Information for Health Care Providers and Public Health Professionals: Preventing Tobacco Use During Pregnancy
On this Page
- What are the health effects of tobacco use on pregnancy?
- What is the prevalence of smoking before, during, and after pregnancy?
- Prevalence of smoking during the last 3 months of pregnancy by demographic characteristics, 24 PRAMS states, 2011
- Prevalence of smoking during the last 3 months of pregnancy by insurance status and prenatal care initiation, 24 PRAMS states, 2011.
- Trends of smoking before pregnancy, during pregnancy, and after delivery, 9 PRAMS states, 2000–2011
- What about products that don’t burn, like electronic cigarettes and smokeless tobacco?
- What works to help pregnant women quit smoking?
- What about cutting back the number of cigarettes smoked without quitting?
- What can be done?
What are the health effects of tobacco use on pregnancy?
Smoking during pregnancy remains one of the most common preventable causes of pregnancy complications illness, and death among infants. Women who quit smoking before or during pregnancy reduce their risk for poor pregnancy outcomes.
Compared with nonsmokers, women who smoke before pregnancy are about twice as likely to experience the following conditions:
- Delay in conception.
- Infertility.
- Ectopic pregnancy.
- Premature rupture of the membranes.
- Placental abruption.
- Placenta previa.
Compared with babies born to nonsmokers, babies born to women who smoke during pregnancy are more likely to have one of the following conditions:
- Premature birth.
- Low birth weight.
- Small for gestational age or fetal growth restricted.
- Born with a cleft lip, or cleft palate.
- Higher risks of SIDS (Sudden Infant Death Syndrome).
All tobacco products that are burned contain nicotine and carbon monoxide. These are harmful during pregnancy. These products include cigarettes, little cigars, cigarillos, and hookah.
What is the prevalence of smoking before, during, and after pregnancy?
CDC’s Pregnancy Risk Assessment Monitoring System (PRAMS) monitors the prevalence of smoking before, during, and after pregnancy based on a mother’s self-report. In 2011, data from 24 states (representing about 40% of US live births) showed
 Before pregnancy
Before pregnancy
- About 23% of women smoked during the 3 months before pregnancy.
During pregnancy
- About 10% of women smoked during the last 3 months of pregnancy.
- Groups who reported the highest prevalence of smoking during pregnancy included (Figure 1)
- American Indians/Alaska Natives.
- Those younger than 25 years of age.
- Those with 12 years of education or less.
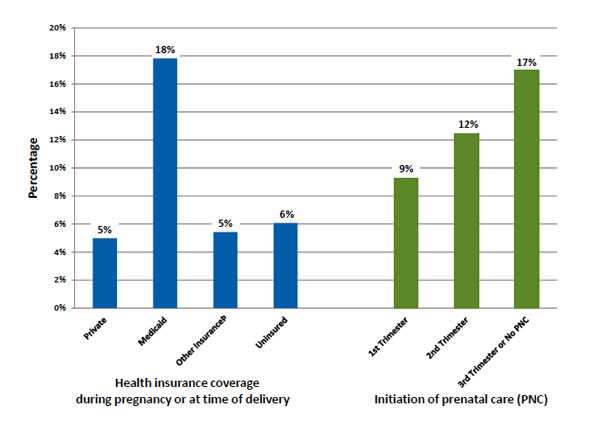
- Women enrolled in Medicaid were three times more likely to smoke than women with private insurance (Figure 2).
- About 55% of women who smoked before pregnancy reported they quit smoking by the last 3 months of pregnancy.
After pregnancy
- Of those who quit smoking during pregnancy, 40% relapsed within 6 months after delivery.
Figure 1. Prevalence of smoking during the last 3 months of pregnancy by demographic characteristics, 24 PRAMS states, 2011.
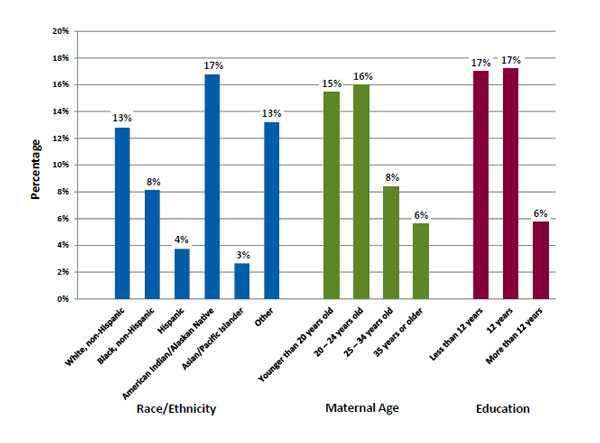
Figure 2. Prevalence of smoking during the last 3 months of pregnancy by insurance status and prenatal care initiation, 24 PRAMS states, 2011.
