscle is critical and allows identifying and preserving the integrity of this nerve in most cases.[4][5] The external branch is susceptible to damage during thyroidectomy or cricothyrotomy, as it lies immediately deep to the superior thyroid artery. The ability to produce pitched sounds is then impaired along with easy voice fatigability, (usually mono-toned voice).
Irritation of the internal laryngeal nerve results in uncontrolled coughing - usually as a result of food or water in the laryngopharynx. The lesion of this branch (for example, during surgery) that seeks an anterior approach to the cervix, is associated with a loss of the laryngeal reflex of cough and an elevate risk of aspiration pneumonia.[6]
Additional images
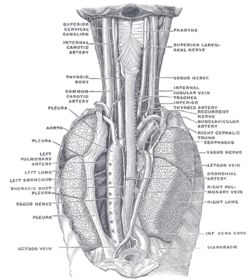 The position and relation of the esophagus in the cervical region and in the posterior mediastinum. Seen from behind.
The position and relation of the esophagus in the cervical region and in the posterior mediastinum. Seen from behind.
References
- Fuller, D. R., Pimentel, J. T., & Peregoy, B. M. (2012). Applied anatomy & physiology for speech-language pathology & audiology. Baltimore, MD: Wolters Kluwer- Lippincott Williams & Wilkins.
- Jansson S, Tisell LE, Hagne I, Sanner E, Stenborg R, Svensson P (1988). "Partial superior laryngeal nerve (SLN) lesions before and after thyroid surgery". World J Surg. 12 (4): 522–7. PMID 3420935.
- Barczyński M, Randolph GW, Cernea CR, Dralle H, Dionigi G, Alesina PF, Mihai R, Finck C, Lombardi D, Hartl DM, Miyauchi A, Serpell J, Snyder S, Volpi E, Woodson G, Kraimps JL, Hisham AN (2013). "External branch of the superior laryngeal nerve monitoring during thyroid and parathyroid surgery: International Neural Monitoring Study Group standards guideline statement". Laryngoscope. 123 Suppl 4: S1–14. doi:10.1002/lary.24301. PMID 23832799.
- Friedman M, LoSavio P, Ibrahim H (2002). "Superior laryngeal nerve identification and preservation in thyroidectomy". Arch. Otolaryngol. Head Neck Surg. 128 (3): 296–303. PMID 11886347.
- Potenza AS, Araujo Filho VJ, Cernea CR (2017). "Injury of the external branch of the superior laryngeal nerve in thyroid surgery". Gland Surg. 6 (5): 552–562. doi:10.21037/gs.2017.06.15. PMC 5676167. PMID 29142848.
- Kiray A, Naderi S, Ergur I, Korman E (2006). "Surgical anatomy of the internal branch of the superior laryngeal nerve". Eur Spine J. 15 (9): 1320–5. doi:10.1007/s00586-005-0006-7. PMC 2438561. PMID 16402208.
This article incorporates text in the public domain from page 912 of the 20th edition of Gray's Anatomy (1918)
Fuller, D. R., Pimentel, J. T., & Peregoy, B. M. (2012). Applied anatomy & physiology for speech-language pathology & audiology. Baltimore, MD: Wolters Kluwer- Lippincott Williams & Wilkins.
External links
- cranialnerves at The Anatomy Lesson by Wesley Norman (Georgetown University) (X)