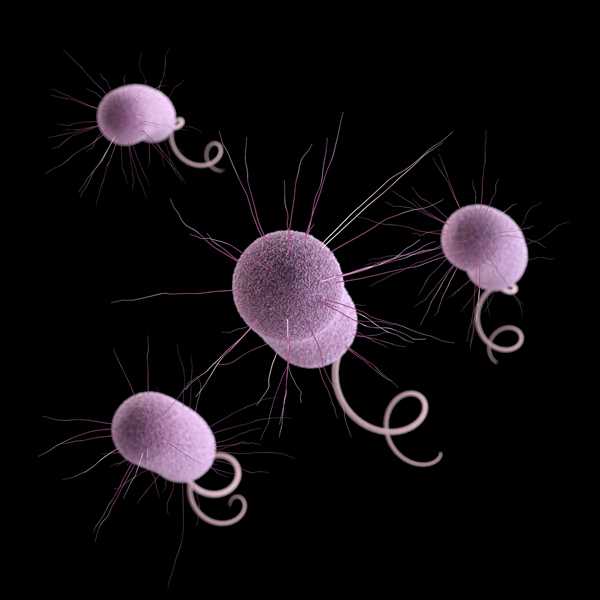
Superbugs threaten hospital patients
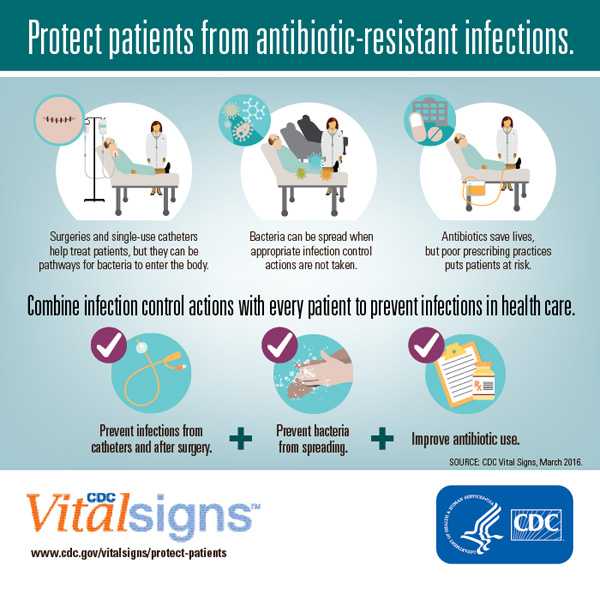
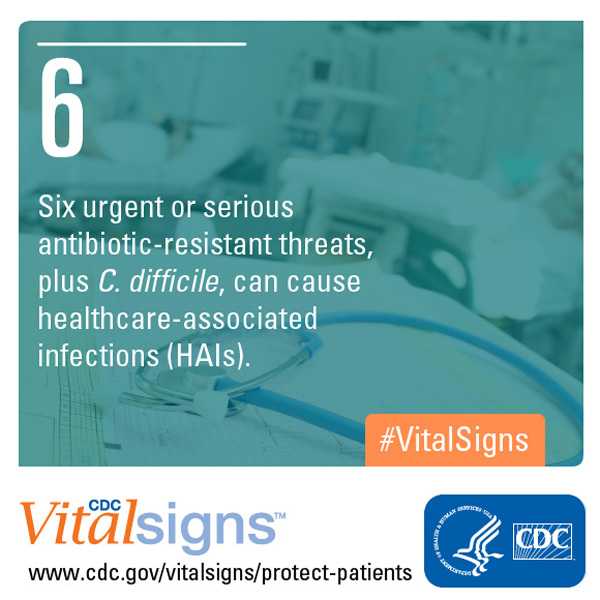
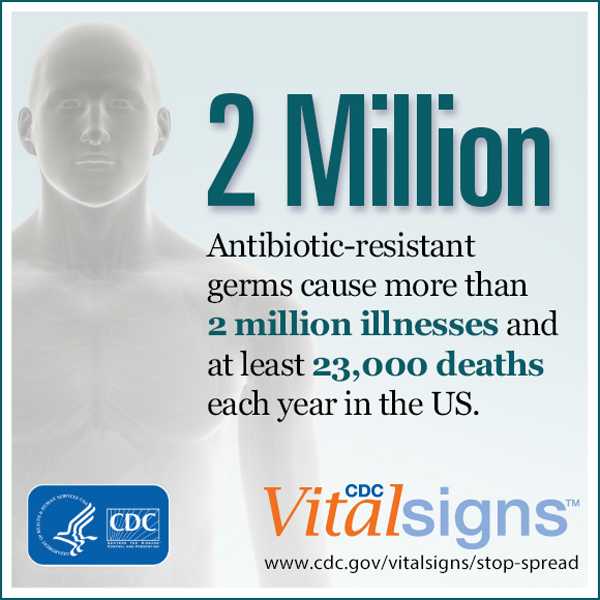
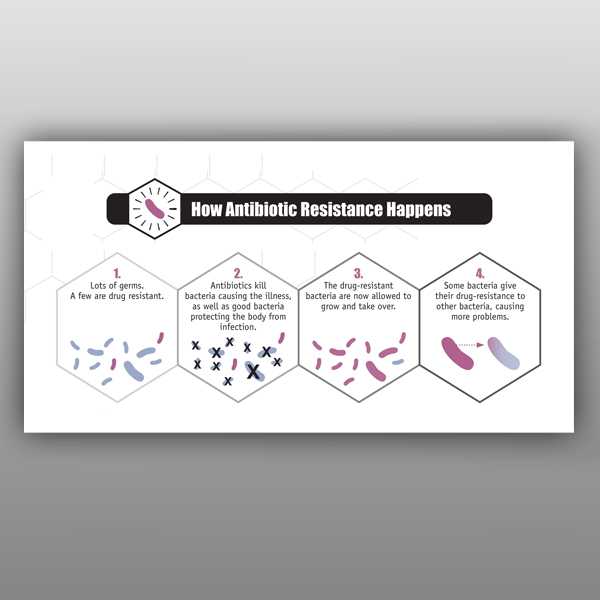
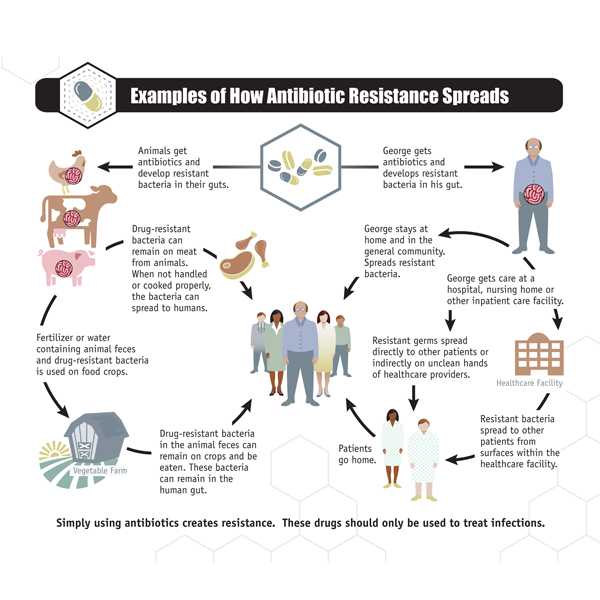
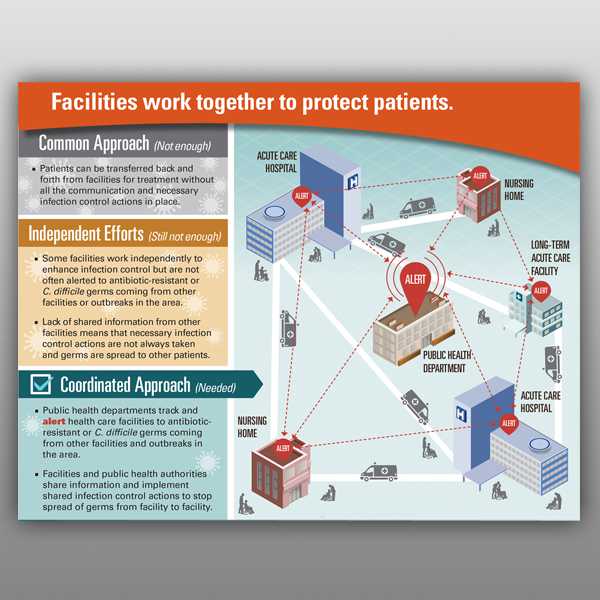
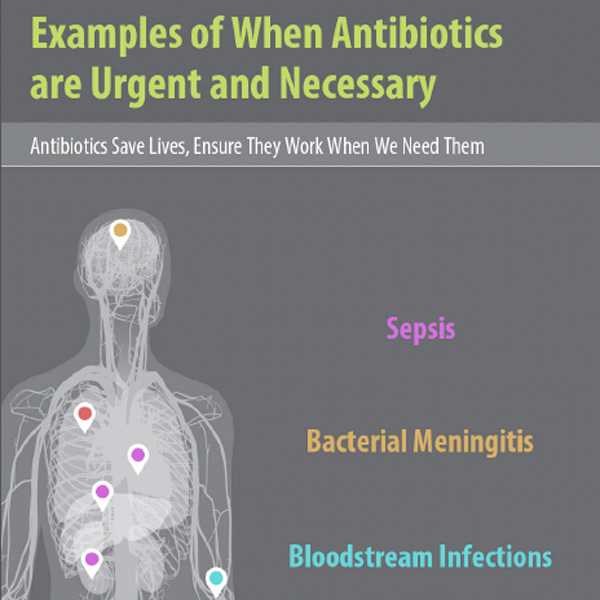
