HIV and Injection Drug Use
Syringe Services Programs for HIV Prevention
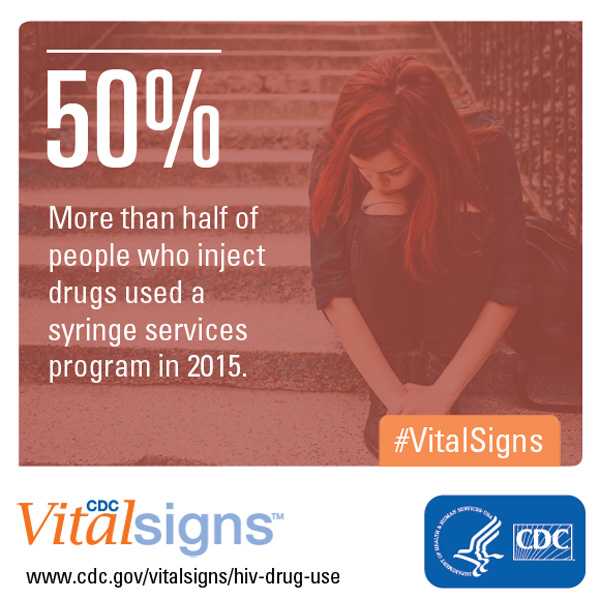
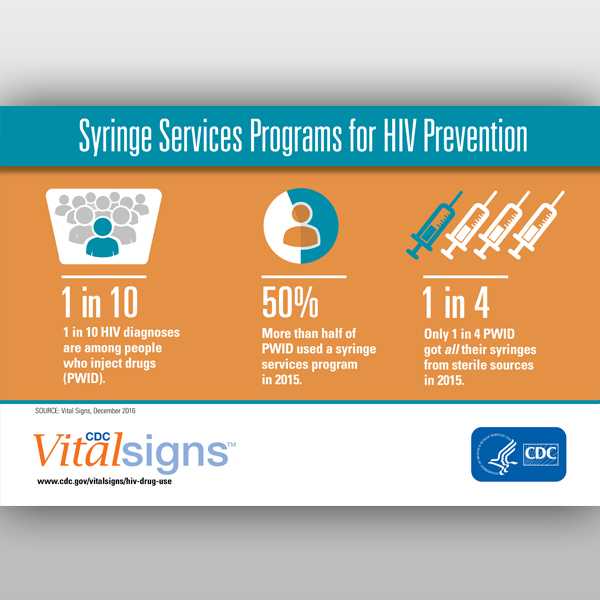
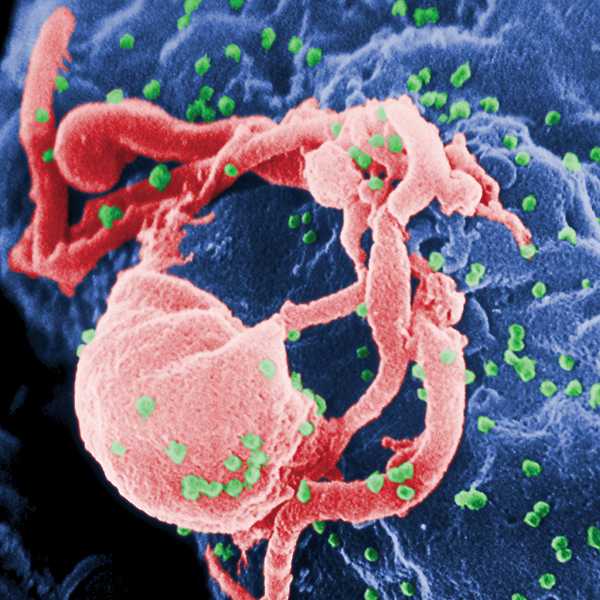
Use of syringe services programs (SSPs) has increased substantially during the past decade, but most people who inject drugs still don’t always use sterile needles, according to a new CDC Vital Signs report published today. Sharing needles and syringes is a direct route of transmission for HIV and hepatitis B and C viruses.
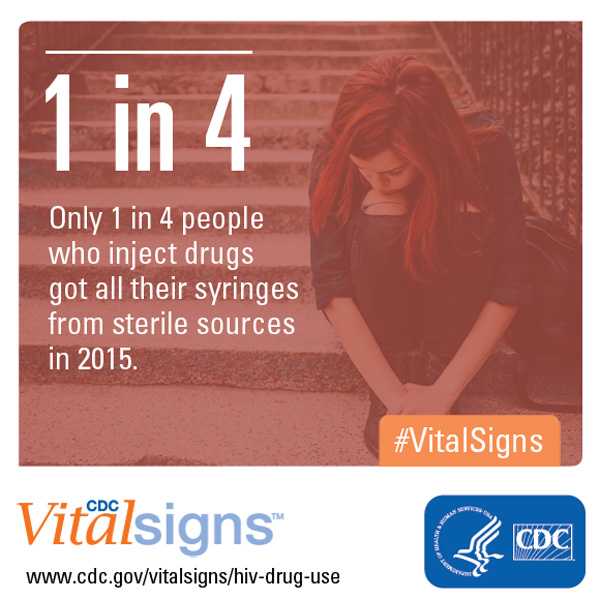
The analysis finds that more than half (54%) of people who inject drugs reported in 2015 they used an SSP in the past year, compared to only about one-third (36%) in 2005. The finding is from a study of people who inject drugs in 22 U.S. cities with a high number of HIV cases. Although SSP use has increased, findings indicate that too few people who inject drugs use only sterile needles. One in three (33%) reported in 2015 that they had shared a needle within the past year – about the same percentage that reported sharing a decade ago (36% in 2005).
