Guidance for Collection, Transport and Submission of Specimens for Ebola Virus Testing
Updated: January 30, 2015
Purpose
To provide guidance for laboratory workers on collecting, transporting and submitting specimens for Ebola virus testing.
Scope
This guidance document replaces the previously posted document: “Interim Guidance for Specimen Collection, Transport, Testing, and Submission for Persons Under Investigation (PUIs) for Ebola Virus Disease (EVD) in the United States.”
This document complements the updated CDC “Guidance for U.S. Laboratories for Managing and Testing Routine Clinical Specimens When There is a Concern About Ebola Virus Disease” which provides guidance for clinical laboratories on testing needed for assessment and care of patients for whom Ebola Virus Disease (EVD) may be a concern, while minimizing risk to laboratory personnel.
This guidance is based on input received from numerous hospital and laboratory directors, infectious disease physicians, CDC Ebola response teams, and state health officials.
Key Points
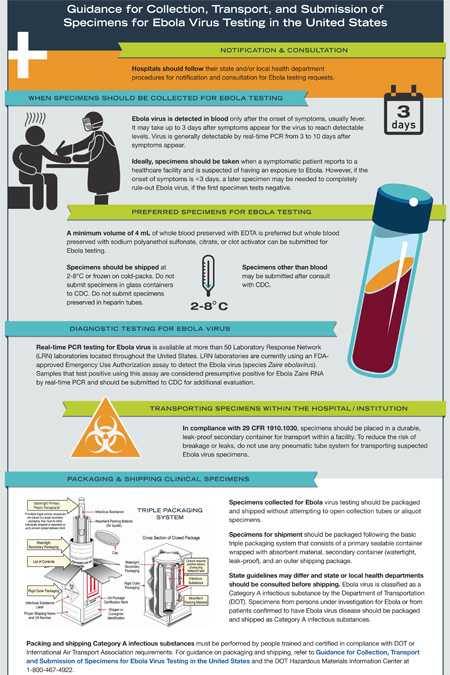
- CDC recommends that Ebola testing be conducted only for persons who meet the criteria for persons under investigation (PUIs) for EVD. A PUI is a person who has both consistent signs and/or symptoms, including:
- Elevated body temperature or subjective fever or symptoms, including severe headache, fatigue, muscle pain, vomiting, diarrhea, abdominal pain, or unexplained hemorrhage, AND
- An epidemiological risk factor within the 21 days preceding the onset of symptoms.
- U.S. hospitals or clinical laboratories concerned about a patient with potential Ebola virus exposure should contact their local and/or state public health authorities. These agencies will work with CDC to determine whether a patient is or is not a PUI, and whether testing is indicated. Patient status should be determined as quickly as possible in order to ensure that patient care is not compromised.
- Presumptive testing for Ebola virus is available at over 50 LRN laboratories located throughout the United States. Any presumptive positive Ebola test result must be confirmed at the CDC to inform public health decisions.
- If it is determined that testing for Ebola virus is indicated, at least 4 mL of whole blood collected in a plastic tube preserved with EDTA is the preferred sample for testing. Specimens should be shipped with refrigerant to maintain 2°–8°C to the designated LRN laboratory.
- If the PUI symptoms have been present for <3 days, a second sample collected 72 hours after onset of symptoms may be required to definitively rule out Ebola.
- To minimize risk to personnel, a site-specific risk assessment must be performed by the laboratory director, safety officer, and other responsible persons prior to receiving specimens in order to determine the potential for exposure from sprays, splashes, or aerosols generated during all laboratory processes, procedures, and activities. Risks should be mitigated by implementing engineering controls, administrative and work practice controls, and use of appropriate personal protective equipment (PPE).
