Spinal muscular atrophy
Spinal muscular atrophy (SMA) is a group of neuromuscular disorders that result in the loss of motor neurons and progressive muscle wasting.[1] The severity of symptoms and age of onset varies by the type.[1] Some types are apparent at or before birth while others are not apparent until adulthood.[1] All generally result in worsening muscle weakness associated with muscle twitching.[1][3] Arm, leg and respiratory muscles are generally affected first.[3][4] Associated problems may include problems with swallowing, scoliosis, and joint contractures.[2][4] SMA is a leading genetic cause of death in infants.[5]
| Spinal muscular atrophy | |
|---|---|
| Other names | Autosomal recessive proximal spinal muscular atrophy, 5q spinal muscular atrophy |
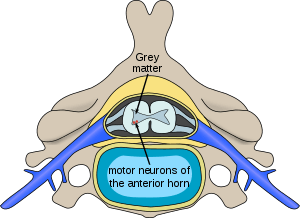 | |
| Location of neurons affected by spinal muscular atrophy in the spinal cord | |
| Specialty | Neurology |
| Symptoms | Progressive muscle weakness[1] |
| Complications | Scoliosis, joint contractures, pneumonia[2] |
| Types | Type 0 to type 4[2] |
| Causes | Mutation in SMN1[2] |
| Diagnostic method | Genetic testing[1] |
| Differential diagnosis | Congenital muscular dystrophy, Duchenne muscular dystrophy, Prader-Willi syndrome[2] |
| Treatment | Supportive care, medications[1] |
| Medication | Nusinersen, onasemnogene abeparvovec |
| Prognosis | Varies by type[2] |
| Frequency | 1 in 10,000 people[2] |
Spinal muscular atrophy is due to a genetic defect in the SMN1 gene.[1][2] They are inherited from a person's parents in an autosomal recessive manner.[1] The SMN1 gene encodes SMN, a protein necessary for survival of motor neurons.[4] Loss of these neurons prevents the sending of signals between the brain and skeletal muscles.[4] Diagnosis is suspected based on symptoms and confirmed by genetic testing.[1]
Treatments include supportive care such as physical therapy, nutrition support, and mechanical ventilation.[1] The medication nusinersen, which is injected around the spinal cord, slows the progression of the disease and improves muscle function.[1][3] In 2019, the gene therapy onasemnogene abeparvovec was approved in the US as a treatment for children under 24 months.[5] Outcomes vary by type from a life expectancy of a few months to mild muscle weakness with a normal life expectancy.[4] The condition affects about 1 in 10,000 people at birth.[2]
Classification
SMA manifests over a wide range of severity, affecting infants through adults. The disease spectrum is variously divided into 3–5 types, in accordance either with the age of onset of symptoms or with the highest attained milestone of motor development.
The most commonly used classification is as follows:
| Type | Eponym | Usual age of onset | Characteristics | OMIM |
|---|---|---|---|---|
| SMA1 (Infantile) |
Werdnig–Hoffmann disease | 0–6 months | The severe form manifests in the first months of life, usually with a quick and unexpected onset ("floppy baby syndrome"). Rapid motor neuron death causes inefficiency of the major bodily organs – especially of the respiratory system – and pneumonia-induced respiratory failure is the most frequent cause of death. Unless placed on mechanical ventilation, babies diagnosed with SMA type 1 do not generally live past two years of age, with death occurring as early as within weeks in the most severe cases (sometimes termed SMA type 0). With proper respiratory support, those with milder SMA type I phenotypes, which account for around 10% of SMA1 cases, are known to live into adolescence and adulthood. | 253300 |
| SMA2 (Intermediate) |
Dubowitz disease | 6–18 months | The intermediate form affects children who are never able to stand and walk but who are able to maintain a sitting position at least some time in their life. The onset of weakness is usually noticed some time between 6 and 18 months. The progress is known to vary greatly, some people gradually grow weaker over time while others through careful maintenance avoid any progression. Scoliosis may be present in these children, and correction with a brace may help improve respiration. Body muscles are weakened, and the respiratory system is a major concern. Life expectancy is reduced but most people with SMA2 live well into adulthood. | 253550 |
| SMA3 (Juvenile) |
Kugelberg–Welander disease | >12 months | The juvenile form usually manifests after 12 months of age and describes people with SMA3 who are able to walk without support at some time, although many later lose this ability. Respiratory involvement is less noticeable, and life expectancy is normal or near normal. | 253400 |
| SMA4 (Adult-onset) |
Adulthood | The adult-onset form (sometimes classified as a late-onset SMA type 3) usually manifests after the third decade of life with gradual weakening of muscles – mainly affects proximal muscles of the extremities – frequently requiring the person to use a wheelchair for mobility. Other complications are rare, and life expectancy is unaffected. | 271150 |
The most severe form of SMA type I is sometimes termed SMA type 0 (or, severe infantile SMA) and is diagnosed in babies that are born so weak that they can survive only a few weeks even with intensive respiratory support. SMA type 0 should not be confused with SMARD1 which may have very similar symptoms and course but has a different genetic cause than SMA.
Motor development in people with SMA is usually assessed using validated functional scales – CHOP INTEND (The Children's Hospital of Philadelphia Infant Test of Neuromuscular Disorders) in SMA1; and either the Motor Function Measure scale or one of a few variants of Hammersmith Functional Motor Scale[6][7][8][9] in SMA types 2 and 3.
The eponymous label Werdnig–Hoffmann disease (sometimes misspelled with a single n) refers to the earliest clinical descriptions of childhood SMA by Johann Hoffmann and Guido Werdnig. The eponymous term Kugelberg–Welander disease is after Erik Klas Hendrik Kugelberg (1913–1983) and Lisa Welander (1909–2001), who distinguished SMA from muscular dystrophy.[10] Rarely used Dubowitz disease (not to be confused with Dubowitz syndrome) is named after Victor Dubowitz, an English neurologist who authored several studies on the intermediate SMA phenotype.
Signs and symptoms

The symptoms vary depending on the SMA type, the stage of the disease as well as individual factors. Signs and symptoms below are most common in the severe SMA type 0/I:[11]
- Areflexia, particularly in extremities
- Overall muscle weakness, poor muscle tone, limpness or a tendency to flop
- Difficulty achieving developmental milestones, difficulty sitting/standing/walking
- In small children: adopting of a frog-leg position when sitting (hips abducted and knees flexed)
- Loss of strength of the respiratory muscles: weak cough, weak cry (infants), accumulation of secretions in the lungs or throat, respiratory distress
- Bell-shaped torso (caused by using only abdominal muscles for respiration) in severe SMA type
- Fasciculations (twitching) of the tongue
- Difficulty sucking or swallowing, poor feeding
Causes
Spinal muscular atrophy is linked to a genetic mutation in the SMN1 gene.[12]
Human chromosome 5 contains two nearly identical genes at location 5q13: a telomeric copy SMN1 and a centromeric copy SMN2. In healthy individuals, the SMN1 gene codes the survival of motor neuron protein (SMN) which, as its name says, plays a crucial role in survival of motor neurons. The SMN2 gene, on the other hand – due to a variation in a single nucleotide (840.C→T) – undergoes alternative splicing at the junction of intron 6 to exon 8, with only 10–20% of SMN2 transcripts coding a fully functional survival of motor neuron protein (SMN-fl) and 80–90% of transcripts resulting in a truncated protein compound (SMNΔ7) which is rapidly degraded in the cell.[13]
In individuals affected by SMA, the SMN1 gene is mutated in such a way that it is unable to correctly code the SMN protein – due to either a deletion[14] occurring at exon 7[15] or to other point mutations (frequently resulting in the functional conversion of the SMN1 sequence into SMN2). Almost all people, however, have at least one functional copy of the SMN2 gene (with most having 2–4 of them) which still codes small amounts of SMN protein – around 10–20% of the normal level – allowing some neurons to survive. In the long run, however, reduced availability of the SMN protein results in gradual death of motor neuron cells in the anterior horn of spinal cord and the brain. Muscles that depend on these motor neurons for neural input now have decreased innervation (also called denervation), and therefore have decreased input from the central nervous system (CNS). Decreased impulse transmission through the motor neurons leads to decreased contractile activity of the denervated muscle. Consequently, denervated muscles undergo progressive atrophy (waste away).