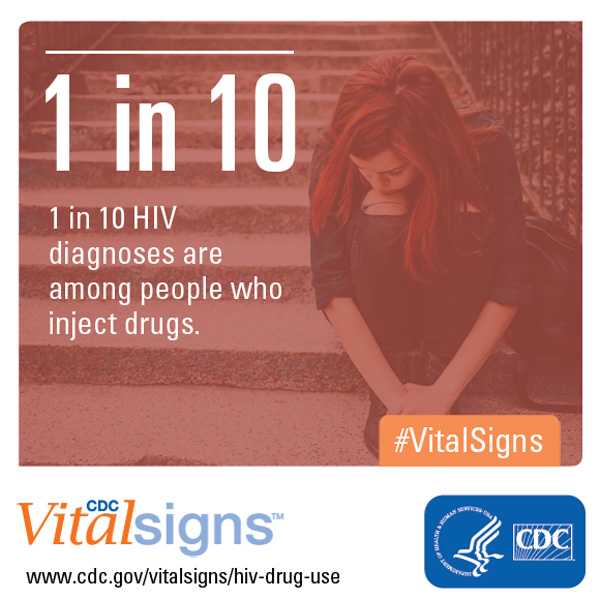
Approximately 9% of HIV infections diagnosed in the United States each year are among people who inject drugs. In recent years, injection drug use has also contributed to a 150% increase in acute cases of hepatitis C infections.
Nationally, HIV diagnoses were cut by nearly half (48%) among people who inject drugs from 2008 to 2014, according to previous CDC analyses. Despite that decline, this Vital Signs report suggests an unmet need persists for sterile injecting equipment – and that many people who inject drugs risk transmitting HIV, hepatitis C, and other infections. The risk may be even higher in rural areas where access to sterile injection equipment may be more limited and in urban and suburban areas where SSPs are restricted or not allowed.
Decisions about implementing SSPs are made at state and local levels, and access to comprehensive SSPs varies across the country. CDC has historically recommended that states ensure people who inject drugs have access to effective prevention services, including sterile injection equipment, medication-assisted treatment for substance use disorder, and HIV and hepatitis testing. In December 2015, Congress gave states and local communities, under some circumstances, the opportunity to use federal funds to support certain components of comprehensive SSPs.
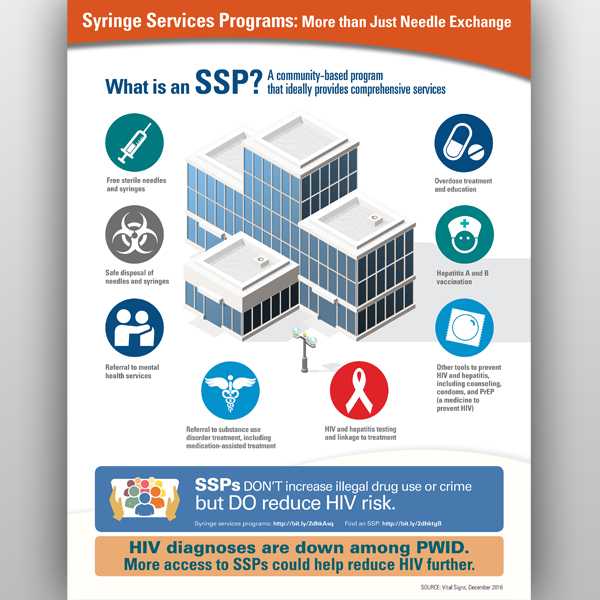
Comprehensive SSPs provide sterile needles and syringes and offer or refer people who inject drugs to prevention, care and treatment services. Those include HIV and hepatitis C testing and treatment, as well as other HIV prevention options like condoms, behavioral interventions, and pre-exposure prophylaxis (PrEP, a daily pill that can prevent HIV). Comprehensive SSPs also offer or refer people to substance use disorder treatment – including medication-assisted treatment – to help stop drug use and prevent HIV and hepatitis infection. They can also provide overdose treatment.