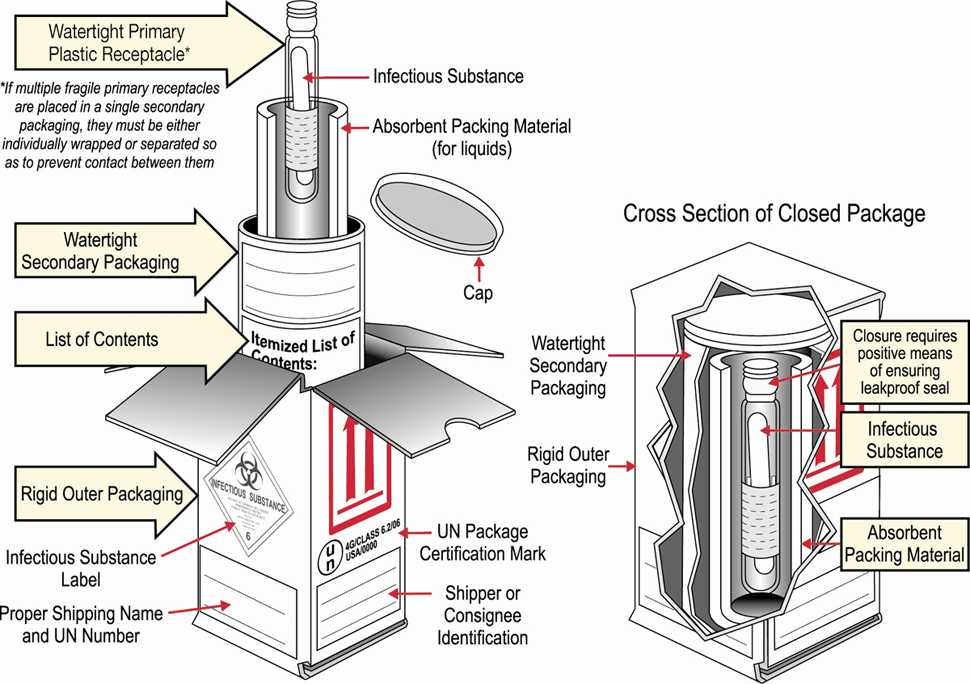
- Ebola virus is classified as a Category A infectious substance by the Department of Transportation (DOT) and transport of samples from PUIs or patients confirmed or suspected of having EVD is regulated by DOT’s Hazardous Materials Regulations (HMR) 49 CFR 171-180. Specimens for shipment should be packaged following the basic triple packaging system consisting of (1) a primary container (a sealable specimen container) wrapped with absorbent material, (2) a secondary container (watertight, leak-proof), and (3) an outer shipping package.
- The United States Occupational Safety and Health Administration (OSHA) Bloodborne Pathogens Standard (29 CFR 1910.1030) was developed to reduce the potential exposure of personnel to bloodborne pathogens. All U.S. laboratories handling patient specimens are required to comply with this standard at all times; strict adherence is an initial step in providing protection to personnel.
Background
Ebola virus can cause a severe, often fatal disease in humans and nonhuman primates. It is transmitted through contact with infected blood or body fluids (e.g., urine, stool, and vomit) and with objects such as needles that have been contaminated with infected body fluids. The incubation period is usually 8–10 days (ranging from 2 to 21 days). Patients can transmit Ebola virus once symptoms appear and through the later stages of disease, as well as postmortem. PUIs should be managed by following appropriate precautions to prevent transmission of Ebola virus to others and the hospital environment; for guidance on infection control, see CDC infection control guidance.
Diagnosing Ebola in a person who has been infected for only a few days may be complicated. The early symptoms of Ebola infection are difficult to distinguish from other, more common infectious diseases such as such as malaria, influenza, and typhoid fever. Ebola virus is detected in blood only after onset of symptoms, most notably fever, which accompany the rise in circulating virus; however, it may take up to 3 days after symptoms begin for the virus to reach detectable levels.
CDC recommends that Ebola testing be conducted only for persons who meet the criteria for persons under investigation (PUIs) for Ebola virus disease. Presumptive Ebola testing is available at over 50 LRN laboratories and confirmatory Ebola testing is available at the CDC. U.S. hospitals or clinical laboratories concerned about a patient with potential Ebola virus exposure should contact their local and state public health authorities before contacting CDC. In joint consultation with CDC (770-488-7100), these agencies will assist in determining whether testing is indicated. No specimens will be accepted by CDC laboratories without prior consultation with CDC.
Collecting Specimens for Ebola Testing
- Specimens should be obtained when a patient meets the criteria for person under investigation (PUI) including patients with clinical signs, symptoms, and epidemiologic risk factors for Ebola virus disease. If the first specimen is obtained 1-3 days after the onset of symptoms and tests negative and the patient remains symptomatic without another diagnosis, a later specimen may be needed to rule-out Ebola virus infection.
- Staff who collect specimens from PUIs should wear appropriate PPE and should refer to Guidance on Personal Protective Equipment To Be Used by Healthcare Workers During Management of Patients with Ebola Virus in U.S. Hospitals, Including Procedures for Putting On (Donning) and Removing (Doffing).
- For adults, a minimum volume of 4 mL whole blood is preferable. For pediatric samples, a minimum of 1 mL whole blood should be collected in pediatric-sized collection tubes. Blood must be collected in plastic collection tubes. Do not transport or ship specimens in glass containers or in heparinized tubes.
- Whole blood preserved with EDTA is preferred, but whole blood preserved with sodium polyanethol sulfonate, citrate or with clot activator is also acceptable.
- Do not separate and remove serum or plasma from the primary collection container.
- Specimens should be packaged and transported at 2°–8°C with cold-packs to the final testing destination.
- Specimens other than blood may be submitted after consultation with CDC by calling the EOC at 770-488-7100.
