Outpatient and Ambulatory Care Settings
For information on screening patients for Ebola, see FAQs on Screening for Ebola Virus Disease. For information on caring for survivors of Ebola, see Interim Guidance for Management of Survivors of Ebola Virus Disease in U.S. Healthcare Settings and Messages for the Care of Survivors of Ebola.
Page Summary
Who this is for: Ambulatory care (outpatient) staff members. Ambulatory care settings can include community health centers, urgent care centers, retail clinics, hospital-based outpatient clinics, non-hospital based clinics and physician offices, ambulatory surgical centers, public health clinics, imaging centers, oncology clinics, ambulatory behavioral health and substance abuse clinics, physical therapy, rehabilitation centers, dental offices, school health clinics (college and other), home health care, and hospice (non-hospital)
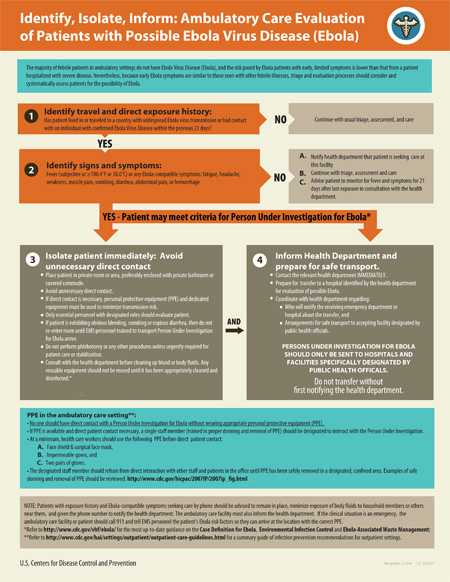
What this is for: Guidance to help ambulatory care staff members evaluate whether or not a patient might have Ebola virus disease (EVD). Staff members in ambulatory care settings should use this information to follow the 3 steps of the "Identify, Isolate, and Inform" strategy. CDC recommends staff members screen all patients with travel histories, exposure, or clinical symptoms that might suggest the person could have EVD.
How this relates to other guidance: Given that people with a risk of exposure to Ebola virus are being closely monitored by state and local health departments and directed to designated facilities for evaluation should they become ill, it is unlikely that patients with EVD will arrive unannounced at an outpatient setting. If staff members do identify a patient with possible EVD, they should immediately isolate the patient and contact the local or state health department so the patient can be transported to a designated hospital.
Key Points
- Most patients with fever and other symptoms coming to an ambulatory care facility don’t have EVD, but it is important that staff members know how to identify and manage patients who might have EVD.
- Staff members should be ready to take 3 steps: Identify, Isolate, and Inform.
- Ask every patient if, in the last 21 days, they traveled to a country with widespread transmission or uncertain control measures, or had contact with someone with confirmed EVD.
- If a patient appears to be at risk for EVD, isolate the patient immediately, avoid unnecessary direct contact, determine personal protective equipment needed, and notify the health department to arrange a transfer to a facility that can further assess the patient.
- Do not transfer the patient without first notifying the health department; these patients should only be transferred to a facility approved by public health authorities.
- Page last reviewed: March 28, 2016
- Page last updated: March 28, 2016
- Content source:


 ShareCompartir
ShareCompartir