Muscles of lower extremities are usually affected first, followed by muscles of upper extremities, spine and neck and, in more severe cases, pulmonary and mastication muscles. Proximal muscles are always affected earlier and to a greater degree than distal.[16]
The severity of SMA symptoms is broadly related to how well the remaining SMN2 genes can make up for the loss of function of SMN1. This is partly related to the number of SMN2 gene copies present on the chromosome. Whilst healthy individuals carry two SMN2 gene copies, people with SMA can have anything between 1 and 4 (or more) of them, with the greater the number of SMN2 copies, the milder the disease severity. Thus, most SMA type I babies have one or two SMN2 copies; people with SMA II and III usually have at least three SMN2 copies; and people with SMA IV normally have at least four of them. However, the correlation between symptom severity and SMN2 copy number is not absolute, and there seem to exist other factors affecting the disease phenotype.[17]
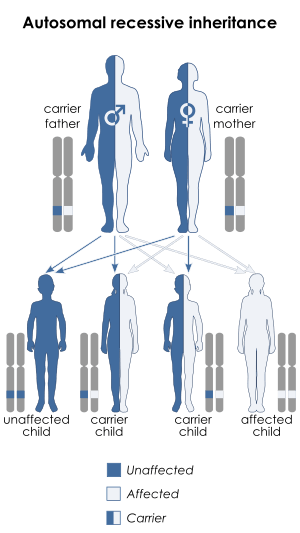
Spinal muscular atrophy is inherited in an autosomal recessive pattern, which means that the defective gene is located on an autosome. Two copies of the defective gene – one from each parent – are required to inherit the disorder: the parents may be carriers and not personally affected. SMA seems to appear de novo (i.e., without any hereditary causes) in around 2–4% of cases.
Spinal muscular atrophy affects individuals of all ethnic groups, unlike other well known autosomal recessive disorders, such as sickle cell disease and cystic fibrosis, which have significant differences in occurrence rate among ethnic groups. The overall prevalence of SMA, of all types and across all ethnic groups, is in the range of 1 per 10,000 individuals; the gene frequency is around 1:100, therefore, approximately one in 50 persons are carriers.[18][19] There are no known health consequences of being a carrier. A person may learn carrier status only if one's child is affected by SMA or by having the SMN1 gene sequenced.
Affected siblings usually have a very similar form of SMA. However, occurrences of different SMA types among siblings do exist – while rare, these cases might be due to additional de novo deletions of the SMN gene, not involving the NAIP gene, or the differences in SMN2 copy numbers.
Diagnosis
The most severe manifestation on the SMA spectrum can be noticeable to mothers late in their pregnancy by reduced or absent fetal movements. Symptoms are critical (including respiratory distress and poor feeding) which usually result in death within weeks, in contrast to the mildest phenotype of SMA (adult-onset), where muscle weakness may present after decades and progress to the use of a wheelchair but life expectancy is unchanged.[20]
The more common clinical manifestations of the SMA spectrum that prompt diagnostic genetic testing:
- Progressive bilateral muscle weakness (Usually upper arms & legs more so than hands and feet) preceded by an asymptomatic period (all but most severe type 0)[20]
- Flattening of the chest wall when taking a breath and belly protrusion when taking a breath in.
- hypotonia associated with absent reflexes.
While the above symptoms point towards SMA, the diagnosis can only be confirmed with absolute certainty through genetic testing for bi-allelic deletion of exon 7 of the SMN1 gene which is the cause in over 95% of cases.[11] Genetic testing is usually carried out using a blood sample, and MLPA is one of more frequently used genetic testing techniques, as it also allows establishing the number of SMN2 gene copies.[11]
Preimplantation testing
Preimplantation genetic diagnosis can be used to screen for SMA-affected embryos during in-vitro fertilisation.
Prenatal testing
Prenatal testing for SMA is possible through chorionic villus sampling, cell-free fetal DNA analysis and other methods.
Carrier testing
Those at risk of being carriers of SMN1 deletion, and thus at risk of having offspring affected by SMA, can undergo carrier analysis using a blood or saliva sample. The American College of Obstetricians and Gynecologists recommends all people thinking of becoming pregnant be tested to see if they are a carrier.[21]
However, genetic testing will not be able to identify all individuals at risk since about 2% of cases are caused by de novo mutations and 5% of the normal populations have two copies of SMN1 on the same chromosome, which makes it possible to be a carrier by having one chromosome with two copies and a second chromosome with zero copies. This situation will lead to a false negative result, as the carrier status will not be correctly detected by a traditional genetic test.[22] [23]
Routine screening
Routine prenatal or neonatal screening for SMA is controversial, because of the cost, and because of the severity of the disease. Some researchers have concluded that population screening for SMA is not cost-effective, at a cost of $5 million per case averted in the United States as of 2009.[24] Others conclude that SMA meets the criteria for screening programs and relevant testing should be offered to all couples.[25] The major argument for neonatal screening is that in SMA type I, there is a critical time period in which to initiate therapies to reduce loss of muscle function and proactive treatment in regards to nutrition.[11]
Management
The management of SMA varies based upon the severity and type. In the most severe forms (types 0/1), individuals have the greatest muscle weakness requiring prompt intervention. Whereas the least severe form (type 4/adult onset), individuals may not seek the certain aspects of care until later (decades) in life. While types of SMA and individuals among each type may differ, therefore specific aspects of an individual's care can differ.
Medication
Nusinersen is used to treat spinal muscular atrophy. It is an antisense nucleotide that modifies the alternative splicing of the SMN2 gene. It is given directly to the central nervous system using an intrathecal injection.[26] It was approved in the US in 2016 and in the EU in 2017.[27]
Onasemnogene abeparvovec is a gene therapy treatment which uses self-complementary adeno-associated virus type 9 (scAAV-9) as a vector to deliver the SMN1 transgene. As an intravenous formulation, it was approved in 2019 in the US to treat those below 24 months of age. As of 2019, approvals in the EU and Japan are pending while an intrathecal formulation for older people is in development.