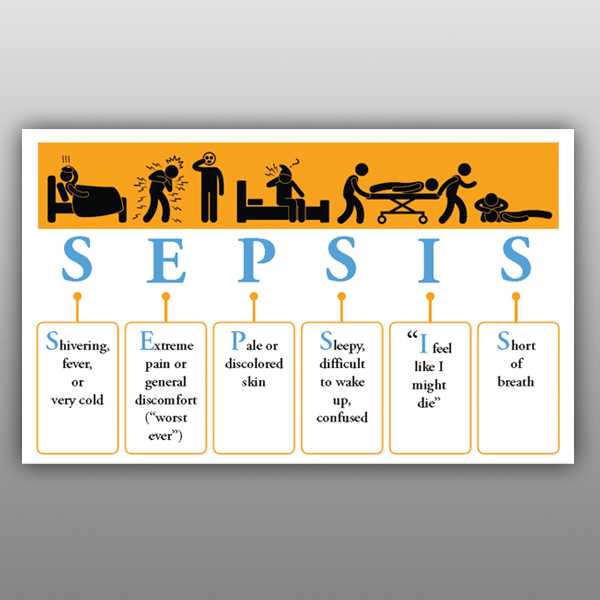
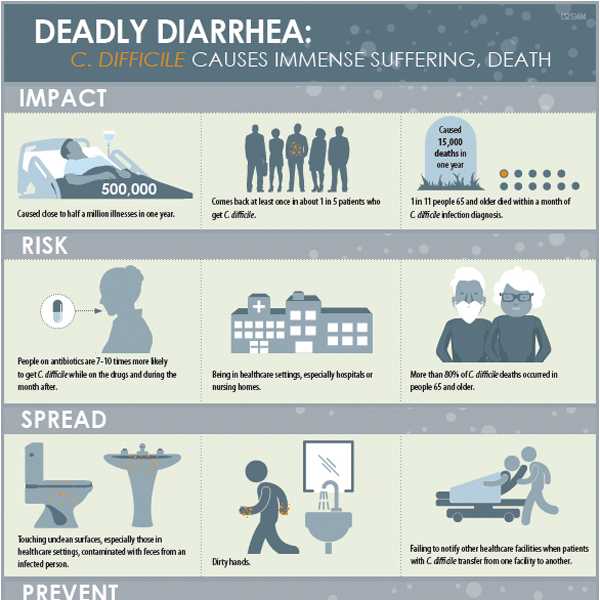
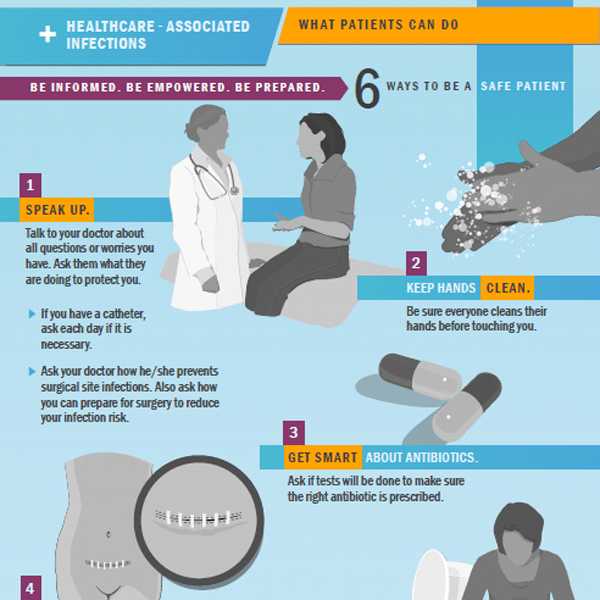
CDC’s latest Vital Signs report urges healthcare workers to use a combination of infection control recommendations to better protect patients from healthcare-associated infections (HAIs) and antibiotic resistance. Many of the most urgent and serious antibiotic-resistant bacteria CDC warned of in the 2013 Antibiotic Resistant Threat Report often threaten patients while they are being treated in healthcare facilities for other conditions. To turn the tide against other complications, such as sepsis, we must prevent healthcare-associated infections (HAIs) in the first place and prevent resistant bacteria from spreading.