Trends from 2000–2011 (data from 9 states)
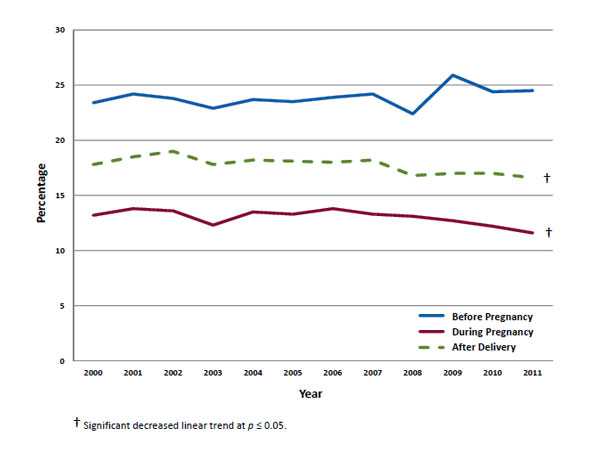
- The prevalence of smoking in the 3 months before pregnancy did not change (Figure 3). About 1 of 4 women smoked before pregnancy.
- The prevalence of smoking declined in the last 3 months of pregnancy (13.2% to 11.6%) and after delivery (17.8% to 16.6%).
Figure 3. Trends of smoking before pregnancy, during pregnancy, and after delivery, 9 PRAMS states, 2000–2011.
What about products that don’t burn, like electronic cigarettes and smokeless tobacco?
Women may perceive tobacco products that don’t burn to be safer than smoking cigarettes. In addition, the use of electronic cigarettes—also referred to as e-pens, e-hookah, tanks, or vape pens—is increasing rapidly among youth and adults.
- All tobacco products contain nicotine, which is a reproductive toxicant and has adverse effects on fetal brain development.
- Pregnant women and women of reproductive age should be cautioned about the use of nicotine-containing products, such as electronic cigarettes, as alternatives to smoking. The health effects of using electronic cigarettes before or during pregnancy have not been studied.
- Electronic cigarettes are not regulated and have not been shown to be a safe and effective cessation aid in smokers.
- The use of smokeless tobacco products, such as snus, during pregnancy has been associated with preterm delivery, stillbirth, and infant apnea.
- There are a number of FDA-approved cessation products, including nicotine replacement therapies (NRT), that are available for the general population of smokers to use to reduce their dependence on nicotine.
- Pregnant women who haven’t been able to quit smoking on their own or with counseling can discuss the risks and benefits of using cessation products, such as NRT, with their health care provider.
For more information, see Q&A about Electronic Nicotine Delivery Systems for Providers Caring for Pregnant Women.
What works to help pregnant women quit smoking?
Counseling by health care providers
 The majority of pregnant women receive prenatal care. Prenatal care visits provide a valuable opportunity to address women’s smoking behavior.
The majority of pregnant women receive prenatal care. Prenatal care visits provide a valuable opportunity to address women’s smoking behavior.
- Pregnancy-specific counseling (e.g., counseling based on the 5A’s model) increases smoking cessation in pregnant women. Steps of the 5A’s include the following:
- Ask the patient about smoking status at first prenatal visit and follow up at subsequent visits.
- Advise the patient to quit.
- Assess the patient’s willingness to quit.
- Assist the patient by providing resources.
- Arrange follow-up visits to track the progress of the patient’s attempt to quit.
- If women are unable to quit on their own or with counseling, ACOG (American College of Obstetricians and Gynecologists) recommends that nicotine replacement therapies be considered under the close supervision of a provider.
- Quitlines can be used to support pregnant smokers in their goal to quit. Quitline counseling is available in every state, easy to use, and generally provided at no cost to the user.
- Health care system changes, such as provider reminders and documentation of smoking status and cessation intervention, can increase the number of patients who quit.
Population-based interventions
State and community tobacco control interventions that promote tobacco cessation, prevent tobacco initiation, and reduce secondhand smoke not only reduce smoking prevalence in the general population, but also decrease prevalence in pregnant women.