Breathing
The respiratory system is the most common system to be affected and the complications are the leading cause of death in SMA types 0/1 and 2. SMA type 3 can have similar respiratory problems, but it is more rare.[16] The complications that arise due to weakened intercostal muscles because of the lack of stimulation from the nerve. The diaphragm is less affected than the intercostal muscles.[16] Once weakened, the muscles never fully recover the same functional capacity to help in breathing and coughing as well as other functions. Therefore, breathing is more difficult and pose a risk of not getting enough oxygen/shallow breathing and insufficient clearance of airway secretions. These issues more commonly occurs while asleep, when muscles are more relaxed. Swallowing muscles in the pharynx can be affected, leading to aspiration coupled with a poor coughing mechanism increases the likelihood of infection/pneumonia.[28] Mobilizing and clearing secretions involve manual or mechanical chest physiotherapy with postural drainage, and manual or mechanical cough assistance device. To assist in breathing, Non-invasive ventilation (BiPAP) is frequently used and tracheostomy may be sometimes performed in more severe cases;[29] both methods of ventilation prolong survival to a comparable degree, although tracheostomy prevents speech development.[30]
Nutrition
The more severe the type of SMA, the more likely to have nutrition related health issues. Health issues can include difficulty in feeding, jaw opening, chewing and swallowing. Individuals with such difficulties can be at increase risk of over or undernutrition, failure to thrive and aspiration. Other nutritional issues, especially in individuals that are non-ambulatory (more severe types of SMA), include food not passing through the stomach quickly enough, gastric reflux, constipation, vomiting and bloating.[31] Therein, it could be necessary in SMA type I and people with more severe type II to have a feeding tube or gastrostomy.[31][32][33] Additionally, metabolic abnormalities resulting from SMA impair β-oxidation of fatty acids in muscles and can lead to organic acidemia and consequent muscle damage, especially when fasting.[34][35] It is suggested that people with SMA, especially those with more severe forms of the disease, reduce intake of fat and avoid prolonged fasting (i.e., eat more frequently than healthy people)[36] as well as choosing softer foods to avoid aspiration.[28] During an acute illness, especially in children, nutritional problems may first present or can exacerbate an existing problem (example: aspiration) as well as cause other health issues such as electrolyte and blood sugar disturbances.[37]
Orthopaedics
Skeletal problems associated with weak muscles in SMA include tight joints with limited range of movement, hip dislocations, spinal deformity, osteopenia, an increase risk of fractures and pain.[16] Weak muscles that normally stabilize joints such as the vertebral column lead to development of kyphosis and/or scoliosis and joint contracture.[16] Spine fusion is sometimes performed in people with SMA I/II once they reach the age of 8–10 to relieve the pressure of a deformed spine on the lungs. Furthermore, immobile individuals, posture and position on mobility devices as well as range of motion exercises, and bone strengthening can be important to prevent complications.[37] People with SMA might also benefit greatly from various forms of physiotherapy, occupational therapy and physical therapy.
Orthotic devices can be used to support the body and to aid walking. For example, orthotics such as AFOs (ankle foot orthoses) are used to stabilise the foot and to aid gait, TLSOs (thoracic lumbar sacral orthoses) are used to stabilise the torso. Assistive technologies may help in managing movement and daily activity and greatly increase the quality of life.
Other
Although the heart is not a matter of routine concern, a link between SMA and certain heart conditions has been suggested.[38][39][40][41]
Children with SMA do not differ from the general population in their behaviour; their cognitive development can be slightly faster, and certain aspects of their intelligence are above the average.[42][43][44] Despite their disability, SMA-affected people report high degree of satisfaction from life.[45]
Palliative care in SMA has been standardised in the Consensus Statement for Standard of Care in Spinal Muscular Atrophy[16] which has been recommended for standard adoption worldwide.
Prognosis
In lack of pharmacological treatment, people with SMA tend to deteriorate over time. Recently, survival has increased in severe SMA patients with aggressive and proactive supportive respiratory and nutritional support.[46]
If left untreated, the majority of children diagnosed with SMA type 0 and I do not reach the age of 4, recurrent respiratory problems being the primary cause of death.[47] With proper care, milder SMA type I cases (which account for approx. 10% of all SMA1 cases) live into adulthood.[48] Long-term survival in SMA type I is not sufficiently evidenced; however, recent advances in respiratory support seem to have brought down mortality.[49]
In untreated SMA type II, the course of the disease is slower to progress and life expectancy is less than the healthy population. Death before the age of 20 is frequent, although many people with SMA live to become parents and grandparents. SMA type III has normal or near-normal life expectancy if standards of care are followed. Type IV, adult-onset SMA usually means only mobility impairment and does not affect life expectancy.
Research directions
Since the underlying genetic cause of SMA was identified in 1995,[14] several therapeutic approaches have been proposed and investigated that primarily focus on increasing the availability of SMN protein in motor neurons.[50] The main research directions are as follows:
SMN1 gene replacement
Gene therapy in SMA aims at restoring the SMN1 gene function through inserting specially crafted nucleotide sequence (a SMN1 transgene) into the cell nucleus using a viral vector; scAAV-9 and scAAV-10 are the primary viral vectors under investigation. In 2019 an AAV9 therapy was approved: Onasemnogene abeparvovec.[51]
Only one programme has reached the clinical stage. Work on developing gene therapy for SMA is also conducted at the Institut de Myologie in Paris[52] and at the University of Oxford. In 2018, also Biogen announced working on a gene therapy product to treat SMA.[53]
SMN2 alternative splicing modulation
This approach aims at modifying the alternative splicing of the SMN2 gene to force it to code for higher percentage of full-length SMN protein. Sometimes it is also called gene conversion, because it attempts to convert the SMN2 gene functionally into SMN1 gene.
The following splicing modulators have reached clinical stage development:
- Branaplam (LMI070, NVS-SM1) is a proprietary small-molecule experimental drug administered orally and being developed by Novartis. As of October 2017 the compound remains in phase-II clinical trial in infants with SMA type 1 while trials in other patient categories are under development.[54]
- Risdiplam (RG7916, RO7034067) is a proprietary small-molecule drug administered orally and developed by PTC Therapeutics in collaboration with Hoffmann-La Roche and SMA Foundation. As of September 2018, risdiplam has advanced to phase II/III clinical trials across a wide spectrum of spinal muscular atrophy where it has shown encouraging early results.
Of discontinued clinical-stage molecules, RG3039, also known as Quinazoline495, was a proprietary quinazoline derivative developed by Repligen and licensed to Pfizer in March 2014 which was discontinued shortly after, having only completed phase I trials. PTK-SMA1 was a proprietary small-molecule splicing modulator of the tetracyclines group developed by Paratek Pharmaceutical and about to enter clinical development in 2010 which however never happened. RG7800 was a molecule akin to RG7916, developed by Hoffmann-La Roche and trialled on SMA patients in 2015, whose development was put on hold indefinitely due to long-term animal toxicity.
Basic research has also identified other compounds which modified SMN2 splicing in vitro, like sodium orthovanadate[55] and aclarubicin.[56] Morpholino-type antisense oligonucleotides, with the same cellular target as nusinersen, remain a subject of intense research, including at the University College London[57] and at the University of Oxford.[58]
SMN2 gene activation
This approach aims at increasing expression (activity) of the SMN2 gene, thus increasing the amount of full-length SMN protein available.
- Oral salbutamol (albuterol), a popular asthma medicine, showed therapeutic potential in SMA both in vitro[59] and in three small-scale clinical trials involving patients with SMA types 2 and 3,[60][61][62] besides offering respiratory benefits.
A few compounds initially showed promise but failed to demonstrate efficacy in clinical trials:
- Butyrates (sodium butyrate and sodium phenylbutyrate) held some promise in in vitro studies[63][64][65] but a clinical trial in symptomatic people did not confirm their efficacy.[66] Another clinical trial in pre-symptomatic types 1–2 infants was completed in 2015 but no results have been published.[67]
- Valproic acid (VPA) was used in SMA on an experimental basis in the 1990s and 2000s because in vitro research suggested its moderate effectiveness.[68][69] However, it demonstrated no efficacy in achievable concentrations when subjected to a large clinical trial.[70][71][72] It has also been proposed that it may be effective in a subset of people with SMA but its action may be suppressed by fatty acid translocase in others.[73] Others argue it may actually aggravate SMA symptoms.[74] It is currently not used due to the risk of severe side effects related to long-term use. A 2019 meta-analysis suggested that VPA may offer benefits, even without improving functional score.[75]
- Hydroxycarbamide (hydroxyurea) was shown effective in mouse models[76] and subsequently commercially researched by Novo Nordisk, Denmark, but demonstrated no effect on people with SMA in subsequent clinical trials.[77]
Compounds which increased SMN2 activity in vitro but did not make it to the clinical stage include growth hormone, various histone deacetylase inhibitors,[78] benzamide M344,[79] hydroxamic acids (CBHA, SBHA, entinostat, panobinostat,[80] trichostatin A,[81][82] vorinostat[83]), prolactin[84] as well as natural polyphenol compounds like resveratrol and curcumin.[85][86] Celecoxib, a p38 pathway activator, is sometimes used off-label by people with SMA based on a single animal study[87] but such use is not backed by clinical-stage research.
