For General Healthcare Settings in West Africa: Managing Patient Flow During Triage, Isolation, and Care of Patients Under Investigation or with Confirmed Ebola Virus Disease (EVD)
Page Summary
Who this is for: Healthcare workers who are now or will be working in general healthcare settings in West African countries with widespread Ebola transmission. This is not intended for those working in Ebola treatment units (ETUs) or Ebola care centers (ECCs).
What this is for: To help reduce the spread of infection in healthcare settings with patients under investigation (PUIs) for Ebola virus disease (EVD) or patients with confirmed EVD, and emphasize the importance of standardizing and prioritizing infection control practices.
How to use: To guide the development and implementation of an infection control plan to prevent the spread of EVD in general healthcare facilities.
Key Points
- A greater awareness and adherence to recommended infection control practices must occur in general healthcare settings to protect healthcare workers and uninfected patients from EVD.
- Preventing transmission of Ebola virus requires a well-considered plan that prioritizes 1) identifying and isolating PUIs, 2) protecting patients and healthcare workers, 3) cleaning up safely, and 4) managing PUIs safely and compassionately.
-
To be effective, each component of an infection control plan must be rigorously and meticulously followed.
This site provides guidance for general healthcare settings, which are healthcare settings not officially dedicated to providing care and treatment for patients with EVD. General healthcare settings include
- Peripheral health units
- Health posts
- Clinics
- Outpatient departments
- Inpatient units in hospitals
The first step in screening and isolation PUIs is to make sure each healthcare facility is set up to properly conduct screening and isolation. This will increase identification of new cases and allow more effective infection control. This set-up will ideally be completed before the PUI comes to the clinic, to be fully prepared.
All healthcare facilities must have the following specific areas:
- Screening area
- Area for patients and staff not under investigation (“cold”)
- Area for isolation of PUIs (“hot”)
- Area to put on personal protective equipment (PPE) outside the isolation area
- Area to remove PPE outside the isolation area
- Separate commode buckets or latrine pots for suspect Ebola patients
- Burning pit or incinerator for burnable waste
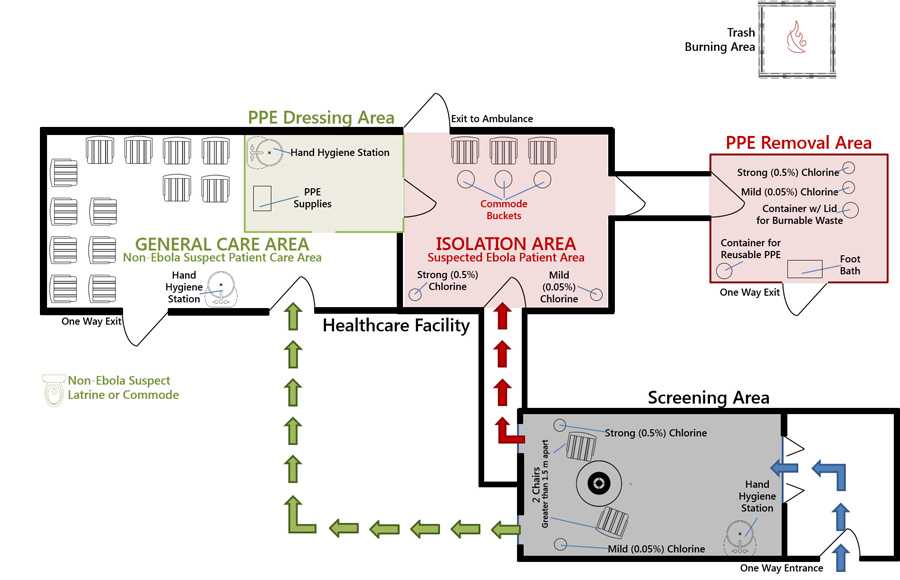
These areas should be clearly defined (for example, by physical boundaries such as rope or doorways with clear signage). Existing clinic rooms and resources can be used by dividing the clinic into these areas.
Setting Up a Screening Area
- Identify a place outside near the entrance of the healthcare facility where screening will take place. All clinic entry should occur through this one entrance. All other entrances should be blocked to keep people from entering at different points.
- Set up a table with two chairs (not covered in fabric, as these are difficult to disinfect). Chairs should be greater than 1.5 meters (or 5 feet) apart.