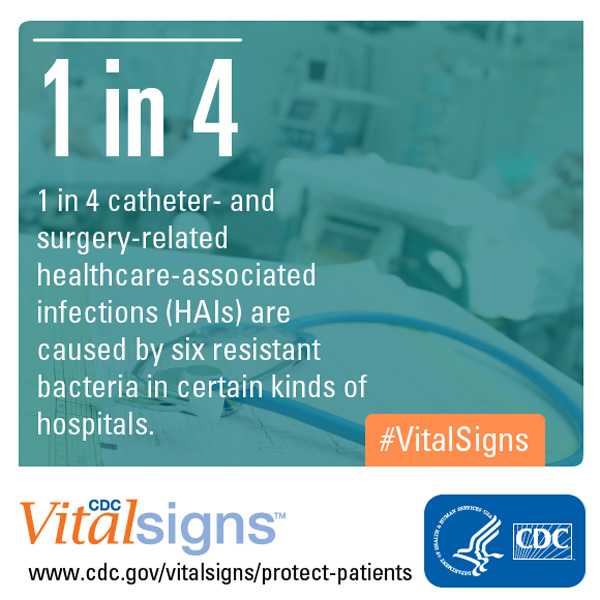
In acute care hospitals, 1 in 7 catheter- and surgery-related HAIs can be caused by any of six antibiotic-resistant bacteria, including methicillin-resistant Staphylococcus aureus (MRSA) and “nightmare bacteria” carbapenem-resistant Enterobacteriaceae (CRE). That number increases to 1 in 4 infections in long-term acute care hospitals, which treat patients who are generally very sick and stay, on average, more than 25 days.
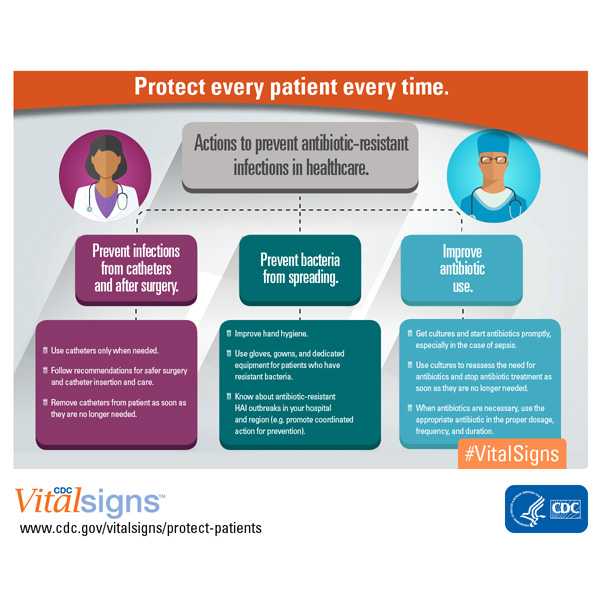
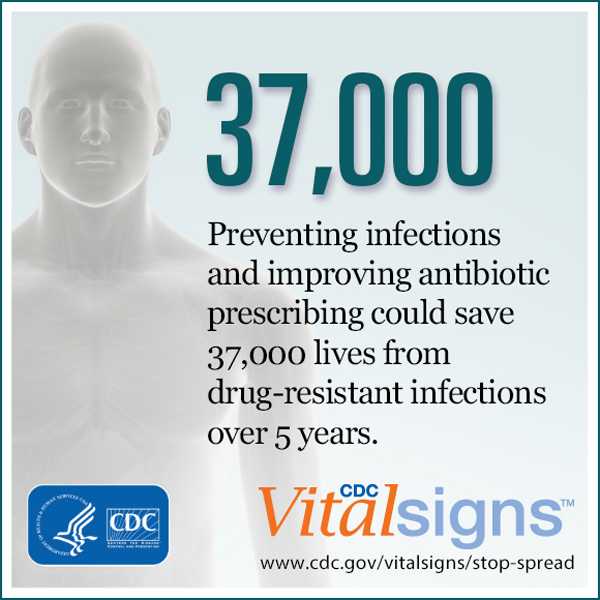
CDC is calling on everyone to continue to do their part to prevent HAIs. The report recommends doctors and nurses combine three critical efforts to accomplish this:
- Prevent the spread of bacteria between patients;
- Prevent infections related to surgery and/or placement of a catheter; and
- Improve antibiotic use through stewardship.