SMN stabilisation
SMN stabilisation aims at stabilising the SMNΔ7 protein, the short-lived defective protein coded by the SMN2 gene, so that it is able to sustain neuronal cells.[88]
No compounds have been taken forward to the clinical stage. Aminoglycosides showed capability to increase SMN protein availability in two studies.[89][90] Indoprofen offered some promise in vitro.[91]
Neuroprotection
Neuroprotective drugs aim at enabling the survival of motor neurons even with low levels of SMN protein.
- Olesoxime is a proprietary neuroprotective compound developed by the French company Trophos, later acquired by Hoffmann-La Roche, which showed stabilising effect in a phase-II clinical trial involving people with SMA types 2 and 3. Its development was discontinued in 2018 in view of competition with Spinraza and worse than expected data coming from an open-label extension trial.[92]
Of clinically studied compounds which did not show efficacy, thyrotropin-releasing hormone (TRH) held some promise in an open-label uncontrolled clinical trial[93][94][95] but did not prove effective in a subsequent double-blind placebo-controlled trial.[96] Riluzole, a drug that has mild clinical benefit in amyotrophic lateral sclerosis, was proposed to be similarly tested in SMA,[97][98] however a 2008–2010 trial in SMA types 2 and 3[99] was stopped early due to lack of satisfactory results.[100]
Compounds that had some neuroprotective effect in in vitro research but never moved to in vivo studies include β-lactam antibiotics (e.g., ceftriaxone)[101][102] and follistatin.[103]
Muscle restoration
This approach aims to counter the effect of SMA by targeting the muscle tissue instead of neurons.
- CK-2127107 (CK-107) is a skeletal troponin activator developed by Cytokinetics in cooperation with Astellas. The drug aims at increasing muscle reactivity despite lowered neural signalling. As of October 2016, the molecule is in a phase II clinical trial in adolescent and adults with SMA types 2, 3, and 4.[104]
Stem cells
In 2013–2014, a small number of SMA1 children in Italy received court-mandated stem cell injections following the Stamina scam, but the treatment was reported having no effect.[105][106]
Whilst stem cells never form a part of any recognised therapy for SMA, a number of private companies, usually located in countries with lax regulatory oversight, take advantage of media hype and market stem cell injections as a "cure" for a vast range of disorders, including SMA. The medical consensus is that such procedures offer no clinical benefit whilst carrying significant risk, therefore people with SMA are advised against them.[107][108]
Registries
People with SMA in the European Union can participate in clinical research by entering their details into registries managed by TREAT-NMD.[109]
See also
References
- "Spinal muscular atrophy". Genetic and Rare Diseases Information Center (GARD) – an NCATS Program. Retrieved 27 May 2019.
- "Spinal Muscular Atrophy". NORD (National Organization for Rare Disorders). Retrieved 27 May 2019.
- "Spinal Muscular Atrophy Fact Sheet | National Institute of Neurological Disorders and Stroke". NINDS. Retrieved 27 May 2019.
- "Spinal muscular atrophy". Genetics Home Reference. Retrieved 27 May 2019.
- "FDA approves innovative gene therapy to treat pediatric patients with spinal muscular atrophy, a rare disease and leading genetic cause of infant mortality". FDA. 24 May 2019. Retrieved 27 May 2019.
- Main M, Kairon H, Mercuri E, Muntoni F (2003). "The Hammersmith functional motor scale for children with spinal muscular atrophy: a scale to test ability and monitor progress in children with limited ambulation". European Journal of Paediatric Neurology. 7 (4): 155–9. doi:10.1016/S1090-3798(03)00060-6. PMID 12865054.
- Krosschell KJ, Maczulski JA, Crawford TO, Scott C, Swoboda KJ (July 2006). "A modified Hammersmith functional motor scale for use in multi-center research on spinal muscular atrophy". Neuromuscular Disorders. 16 (7): 417–26. doi:10.1016/j.nmd.2006.03.015. PMC 3260054. PMID 16750368.
- O'Hagen JM, Glanzman AM, McDermott MP, Ryan PA, Flickinger J, Quigley J, Riley S, Sanborn E, Irvine C, Martens WB, Annis C, Tawil R, Oskoui M, Darras BT, Finkel RS, De Vivo DC (October 2007). "An expanded version of the Hammersmith Functional Motor Scale for SMA II and III patients". Neuromuscular Disorders. 17 (9–10): 693–7. doi:10.1016/j.nmd.2007.05.009. PMID 17658255.
- Glanzman AM, O'Hagen JM, McDermott MP, Martens WB, Flickinger J, Riley S, Quigley J, Montes J, Dunaway S, Deng L, Chung WK, Tawil R, Darras BT, De Vivo DC, Kaufmann P, Finkel RS, et al. (Pediatric Neuromuscular Clinical Research Network for Spinal Muscular Atrophy (PNCR)) (December 2011). "Validation of the Expanded Hammersmith Functional Motor Scale in spinal muscular atrophy type II and III". Journal of Child Neurology. 26 (12): 1499–507. doi:10.1177/0883073811420294. PMID 21940700.
- Dubowitz V (January 2009). "Ramblings in the history of spinal muscular atrophy". Neuromuscular Disorders. 19 (1): 69–73. doi:10.1016/j.nmd.2008.10.004. PMID 18951794.
- Oskoui M, Darras BT, DeVivo DC (2017). "Chapter 1". In Sumner CJ, Paushkin S, Ko CP (eds.). Spinal Muscular Atrophy: Disease Mechanisms. Elsevier. ISBN 978-0-12-803685-3.
- Brzustowicz LM, Lehner T, Castilla LH, Penchaszadeh GK, Wilhelmsen KC, Daniels R, Davies KE, Leppert M, Ziter F, Wood D (April 1990). "Genetic mapping of chronic childhood-onset spinal muscular atrophy to chromosome 5q11.2-13.3". Nature. 344 (6266): 540–1. Bibcode:1990Natur.344..540B. doi:10.1038/344540a0. PMID 2320125.
- "Spinal muscular atrophy". Genetics Home Reference. Retrieved 15 May 2019.
- Lefebvre S, Bürglen L, Reboullet S, Clermont O, Burlet P, Viollet L, Benichou B, Cruaud C, Millasseau P, Zeviani M (January 1995). "Identification and characterization of a spinal muscular atrophy-determining gene". Cell. 80 (1): 155–65. doi:10.1016/0092-8674(95)90460-3. PMID 7813012.
- Passini MA, Bu J, Richards AM, Kinnecom C, Sardi SP, Stanek LM, Hua Y, Rigo F, Matson J, Hung G, Kaye EM, Shihabuddin LS, Krainer AR, Bennett CF, Cheng SH (March 2011). "Antisense oligonucleotides delivered to the mouse CNS ameliorate symptoms of severe spinal muscular atrophy". Science Translational Medicine. 3 (72): 72ra18. doi:10.1126/scitranslmed.3001777. PMC 3140425. PMID 21368223.
- Wang CH, Finkel RS, Bertini ES, Schroth M, Simonds A, Wong B, Aloysius A, Morrison L, Main M, Crawford TO, Trela A (August 2007). "Consensus statement for standard of care in spinal muscular atrophy". Journal of Child Neurology. 22 (8): 1027–49. doi:10.1177/0883073807305788. PMID 17761659.
- Jedrzejowska M, Milewski M, Zimowski J, Borkowska J, Kostera-Pruszczyk A, Sielska D, Jurek M, Hausmanowa-Petrusewicz I (2009). "Phenotype modifiers of spinal muscular atrophy: the number of SMN2 gene copies, deletion in the NAIP gene and probably gender influence the course of the disease". Acta Biochimica Polonica. 56 (1): 103–8. doi:10.18388/abp.2009_2521. PMID 19287802.