- A $1.00 increase in cigarette taxes increased quit rates among pregnant women by 5 percentage points. Higher cigarette prices also reduced the number of women who start smoking again after delivery.
- Full smoking bans in private work sites can increase the number of women who quit during pregnancy by about 5 percentage points.
- Expanded Medicaid tobacco-cessation coverage increased quitting by almost 2 percentage points in women who smoked before pregnancy.
What about cutting back the number of cigarettes smoked without quitting?
Pregnant women should be advised that complete cessation has the most health benefits by far, and any amount of smoking can be harmful to the fetus. Studies support that cutting down without quitting before the third trimester of pregnancy may improve fetal growth. However, smoking has many other health effects and the potential benefits of simply reducing the number of cigarettes smoked without quitting should be weighed against the following:
- Nicotine is a reproductive toxicant and smoking has been found to contribute to adverse health effects on pregnancy including preterm birth and stillbirth.
- Nicotine has lasting adverse effects on fetal brain development.
- Nicotine is believed to affect fetal lung development and contributes to the risk of SIDS.
- Smoking most likely affects fetal growth through products of combustion, such as carbon monoxide (CO). There are more than 7,000 other chemicals in tobacco smoke, many of which could also affect fetal health.
- Fetal growth cannot be viewed as a measure of other health effects. It is unknown whether reducing the number of cigarettes smoked improves outcomes other than fetal growth.
CDC Tips from Former Smokers
- Watch or read real stories from mothers who quit smoking or whose children are affected by tobacco smoke
- Amanda tried hard to quit smoking while she was pregnant, but she was unable to overcome her addiction to cigarettes.
- Beatrice is a mother of two boys. She has no health problems but quit smoking with support from friends and family.
- Tiffany quit smoking because her mother died of cancer when Tiffany was 16. She could not bear the idea of missing out on her own daughter’s life.
- Jessica never smoked but her son has severe asthma triggered by secondhand smoke exposure.
What can be done?
Doctors, midwives, nurses, and other health care providers can
- Ask all pregnant women about their tobacco use (cigarettes, cigars, little cigars, cigarillos, hookah, smokeless, and electronic cigarettes) and provide nonjudgmental support for women who want to quit. An interactive Web-based program teaches best-practice approaches to help pregnant smokers and women of reproductive age to quit. This program is endorsed by CDC and American Congress of Obstetricians and Gynecologists (ACOG) and is available for continuing education credits.
- Refer pregnant women to their state quitline, 1-800-QUIT-NOW (1-800-784-8669). Quitlines provide special services and counseling for pregnant and postpartum women. Follow up with pregnant women to make sure they have initiated counseling.
- Share and use resources from the CDC Tips from Former Smokers campaign such as posters, videos, and factsheets.
Public health professionals can
- Link health systems and organizations that serve women who are at high risk for smoking during pregnancy with available resources. An interactive Web-based program teaches best-practice approaches to help pregnant smokers and women of reproductive age to quit.
- Educate providers and pregnant women on tobacco cessation coverage benefits and services available in your state. As of October 2010, states are to provide tobacco cessation counseling and medication without cost sharing for pregnant Medicaid beneficiaries.
- Monitor your state’s prenatal smoking prevalence by using CDC's PRAMStat.
Women can
- Quit smoking before you get pregnant, which is best.
- If you are pregnant, quit smoking to help reduce your and your baby’s risk of health problems. It's never too late to quit smoking. Don’t start smoking again after your baby is born. Find tips on quitting smoking.
- Talk with your doctor, nurse, or health care professional about quitting. For additional support, call the quitline at 1-800-QUIT-NOW (1-800-784-8669). The quitline provides special resources for pregnant women.
- Watch or read real stories from mothers who quit smoking or whose children are affected by tobacco smoke.
- Learn more online about the effects of smoking and health risks of smoking.
Family and friends can
- Be supportive and nonjudgmental.
- If you smoke, don’t smoke around the expecting mother. Better yet, show your support and quit smoking yourself. It will benefit your health as well as hers.
- Let the expecting mother know about support from the quitline 1-800-QUIT-NOW (1-800-784-8669). The quitline provides special resources for pregnant women.
- Tell her about real stories from mothers who quit smoking or whose children are affected by tobacco smoke.
- Learn more online about the effects of smoking and health risks of smoking.
- Page last reviewed: July 20, 2016
- Page last updated: August 5, 2016
- Content source:





 ShareCompartir
ShareCompartir