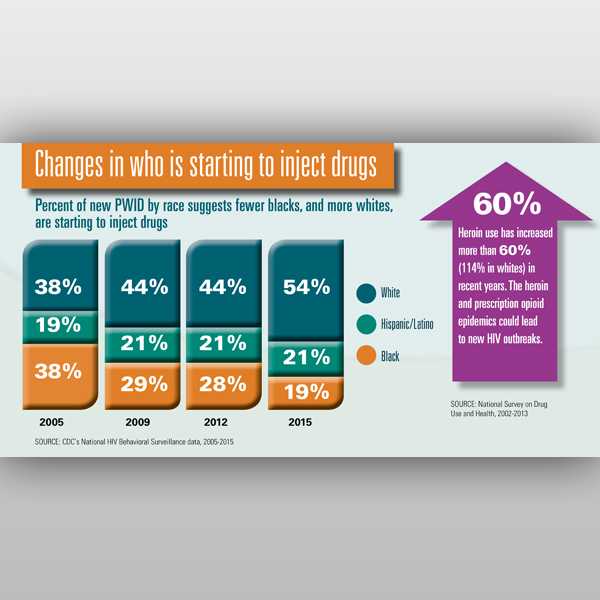
Today’s report highlights some successes in HIV prevention among African Americans and Latinos who inject drugs in 22 cities and nationally. It also found worrying trends in whites who inject drugs.
African Americans who inject drugs
- The percentage of African Americans who inject drugs who reported getting all syringes from a sterile source increased by 48%; the percentage who reported syringe sharing declined by 34% from 2005 to 2015 among the cities studied.
- Nationally, the number of HIV diagnoses among African Americans who inject drugs declined by approximately 50% from 2008 to 2014.
Latinos who inject drugs
- The percentage of Latinos who inject drugs who reported syringe sharing declined by 12% from 2005 to 2015.
- Nationally, the number of HIV diagnoses among Latinos who inject drugs declined by approximately 50% from 2008 to 2014.
Whites who inject drugs
- High levels of sharing continued among whites who inject drugs, with 45% reporting sharing in 2005 and 43% reporting sharing in 2015.
- The percentage of whites who inject drugs who reported receiving all syringes from sterile sources remained unchanged at 22% over the decade among the cities studied.
- Nationally, HIV diagnoses among whites who inject drugs declined by approximately 27% from 2008 to 2014, but have remained stable from 2012 to 2014.
About this Vital Signs Analysis
Behavioral risk analyses are based on data from CDC’s National HIV Behavioral Surveillance system, which has been monitoring HIV risk behavior among people who inject drugs since 2005. While not nationally representative, the data are collected from people who inject drugs in 22 large cities where approximately half of the nation’s HIV cases are diagnosed. Diagnoses data are based on CDC’s National HIV Surveillance System and are nationally representative.
Contact Information
CDC Media Relations
(404) 639-3286
media@cdc.gov
Vital Signs Links
Factsheet:
English [1.9MB]
Spanish [2.39MB]
Spokespersons
Jonathan Mermin, MD, MPH
“Until now, the nation has made substantial progress in preventing HIV among people who inject drugs, but this success is threatened,” said Jonathan Mermin, MD, MPH, director of CDC’s National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention. “Syringe services programs work, and their expansion is pivotal for progress in the coming decades.”
Jonathan Mermin, MD, MPH – Director, CDC’s National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention
Eugene McCray, MD

“It is encouraging to see prevention efforts paying off in African-American and Latino communities,” said Eugene McCray, MD, director of CDC’s Division of HIV/AIDS Prevention. “We must now take concrete steps that build upon and accelerate that progress. HIV risk remains too high for all people who inject drugs.”
Eugene McCray, MD – Director, CDC’s Division of HIV/AIDS Prevention
Related Links
- Press Release: Use of syringe services programs increases, but access must improve for greater HIV prevention – English | Spanish
- MMWR – Vital Signs: Trends in HIV Diagnoses, Risk Behaviors, and Prevention Among Persons Who Inject Drugs — United States
- Vital Signs: Home | December 2016 Vital Signs | Fact Sheet PDF 1.9 MB | Topics
- Vital Signs: (Spanish) Home | 2016 Diciembre – Signos Vitales | Fact Sheet PDF 2.39MB | Topics
- CDC Program Guidance for Implementing Certain Components of Syringe Services Programs, 2016
- CDC Consultations on Determination of SSP Need Requests
- CDC Statement on Syringe Services Programs, Dec. 21, 2015
- County-Level Vulnerability Assessment for Rapid Dissemination of HIV or HCV Infections Among Persons Who Inject Drugs, United States
Podcast
- Vital Signs – HIV and Injection Drug Use – English | Spanish
- Vital Signs – HIV and Injection Drug Use – [PSA – 0:60 seconds]
- Page last reviewed: November 29, 2016
- Page last updated: November 29, 2016
- Content source:



 ShareCompartir
ShareCompartir