- Su YN, Hung CC, Lin SY, Chen FY, Chern JP, Tsai C, Chang TS, Yang CC, Li H, Ho HN, Lee CN (February 2011). Schrijver I (ed.). "Carrier screening for spinal muscular atrophy (SMA) in 107,611 pregnant women during the period 2005-2009: a prospective population-based cohort study". PLOS ONE. 6 (2): e17067. Bibcode:2011PLoSO...617067S. doi:10.1371/journal.pone.0017067. PMC 3045421. PMID 21364876.
- Sugarman EA, Nagan N, Zhu H, Akmaev VR, Zhou Z, Rohlfs EM, Flynn K, Hendrickson BC, Scholl T, Sirko-Osadsa DA, Allitto BA (January 2012). "Pan-ethnic carrier screening and prenatal diagnosis for spinal muscular atrophy: clinical laboratory analysis of >72,400 specimens". European Journal of Human Genetics. 20 (1): 27–32. doi:10.1038/ejhg.2011.134. PMC 3234503. PMID 21811307.
- Ottesen EW (January 2017). "ISS-N1 makes the First FDA-approved Drug for Spinal Muscular Atrophy". Translational Neuroscience. 8 (1): 1–6. doi:10.1515/tnsci-2017-0001. PMC 5382937. PMID 28400976.
- "Carrier Screening in the Age of Genomic Medicine – ACOG". www.acog.org. Retrieved 24 February 2017.
- Prior TW (November 2008). "Carrier screening for spinal muscular atrophy". Genetics in Medicine. 10 (11): 840–2. doi:10.1097/GIM.0b013e318188d069. PMC 3110347. PMID 18941424.
- Ar Rochmah M, Awano H, Awaya T, Harahap NI, Morisada N, Bouike Y, Saito T, Kubo Y, Saito K, Lai PS, Morioka I, Iijima K, Nishio H, Shinohara M (November 2017). "Spinal muscular atrophy carriers with two SMN1 copies". Brain & Development. 39 (10): 851–860. doi:10.1016/j.braindev.2017.06.002. PMID 28676237.
- Little SE, Janakiraman V, Kaimal A, Musci T, Ecker J, Caughey AB (March 2010). "The cost-effectiveness of prenatal screening for spinal muscular atrophy". American Journal of Obstetrics and Gynecology. 202 (3): 253.e1–7. doi:10.1016/j.ajog.2010.01.032. PMID 20207244.
- Prior TW (November 2008). "Carrier screening for spinal muscular atrophy". Genetics in Medicine. 10 (11): 840–2. doi:10.1097/GIM.0b013e318188d069. PMC 3110347. PMID 18941424.
- Grant C (27 December 2016). "Surprise Drug Approval Is Holiday Gift for Biogen". Wall Street Journal. ISSN 0099-9660. Retrieved 27 December 2016.
- "SPINRAZA® (Nusinersen) Approved in the European Union as First Treatment for Spinal Muscular Atrophy". AFP. 1 June 2017. Retrieved 1 June 2017.
- Bodamer O (November 2017). "Spinal Muscular Atrophy". uptodate.com. Retrieved 1 December 2017.
- Bach JR, Niranjan V, Weaver B (April 2000). "Spinal muscular atrophy type 1: A noninvasive respiratory management approach". Chest. 117 (4): 1100–5. doi:10.1378/chest.117.4.1100. PMID 10767247.
- Bach JR, Saltstein K, Sinquee D, Weaver B, Komaroff E (May 2007). "Long-term survival in Werdnig-Hoffmann disease". American Journal of Physical Medicine & Rehabilitation. 86 (5): 339–45 quiz 346–8, 379. doi:10.1097/PHM.0b013e31804a8505. PMID 17449977.
- Messina S, Pane M, De Rose P, Vasta I, Sorleti D, Aloysius A, Sciarra F, Mangiola F, Kinali M, Bertini E, Mercuri E (May 2008). "Feeding problems and malnutrition in spinal muscular atrophy type II". Neuromuscular Disorders. 18 (5): 389–93. doi:10.1016/j.nmd.2008.02.008. PMID 18420410.
- Chen YS, Shih HH, Chen TH, Kuo CH, Jong YJ (March 2012). "Prevalence and risk factors for feeding and swallowing difficulties in spinal muscular atrophy types II and III". The Journal of Pediatrics. 160 (3): 447–451.e1. doi:10.1016/j.jpeds.2011.08.016. PMID 21924737.
- Tilton AH, Miller MD, Khoshoo V (June 1998). "Nutrition and swallowing in pediatric neuromuscular patients". Seminars in Pediatric Neurology. 5 (2): 106–15. doi:10.1016/S1071-9091(98)80026-0. PMID 9661244.
- Tein I, Sloane AE, Donner EJ, Lehotay DC, Millington DS, Kelley RI (January 1995). "Fatty acid oxidation abnormalities in childhood-onset spinal muscular atrophy: primary or secondary defect(s)?". Pediatric Neurology. 12 (1): 21–30. doi:10.1016/0887-8994(94)00100-G. PMID 7748356.
- Crawford TO, Sladky JT, Hurko O, Besner-Johnston A, Kelley RI (March 1999). "Abnormal fatty acid metabolism in childhood spinal muscular atrophy". Annals of Neurology. 45 (3): 337–43. doi:10.1002/1531-8249(199903)45:3<337::AID-ANA9>3.0.CO;2-U. PMID 10072048.
- Leighton S (2003). "Nutrition issues associated with spinal muscular atrophy". Nutrition & Dietetics. 60 (2): 92–96.
- Apkon S (Summer 2017). "SMA CARE SERIES – Musculoskeletal System" (PDF). www.curesma.org.
- Rudnik-Schöneborn S, Heller R, Berg C, Betzler C, Grimm T, Eggermann T, Eggermann K, Wirth R, Wirth B, Zerres K (October 2008). "Congenital heart disease is a feature of severe infantile spinal muscular atrophy". Journal of Medical Genetics. 45 (10): 635–8. doi:10.1136/jmg.2008.057950. PMID 18662980.
- Heier CR, Satta R, Lutz C, DiDonato CJ (October 2010). "Arrhythmia and cardiac defects are a feature of spinal muscular atrophy model mice". Human Molecular Genetics. 19 (20): 3906–18. doi:10.1093/hmg/ddq330. PMC 2947406. PMID 20693262.
- Shababi M, Habibi J, Yang HT, Vale SM, Sewell WA, Lorson CL (October 2010). "Cardiac defects contribute to the pathology of spinal muscular atrophy models". Human Molecular Genetics. 19 (20): 4059–71. doi:10.1093/hmg/ddq329. PMID 20696672.
- Bevan AK, Hutchinson KR, Foust KD, Braun L, McGovern VL, Schmelzer L, Ward JG, Petruska JC, Lucchesi PA, Burghes AH, Kaspar BK (October 2010). "Early heart failure in the SMNDelta7 model of spinal muscular atrophy and correction by postnatal scAAV9-SMN delivery". Human Molecular Genetics. 19 (20): 3895–905. doi:10.1093/hmg/ddq300. PMC 2947399. PMID 20639395.
- von Gontard A, Zerres K, Backes M, Laufersweiler-Plass C, Wendland C, Melchers P, Lehmkuhl G, Rudnik-Schöneborn S (February 2002). "Intelligence and cognitive function in children and adolescents with spinal muscular atrophy". Neuromuscular Disorders. 12 (2): 130–6. doi:10.1016/S0960-8966(01)00274-7. PMID 11738354.
- Billard C, Gillet P, Signoret JL, Uicaut E, Bertrand P, Fardeau M, Barthez-Carpentier MA, Santini JJ (1992). "Cognitive functions in Duchenne muscular dystrophy: a reappraisal and comparison with spinal muscular atrophy". Neuromuscular Disorders. 2 (5–6): 371–8. doi:10.1016/S0960-8966(06)80008-8. PMID 1300185.