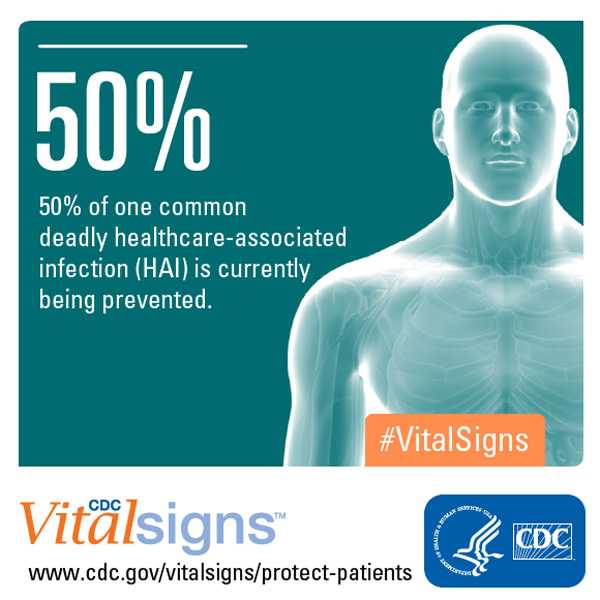
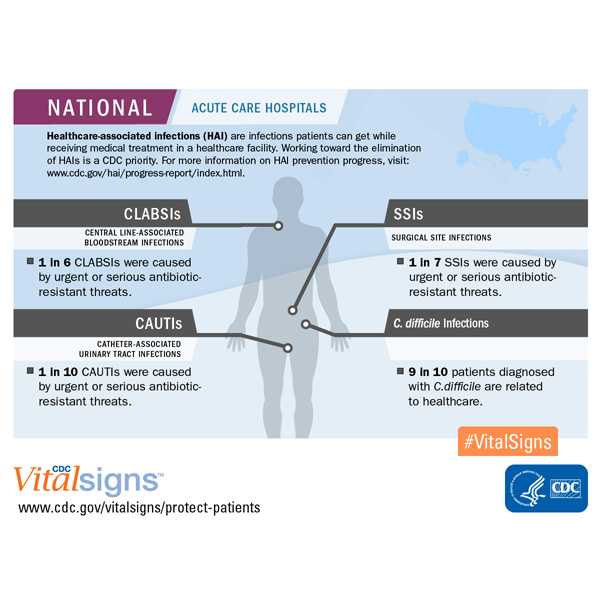
Progress has been made in preventing HAIs, but more work is needed – especially in fighting antibiotic-resistant bacteria. The Vital Signs report, along with national data from CDC’s latest annual progress report on HAI prevention, show that acute care hospitals have achieved:
- A 50 percent decrease in central line-associated bloodstream infections (CLABSIs) between 2008 and 2014.
- 1 in 6 remaining CLABSIs are caused by urgent or serious antibiotic-resistant bacteria.
- A 17 percent decrease in surgical site infections (SSIs) between 2008 and 2014 related to 10 procedures tracked in previous HAI progress reports.
- 1 in 7 remaining SSIs are caused by urgent or serious antibiotic-resistant bacteria.