- Set up the required items at the screening site. These include the following:
- Hand hygiene station that has mild (0.05%) chlorinated water, soap, or alcohol-based hand sanitizer
- Hand-washing poster
- Two or more working thermometers (infrared, digital, or mercury)
- Mild chlorine solution (0.05%) to clean the thermometers
- Disposable towels to clean the thermometers
- Small waste bin (for used cotton wool and gloves)
- Box of gloves
- Face shields (if not available, face masks and goggles can replace face shields)
- Screening flowchart—laminated and located at the screening table
Have all patients wash their hands thoroughly with the mild (0.05%) chlorine solution or soap and water on arrival at the screening site. They should be asked to use the handwashing poster as a guide.
Setting Up Area for Patients and Staff Not Under Investigation (“Cold” Area)
The clean area of the clinic can operate as it normally does, with these two exceptions:
- Set up of handwashing stations throughout the clean area to encourage handwashing.
- PPE supplies should be available in all patient care areas. All staff should wear at least basic PPE (boots, gloves and face shield or boots, gloves, goggles and face mask) when caring for any patient.
Setting Up the Isolation Area
An isolation area ("hot area") must be prepared before patients arrive to the clinic. The isolation area should be separated from the regular clinic (“cold” area) and should be used ONLY for PUIs. This area must be considered contaminated and MUST NOT be used for treatment of patients not under investigation, unexposed people, or storage of supplies or equipment.
The isolation area should be a separate room. However, if an isolation room is not feasible, use a shady area outdoors, or set up a tent outside. If no outside space is available, the corner of one room can be marked off (for example, with rope) and should be at least 2 meters (or 6.5 feet) away from patients not under investigation for EVD. This area must be marked with signs informing other patients and staff that it is an isolation area and only authorized personnel are allowed to enter. A guard should be placed near the entrance/exit to the isolation area, when possible, to prevent unauthorized movement in and out of the area. The guard should also keep a record of all healthcare workers who enter the isolation area and the task or procedure they performed.
Inside the isolation area
- There should be only nonupholstered furniture. A simple bed is best, and if there is room, a chair and table. There should be no upholstered or stuffed material in this room (for example, covered furniture, rugs, mattresses), because these are difficult to disinfect. If there is to be any area for patient sleeping, it must not have a mattress that could absorb infectious fluids; a plastic mattress cover can be used. If the families want to provide bedding, this is acceptable. However, the bedding must be disposed of (burned) after patient leaves (a mattress cover should still be used).
- Two buckets with chlorine solution (one mild [0.05%] and one strong [0.5%]) for disinfection and cleaning should be placed inside the isolation room.
- Feeding utensils, plates, and cups should be clearly marked as only for PUIs. Each patient should use his/her own utensil.
- A latrine pot or commode bucket should be clearly marked for use only by PUIs. If a latrine is not available inside the isolation area, a commode bucket or bedpan should be used.
Only personnel trained and designated for work inside the isolation area should be allowed to enter the isolation area. Extended PPE must be worn at all times in this isolation area. Try to minimize the number of times the isolation area is entered by healthcare workers.
Where to Put on PPE
Outside of the isolation area, there must be a marked off area where PPE can be put on cleanly and carefully. This area needs to have adequate supplies, including all of the following:
- Poster on how to put on PPE
- Handwashing station with mild (0.05%) chlorine solution
- Gowns
- Gloves
- Face shield (goggles and face mask if face shield is unavailable)
- Head cover (optional)
- Apron
- Thick, reusable gloves
Areas for Removing PPE
An area outside the exit of the isolation unit should be marked off for PPE removal. This area should contain the following items:
- Glove-washing station with strong (0.5%) chlorine
- Bucket filled with strong (0.5%) chlorine in which dirty thick reusable gloves, goggles, or aprons will be soaked
- Bucket filled with mild (0.05%) chlorine for rinsing reusable PPE after being soaked
- Container with a lid to hold the infectious burnable waste
- Foot bath filled with strong (0.5%) chlorine
- Handwashing station with mild (0.05%) chlorine just outside the PPE removal area
- A poster illustrating the steps in removing PPE
- Disposable towels
PPE should be removed slowly and carefully under the supervision of a buddy or a trained observer. See guidance on PPE for details.
Separate Toilets or Latrines for PUIs and Patients not Under Investigation for Ebola
It is important that latrines for patients not under investigation and staff be separate from the one that will be used by PUIs. Signs should be placed on the toilets clearly marking who can use which of the facilities.
Waste Management Area
An area of the clinic grounds must be marked off for waste management. All waste from the clinic must be burned in either a burn pit or an incinerator. This place should be on the healthcare facility site, but away from the normal flow of people/cars, and should not be in an area where it will attract people.
- Page last reviewed: January 28, 2015
- Page last updated: December 3, 2014
- Content source:


 ShareCompartir
ShareCompartir