- Laufersweiler-Plass C, Rudnik-Schöneborn S, Zerres K, Backes M, Lehmkuhl G, von Gontard A (January 2003). "Behavioural problems in children and adolescents with spinal muscular atrophy and their siblings". Developmental Medicine and Child Neurology. 45 (1): 44–9. doi:10.1017/S0012162203000082. PMID 12549754.
- de Oliveira CM, Araújo AP (January 2011). "Self-reported quality of life has no correlation with functional status in children and adolescents with spinal muscular atrophy". European Journal of Paediatric Neurology. 15 (1): 36–9. doi:10.1016/j.ejpn.2010.07.003. PMID 20800519.
- Darras B, Finkel R (2017). Spinal Muscular Atrophy. United Kingdom, United States: Elsevier. p. 417. ISBN 978-0-12-803685-3.
- Yuan N, Wang CH, Trela A, Albanese CT (June 2007). "Laparoscopic Nissen fundoplication during gastrostomy tube placement and noninvasive ventilation may improve survival in type I and severe type II spinal muscular atrophy". Journal of Child Neurology. 22 (6): 727–31. doi:10.1177/0883073807304009. PMID 17641258.
- Bach JR (May 2007). "Medical considerations of long-term survival of Werdnig-Hoffmann disease". American Journal of Physical Medicine & Rehabilitation. 86 (5): 349–55. doi:10.1097/PHM.0b013e31804b1d66. PMID 17449979.
- Oskoui M, Levy G, Garland CJ, Gray JM, O'Hagen J, De Vivo DC, Kaufmann P (November 2007). "The changing natural history of spinal muscular atrophy type 1". Neurology. 69 (20): 1931–6. doi:10.1212/01.wnl.0000290830.40544.b9. PMID 17998484.
- d'Ydewalle C, Sumner CJ (April 2015). "Spinal Muscular Atrophy Therapeutics: Where do we Stand?". Neurotherapeutics. 12 (2): 303–16. doi:10.1007/s13311-015-0337-y. PMC 4404440. PMID 25631888.
- "$2.1m Novartis gene therapy to become world's most expensive drug". The Guardian. Reuters. 25 May 2019. ISSN 0261-3077.
- Benkhelifa-Ziyyat S, Besse A, Roda M, Duque S, Astord S, Carcenac R, Marais T, Barkats M (February 2013). "Intramuscular scAAV9-SMN injection mediates widespread gene delivery to the spinal cord and decreases disease severity in SMA mice". Molecular Therapy. 21 (2): 282–90. doi:10.1038/mt.2012.261. PMC 3594018. PMID 23295949.
- "Biogen Releases Community Statement on Spinraza Access and New Data | Cure SMA". www.curesma.org. Retrieved 11 September 2018.
- "Novartis Releases Update on LMI070 (Branaplam) Clinical Trial". CureSMA. Retrieved 7 October 2017.
- Zhang ML, Lorson CL, Androphy EJ, Zhou J (October 2001). "An in vivo reporter system for measuring increased inclusion of exon 7 in SMN2 mRNA: potential therapy of SMA". Gene Therapy. 8 (20): 1532–8. doi:10.1038/sj.gt.3301550. PMID 11704813.
- Andreassi C, Jarecki J, Zhou J, Coovert DD, Monani UR, Chen X, Whitney M, Pollok B, Zhang M, Androphy E, Burghes AH (November 2001). "Aclarubicin treatment restores SMN levels to cells derived from type I spinal muscular atrophy patients". Human Molecular Genetics. 10 (24): 2841–9. doi:10.1093/hmg/10.24.2841. PMID 11734549.
- Zhou H, Meng J, Marrosu E, Janghra N, Morgan J, Muntoni F (November 2015). "Repeated low doses of morpholino antisense oligomer: an intermediate mouse model of spinal muscular atrophy to explore the window of therapeutic response". Human Molecular Genetics. 24 (22): 6265–77. doi:10.1093/hmg/ddv329. PMC 4614699. PMID 26264577.
- Hammond SM, Hazell G, Shabanpoor F, Saleh AF, Bowerman M, Sleigh JN, Meijboom KE, Zhou H, Muntoni F, Talbot K, Gait MJ, Wood MJ (September 2016). "Systemic peptide-mediated oligonucleotide therapy improves long-term survival in spinal muscular atrophy". Proceedings of the National Academy of Sciences of the United States of America. 113 (39): 10962–7. doi:10.1073/pnas.1605731113. PMC 5047168. PMID 27621445.
- Angelozzi C, Borgo F, Tiziano FD, Martella A, Neri G, Brahe C (January 2008). "Salbutamol increases SMN mRNA and protein levels in spinal muscular atrophy cells". Journal of Medical Genetics. 45 (1): 29–31. doi:10.1136/jmg.2007.051177. PMID 17932121.
- Pane M, Staccioli S, Messina S, D'Amico A, Pelliccioni M, Mazzone ES, Cuttini M, Alfieri P, Battini R, Main M, Muntoni F, Bertini E, Villanova M, Mercuri E (July 2008). "Daily salbutamol in young patients with SMA type II". Neuromuscular Disorders. 18 (7): 536–40. doi:10.1016/j.nmd.2008.05.004. PMID 18579379.
- Tiziano FD, Lomastro R, Pinto AM, Messina S, D'Amico A, Fiori S, Angelozzi C, Pane M, Mercuri E, Bertini E, Neri G, Brahe C (December 2010). "Salbutamol increases survival motor neuron (SMN) transcript levels in leucocytes of spinal muscular atrophy (SMA) patients: relevance for clinical trial design". Journal of Medical Genetics. 47 (12): 856–8. doi:10.1136/jmg.2010.080366. PMID 20837492.
- Morandi L, Abiusi E, Pasanisi MB, Lomastro R, Fiori S, Di Pietro L, Angelini C, Sorarù G, Gaiani A, Mongini T, Vercelli L (2013). "P.6.4 Salbutamol tolerability and efficacy in adult type III SMA patients: Results of a multicentric, molecular and clinical, double-blind, placebo-controlled study". Neuromuscular Disorders. 23 (9–10): 771. doi:10.1016/j.nmd.2013.06.475.
- Chang JG, Hsieh-Li HM, Jong YJ, Wang NM, Tsai CH, Li H (August 2001). "Treatment of spinal muscular atrophy by sodium butyrate". Proceedings of the National Academy of Sciences of the United States of America. 98 (17): 9808–13. Bibcode:2001PNAS...98.9808C. doi:10.1073/pnas.171105098. PMC 55534. PMID 11504946.
- Andreassi C, Angelozzi C, Tiziano FD, Vitali T, De Vincenzi E, Boninsegna A, Villanova M, Bertini E, Pini A, Neri G, Brahe C (January 2004). "Phenylbutyrate increases SMN expression in vitro: relevance for treatment of spinal muscular atrophy". European Journal of Human Genetics. 12 (1): 59–65. doi:10.1038/sj.ejhg.5201102. PMID 14560316.
- Brahe C, Vitali T, Tiziano FD, Angelozzi C, Pinto AM, Borgo F, Moscato U, Bertini E, Mercuri E, Neri G (February 2005). "Phenylbutyrate increases SMN gene expression in spinal muscular atrophy patients". European Journal of Human Genetics. 13 (2): 256–9. doi:10.1038/sj.ejhg.5201320. PMID 15523494.