- No change in the overall catheter-associated urinary tract infections (CAUTIs) between 2009 and 2014. During this time however, there was progress in non-ICU settings, progress in all settings between 2013 and 2014, and most notably, even more progress in all settings towards the end of 2014.
- 1 in 10 CAUTIs are caused by urgent or serious antibiotic-resistant bacteria.
For the first time, CDC released a new web app with interactive data on HAIs caused by antibiotic-resistant bacteria, Antibiotic Resistance Patient Safety Atlas. The tool provides national, regional, and state map views of superbug/drug combinations showing percent resistance over time. The Atlas uses data reported to CDC’s National Healthcare Safety Network from 2011 to 2014 from more than 4,000 healthcare facilities.
Congress has recognized the urgent need to combat antibiotic resistance. In fiscal year 2016, Congress appropriated $160 million in new funding for CDC to implement its activities listed in the National Action Plan for Combating Antibiotic-resistant Bacteria. With this funding, CDC will fight the spread of antibiotic resistance by:
- accelerating outbreak detection and prevention in every state;
- enhancing tracking of resistance mechanisms and resistant infections;
- supporting innovative research to address current gaps in knowledge; and
- improving antibiotic use.
Visit the full press release for more details.
Contact Information
CDC Media Relations
(404) 639-3286
media@cdc.gov
Vital Signs Links
Factsheet:
English [1.98MB]
Spanish [3.04MB]
Spokespersons
Clifford McDonald, MD
“For clinicians, prevention means isolating patients when necessary. It also means being aware of antibiotic resistance patterns in your facilities, following recommendations for preventing infections that can occur after surgery or from central lines and catheters placed in the body, and prescribing antibiotics correctly.”
Clifford McDonald, MD – Associate Director for Science, CDC Division of Healthcare Quality Promotion
Arjun Srinivasan, MD
“We don’t want untreatable infections to become common. Some concrete plans to combat this include obtaining real-time data about antibiotic use and trends to better understand prescribing practices and using CDC’s National Healthcare Safety Network (NHSN) in hospitals. We are also working with partners to set national goals for improving antibiotic use and reducing resistance across all healthcare settings to improve antibiotic prescribing.”
Arjun Srinivasan, MD – Associate Director for Healthcare-Associated Infection Prevention Programs, Division of Healthcare Quality Promotion
Related Links
- Press Release: Superbugs threaten hospital patients – English | Spanish
- MMWR – Vital Signs: Preventing Antibiotic-Resistant Infections in Hospitals — United States, 2014 | PDF [1.25MB]
- Vital Signs: Home | March 2016 Vital Signs | Fact Sheet PDF[1.98MB] | Topics
- Vital Signs (Spanish): Home | March 2016 Vital Signs | Fact Sheet PDF [3.04MB] | Topics
- Antibiotic Resistance Patient Safety Atlas
- National and State Healthcare-Associated Infections Progress Report
- CDC’s Safe Healthcare Blog
- CDC Healthcare-associated Infections Website
- CDC Drug Resistance Website
- Biggest Antibiotic Resistance Threats
- CDC Clostridium difficile Infection Website
- CDC Sepsis Website
- CDC MRSA Website
- CDC CRE Website
- National Healthcare Safety Network
- Core Elements of Hospital Antibiotic Stewardship Programs
- Get Smart: Know When Antibiotics Work
Video
- Healthcare-Associated Infections in the United States (2014)
- Get Smart About Antibiotics: For Healthcare Professionals
- CDC Vital Signs (2015): Stop the Spread of Antibiotic Resistance (Short)
- 5 Tips for Patients
- Get Smart About Antibiotics: For Patients and Parents
- CDC Urges Sepsis Awareness
Podcast
- Making Health Care Safer English | Spanish
- Making Health Care Safer [PSA – 0:60 seconds]
- Vital Signs (2015) – Communication Can Save Lives
- Vital Signs (2014) – Antibiotic RX in Hospitals: Proceed with Caution
- Signos Vitales de los CDC (2014) – Antibióticos recetados en los hospitales: Tenga cuidado
- Snort, sniffle, sneeze: No Antibiotics Please (2009)
- Page last reviewed: March 3, 2016
- Page last updated: March 3, 2016
- Content source:



 ShareCompartir
ShareCompartir