Storing Clinical Specimens for Ebola Testing
If necessary, short-term storage of specimens before shipping should be at 4°C or frozen.
Diagnostic Testing for Ebola Virus
Real-time PCR testing for Ebola virus is available at over 50 LRN laboratories located throughout the United States. LRN laboratories are currently using an FDA approved Emergency Use Only (EUA) assay to detect the Ebola (Zaire species) virus. Samples that test positive using this assay are considered presumptive positive for Ebola Zaire RNA by real time RT-PCR and should be submitted to CDC for additional evaluation.
Transporting Specimens within the Facility
- PPE to be worn during transport within the facility should be determined by a site-specific risk assessment, and may vary among facilities. Recommendations for PPE include disposable fluid-resistant closed lab coat, disposable gloves, covered legs and closed-toed shoes.
- Before removing patient specimens from the site of care, it is advisable to plan the route of the sample from the patient area to the location where it will be packed for shipping in order to avoid high traffic areas.
- Before removing patient specimens from the site of care, the outside of the specimen containers should be decontaminated with an approved disinfectant as described in Interim Guidance for Environmental Infection Control in Hospitals for Ebola Virus.
Note: Recommended disinfectants are those known to kill non-enveloped viruses and can be found in List L of EPA's Disinfectants for Use Against the Ebola Virus. This list of registered disinfectants meets the CDC’s criteria for use against the Ebola virus on hard, non-porous surfaces.
- In compliance with OSHA Bloodborne Pathogens Standard (29 CFR 1910.1030), specimens should be placed in a durable, leak-proof secondary container.
- After placing in a secondary container, specimens should be hand-carried to the laboratory or packing area. DO NOT use any pneumatic tube system (automated or vacuum specimen delivery system) for transporting specimens.
Transporting Specimens for Ebola Testing to Sites Outside the Facility
- Samples from patients that are suspected of or confirmed to have Ebola virus infection should be packaged and shipped as Category A infectious substances in accordance with the DOT’s Hazardous Materials Regulations (HMR) 49 CFR 171-180.
- All persons packing and shipping infectious substances must be trained and certified in compliance with DOT or the International Air Transport Association (IATA) requirements every two years.
- Specimens collected for Ebola virus testing should be packed and shipped without attempting to open collection tubes or aliquot specimens. Opening the tubes destroys the vacuum seal and thus increases the risk of leakage during transport.
- Specimens for shipment should be packaged following the basic triple packaging system, which consists of (1) a primary container (a sealable specimen container) wrapped with absorbent material, (2) a secondary container (watertight, leak-proof), and (3) an outer shipping package. For questions about (packaging) transportation regulations, contact the U.S. DOT Hazardous Materials Information Center at 1-800-467-4922.
Packing and Shipping Clinical Specimens for Confirmation at CDC
The following steps should be followed by persons certified to ship infectious substances.
- Because guidelines may vary state to state, contact your state and/or local health department prior to shipping.
- Email tracking number to EOCEVENT246@CDC.GOV
- Do not ship for weekend delivery unless instructed to do so by CDC.
- Ship to:
Centers for Disease Control and Prevention
ATTN STAT LAB: VSPB, UNIT #70
1600 Clifton Road NE
Atlanta, GA 30333
Phone 770-488-7100
- Include the following information inside the package: your name, the patient's name, test(s) requested, date of collection, laboratory or accession number, and CDC Form 50.34 [PDF – 1 page] and Viral Special Pathogens Branch specimen submission forms [PDF – 2 pages].
- On the outside of the box, specify how the specimen should be stored: refrigerated.
- Include documentation required by DOT or IATA.
Occupational Health
Potential exposures to blood, body fluids, and other infectious materials must be reported immediately according to your institution’s policies and procedures.
When to Contact CDC
Hospitals should contact their state and/or local health department before contacting CDC. CDC is available for consultation at 770-488-7100.
CDC will continue to evaluate new information as it becomes available and will update this guidance as needed.
Additional Resources and Information
- Instructions for Submitting Diagnostic Specimens to CDC’s Viral Special Pathogens Branch
- Viral Special Pathogens Branch Specimen Submission Information [PDF – 2 pages]
- Infection Prevention and Control Recommendations for Hospitalized Patients with Known or Suspected Ebola Virus Disease in U.S. Hospitals
- HAN 364: Guidelines for Evaluation of US Patients Suspected of Having Ebola Virus Disease
- Guidelines for Disinfection and Sterilization in Healthcare Facilities, 2008
- Guidelines for Safe Work Practices in Human and Animal Medical Diagnostic Laboratories [PDF – 105 pages]
- Submitting Specimens to CDC Specimen Submission Form
- Page last reviewed: February 5, 2015
- Page last updated: February 5, 2015
- Content source:


 ShareCompartir
ShareCompartir