- Mercuri E, Bertini E, Messina S, Solari A, D'Amico A, Angelozzi C, Battini R, Berardinelli A, Boffi P, Bruno C, Cini C, Colitto F, Kinali M, Minetti C, Mongini T, Morandi L, Neri G, Orcesi S, Pane M, Pelliccioni M, Pini A, Tiziano FD, Villanova M, Vita G, Brahe C (January 2007). "Randomized, double-blind, placebo-controlled trial of phenylbutyrate in spinal muscular atrophy". Neurology. 68 (1): 51–5. doi:10.1212/01.wnl.0000249142.82285.d6. PMID 17082463.
- Clinical trial number NCT00528268 for "Study to Evaluate Sodium Phenylbutyrate in Pre-symptomatic Infants With Spinal Muscular Atrophy (STOPSMA)" at ClinicalTrials.gov
- Brichta L, Hofmann Y, Hahnen E, Siebzehnrubl FA, Raschke H, Blumcke I, Eyupoglu IY, Wirth B (October 2003). "Valproic acid increases the SMN2 protein level: a well-known drug as a potential therapy for spinal muscular atrophy". Human Molecular Genetics. 12 (19): 2481–9. doi:10.1093/hmg/ddg256. PMID 12915451.
- Tsai LK, Tsai MS, Ting CH, Li H (November 2008). "Multiple therapeutic effects of valproic acid in spinal muscular atrophy model mice". Journal of Molecular Medicine. 86 (11): 1243–54. doi:10.1007/s00109-008-0388-1. PMID 18649067.
- Swoboda KJ, Scott CB, Crawford TO, Simard LR, Reyna SP, Krosschell KJ, Acsadi G, Elsheik B, Schroth MK, D'Anjou G, LaSalle B, Prior TW, Sorenson SL, Maczulski JA, Bromberg MB, Chan GM, Kissel JT, et al. (Project Cure Spinal Muscular Atrophy Investigators Network) (August 2010). Boutron I (ed.). "SMA CARNI-VAL trial part I: double-blind, randomized, placebo-controlled trial of L-carnitine and valproic acid in spinal muscular atrophy". PLOS ONE. 5 (8): e12140. Bibcode:2010PLoSO...512140S. doi:10.1371/journal.pone.0012140. PMC 2924376. PMID 20808854.
- Kissel JT, Scott CB, Reyna SP, Crawford TO, Simard LR, Krosschell KJ, Acsadi G, Elsheik B, Schroth MK, D'Anjou G, LaSalle B, Prior TW, Sorenson S, Maczulski JA, Bromberg MB, Chan GM, Swoboda KJ, et al. (Project Cure Spinal Muscular Atrophy Investigators' Network) (2011). "SMA CARNIVAL TRIAL PART II: a prospective, single-armed trial of L-carnitine and valproic acid in ambulatory children with spinal muscular atrophy". PLOS ONE. 6 (7): e21296. Bibcode:2011PLoSO...621296K. doi:10.1371/journal.pone.0021296. PMC 3130730. PMID 21754985.
- Darbar IA, Plaggert PG, Resende MB, Zanoteli E, Reed UC (March 2011). "Evaluation of muscle strength and motor abilities in children with type II and III spinal muscle atrophy treated with valproic acid". BMC Neurology. 11: 36. doi:10.1186/1471-2377-11-36. PMC 3078847. PMID 21435220.
- Garbes L, Heesen L, Hölker I, Bauer T, Schreml J, Zimmermann K, Thoenes M, Walter M, Dimos J, Peitz M, Brüstle O, Heller R, Wirth B (January 2013). "VPA response in SMA is suppressed by the fatty acid translocase CD36". Human Molecular Genetics. 22 (2): 398–407. doi:10.1093/hmg/dds437. PMID 23077215.
- Rak K, Lechner BD, Schneider C, Drexl H, Sendtner M, Jablonka S (December 2009). "Valproic acid blocks excitability in SMA type I mouse motor neurons". Neurobiology of Disease. 36 (3): 477–87. doi:10.1016/j.nbd.2009.08.014. PMID 19733665.
- Elshafay A, Hieu TH, Doheim MF, Kassem MA, ELdoadoa MF, Holloway SK, Abo-Elghar H, Hirayama K, Huy NT (March 2019). "Efficacy and Safety of Valproic Acid for Spinal Muscular Atrophy: A Systematic Review and Meta-Analysis". CNS Drugs. 33 (3): 239–250. doi:10.1007/s40263-019-00606-6. PMID 30796634.
- Grzeschik SM, Ganta M, Prior TW, Heavlin WD, Wang CH (August 2005). "Hydroxyurea enhances SMN2 gene expression in spinal muscular atrophy cells". Annals of Neurology. 58 (2): 194–202. doi:10.1002/ana.20548. PMID 16049920.
- Chen TH, Chang JG, Yang YH, Mai HH, Liang WC, Wu YC, Wang HY, Huang YB, Wu SM, Chen YC, Yang SN, Jong YJ (December 2010). "Randomized, double-blind, placebo-controlled trial of hydroxyurea in spinal muscular atrophy". Neurology. 75 (24): 2190–7. doi:10.1212/WNL.0b013e3182020332. PMID 21172842.
- Evans MC, Cherry JJ, Androphy EJ (October 2011). "Differential regulation of the SMN2 gene by individual HDAC proteins". Biochemical and Biophysical Research Communications. 414 (1): 25–30. doi:10.1016/j.bbrc.2011.09.011. PMC 6538936. PMID 21925145.
- Riessland M, Brichta L, Hahnen E, Wirth B (August 2006). "The benzamide M344, a novel histone deacetylase inhibitor, significantly increases SMN2 RNA/protein levels in spinal muscular atrophy cells". Human Genetics. 120 (1): 101–10. doi:10.1007/s00439-006-0186-1. PMID 16724231.
- Garbes L, Riessland M, Hölker I, Heller R, Hauke J, Tränkle C, Coras R, Blümcke I, Hahnen E, Wirth B (October 2009). "LBH589 induces up to 10-fold SMN protein levels by several independent mechanisms and is effective even in cells from SMA patients non-responsive to valproate". Human Molecular Genetics. 18 (19): 3645–58. doi:10.1093/hmg/ddp313. PMID 19584083.
- Narver HL, Kong L, Burnett BG, Choe DW, Bosch-Marcé M, Taye AA, Eckhaus MA, Sumner CJ (October 2008). "Sustained improvement of spinal muscular atrophy mice treated with trichostatin A plus nutrition". Annals of Neurology. 64 (4): 465–70. doi:10.1002/ana.21449. PMID 18661558.
- Avila AM, Burnett BG, Taye AA, Gabanella F, Knight MA, Hartenstein P, Cizman Z, Di Prospero NA, Pellizzoni L, Fischbeck KH, Sumner CJ (March 2007). "Trichostatin A increases SMN expression and survival in a mouse model of spinal muscular atrophy". The Journal of Clinical Investigation. 117 (3): 659–71. doi:10.1172/JCI29562. PMC 1797603. PMID 17318264.
- Riessland M, Ackermann B, Förster A, Jakubik M, Hauke J, Garbes L, Fritzsche I, Mende Y, Blumcke I, Hahnen E, Wirth B (April 2010). "SAHA ameliorates the SMA phenotype in two mouse models for spinal muscular atrophy". Human Molecular Genetics. 19 (8): 1492–506. doi:10.1093/hmg/ddq023. PMID 20097677.
- Farooq F, Molina FA, Hadwen J, MacKenzie D, Witherspoon L, Osmond M, Holcik M, MacKenzie A (August 2011). "Prolactin increases SMN expression and survival in a mouse model of severe spinal muscular atrophy via the STAT5 pathway". The Journal of Clinical Investigation. 121 (8): 3042–50. doi:10.1172/JCI46276. PMC 3148738. PMID 21785216.
- Sakla MS, Lorson CL (January 2008). "Induction of full-length survival motor neuron by polyphenol botanical compounds". Human Genetics. 122 (6): 635–43. doi:10.1007/s00439-007-0441-0. PMID 17962980.
- Dayangaç-Erden D, Bora G, Ayhan P, Kocaefe C, Dalkara S, Yelekçi K, Demir AS, Erdem-Yurter H (March 2009). "Histone deacetylase inhibition activity and molecular docking of (e )-resveratrol: its therapeutic potential in spinal muscular atrophy". Chemical Biology & Drug Design. 73 (3): 355–64. CiteSeerX 10.1.1.515.8424. doi:10.1111/j.1747-0285.2009.00781.x. PMID 19207472.
- Farooq F, Abadía-Molina F, MacKenzie D, Hadwen J, Shamim F, O'Reilly S, Holcik M, MacKenzie A (September 2013). "Celecoxib increases SMN and survival in a severe spinal muscular atrophy mouse model via p38 pathway activation". Human Molecular Genetics. 22 (17): 3415–24. doi:10.1093/hmg/ddt191. PMID 23656793.
- Burnett BG, Muñoz E, Tandon A, Kwon DY, Sumner CJ, Fischbeck KH (March 2009). "Regulation of SMN protein stability". Molecular and Cellular Biology. 29 (5): 1107–15. doi:10.1128/MCB.01262-08. PMC 2643817. PMID 19103745.
- Mattis VB, Rai R, Wang J, Chang CW, Coady T, Lorson CL (November 2006). "Novel aminoglycosides increase SMN levels in spinal muscular atrophy fibroblasts". Human Genetics. 120 (4): 589–601. doi:10.1007/s00439-006-0245-7. PMID 16951947.
- Mattis VB, Fosso MY, Chang CW, Lorson CL (November 2009). "Subcutaneous administration of TC007 reduces disease severity in an animal model of SMA". BMC Neuroscience. 10: 142. doi:10.1186/1471-2202-10-142. PMC 2789732. PMID 19948047.
- Lunn MR, Root DE, Martino AM, Flaherty SP, Kelley BP, Coovert DD, Burghes AH, Man NT, Morris GE, Zhou J, Androphy EJ, Sumner CJ, Stockwell BR (November 2004). "Indoprofen upregulates the survival motor neuron protein through a cyclooxygenase-independent mechanism". Chemistry & Biology. 11 (11): 1489–93. doi:10.1016/j.chembiol.2004.08.024. PMC 3160629. PMID 15555999.
- Taylor NP (1 June 2018). "Roche scraps €120M SMA drug after hitting 'many difficulties'". www.fiercebiotech.com. Retrieved 8 June 2018.
- Takeuchi Y, Miyanomae Y, Komatsu H, Oomizono Y, Nishimura A, Okano S, Nishiki T, Sawada T (July 1994). "Efficacy of thyrotropin-releasing hormone in the treatment of spinal muscular atrophy". Journal of Child Neurology. 9 (3): 287–9. doi:10.1177/088307389400900313. PMID 7930408.
- Tzeng AC, Cheng J, Fryczynski H, Niranjan V, Stitik T, Sial A, Takeuchi Y, Foye P, DePrince M, Bach JR (2000). "A study of thyrotropin-releasing hormone for the treatment of spinal muscular atrophy: a preliminary report". American Journal of Physical Medicine & Rehabilitation. 79 (5): 435–40. doi:10.1097/00002060-200009000-00005. PMID 10994885.
- Kato Z, Okuda M, Okumura Y, Arai T, Teramoto T, Nishimura M, Kaneko H, Kondo N (August 2009). "Oral administration of the thyrotropin-releasing hormone (TRH) analogue, taltireline hydrate, in spinal muscular atrophy". Journal of Child Neurology. 24 (8): 1010–2. doi:10.1177/0883073809333535. PMID 19666885.
- Wadman, Renske I; Bosboom, Wendy MJ; van den Berg, Leonard H; Wokke, John HJ; Iannaccone, Susan T; Vrancken, Alexander FJE (7 December 2011), "Drug treatment for spinal muscular atrophy type I", in The Cochrane Collaboration (ed.), Cochrane Database of Systematic Reviews, John Wiley & Sons, Ltd, doi:10.1002/14651858.cd006281.pub3
- Haddad H, Cifuentes-Diaz C, Miroglio A, Roblot N, Joshi V, Melki J (October 2003). "Riluzole attenuates spinal muscular atrophy disease progression in a mouse model". Muscle & Nerve. 28 (4): 432–7. doi:10.1002/mus.10455. PMID 14506714.
- Dimitriadi M, Kye MJ, Kalloo G, Yersak JM, Sahin M, Hart AC (April 2013). "The neuroprotective drug riluzole acts via small conductance Ca2+-activated K+ channels to ameliorate defects in spinal muscular atrophy models". The Journal of Neuroscience. 33 (15): 6557–62. doi:10.1523/JNEUROSCI.1536-12.2013. PMC 3652322. PMID 23575853.
- Clinical trial number NCT00774423 for "Study to Evaluate the Efficacy of Riluzole in Children and Young Adults With Spinal Muscular Atrophy (SMA)" at ClinicalTrials.gov
- "Riluzole: premiers résultats décevants" (in French). AFM Téléthon. 22 September 2010.
- Nizzardo M, Nardini M, Ronchi D, Salani S, Donadoni C, Fortunato F, Colciago G, Falcone M, Simone C, Riboldi G, Govoni A, Bresolin N, Comi GP, Corti S (June 2011). "Beta-lactam antibiotic offers neuroprotection in a spinal muscular atrophy model by multiple mechanisms" (PDF). Experimental Neurology. 229 (2): 214–25. doi:10.1016/j.expneurol.2011.01.017. hdl:2434/425410. PMID 21295027.
- Hedlund E (September 2011). "The protective effects of β-lactam antibiotics in motor neuron disorders". Experimental Neurology. 231 (1): 14–8. doi:10.1016/j.expneurol.2011.06.002. PMID 21693120.
- Rose FF, Mattis VB, Rindt H, Lorson CL (March 2009). "Delivery of recombinant follistatin lessens disease severity in a mouse model of spinal muscular atrophy". Human Molecular Genetics. 18 (6): 997–1005. doi:10.1093/hmg/ddn426. PMC 2649020. PMID 19074460.
- "CK-2127107".
- Carrozzi M, Amaddeo A, Biondi A, Zanus C, Monti F, Alessandro V (November 2012). "Stem cells in severe infantile spinal muscular atrophy (SMA1)". Neuromuscular Disorders. 22 (11): 1032–4. doi:10.1016/j.nmd.2012.09.005. PMID 23046997.
- Mercuri E, Bertini E (December 2012). "Stem cells in severe infantile spinal muscular atrophy". Neuromuscular Disorders. 22 (12): 1105. doi:10.1016/j.nmd.2012.11.001. PMID 23206850.
- Committee for Advanced Therapies and CAT Scientific Secretariat (August 2010). "Use of unregulated stem-cell based medicinal products". Lancet. 376 (9740): 514. doi:10.1016/S0140-6736(10)61249-4. PMID 20709228.
- European Medicines Agency (16 April 2010). "Concerns over unregulated medicinal products containing stem cells" (PDF). European Medicines Agency.
- "National registries for DMD, SMA and DM". Archived from the original on 22 January 2011.
Further reading
- Parano E, Pavone L, Falsaperla R, Trifiletti R, Wang C (August 1996). "Molecular basis of phenotypic heterogeneity in siblings with spinal muscular atrophy". Annals of Neurology. 40 (2): 247–51. doi:10.1002/ana.410400219. PMID 8773609.
- Wang CH, Finkel RS, Bertini ES, Schroth M, Simonds A, Wong B, Aloysius A, Morrison L, Main M, Crawford TO, Trela A (August 2007). "Consensus statement for standard of care in spinal muscular atrophy". Journal of Child Neurology. 22 (8): 1027–49. doi:10.1177/0883073807305788. PMID 17761659.