Strong Labs Save Lives

More than a decade ago, the U.S. Government launched the President’s Emergency Plan for AIDS Relief (PEPFAR) to help bring lifesaving treatment to as many people as possible in sub-Saharan Africa – the epicenter of the world’s AIDS crisis. But as treatment efforts expanded, it became increasingly clear that weak laboratory systems were undermining efforts to effectively fight the disease across the continent. Although often neglected, strong laboratories are at the core of any country’s ability to prevent, identify, and respond to HIV, TB, and other diseases.
To tackle this major health challenge, in 2007 the U.S. Centers for Disease Control (CDC), PEPFAR, and Becton Dickinson (BD) joined forces with Ministries of Health in four African countries. The results of this innovative partnership, known as Labs for Life, were featured in the April 2016 of the Journal of Infectious Diseases. The partnership focused on Kenya, Mozambique, Ethiopia, and Uganda – countries with some of the highest rates of HIV and TB in the world

“One of the most remarkable outcomes of the CDC, PEPFAR and Becton Dickinson (BD) partnership was the reduction in transport time for TB testing from twelve days to two days. Results like that inspire trust in test results, confidence in clinicians and underscores the fact that strong labs save lives.”
-Dr. John Nkengasong, Chief of DGHT’s International Laboratory Branch

KENYA
Frontline Healthcare workers: Our Greatest Asset in the Fight against HIV
In the early 2000’s with the HIV epidemic at its height, the global community pushed to get those in need access to essential medicine to treat the disease. However, without adequate labs to accurately diagnose and track the disease, frontline healthcare workers didn’t have a chance of winning the fight against this deadly disease. Nowhere was this truer than in Kenya: a nation where high HIV prevalence rates (5.6 percent) meant even greater risk to patients and healthcare workers.
A false positive or negative blood result could mean a delay in much needed treatment or worse, the spread of diseases like hepatitis or HIV. Baseline studies conducted in Kenya before the launch of the CDC, PEPFAR and BD partnership showed none of the 194 observed blood draws met safety and quality standards. As part of the partnership, healthcare workers were trained to safely draw blood increasing their knowledge by 41 percent and resulting in fewer misdiagnosis, higher quality lab results and quicker treatment.
The partnership, which equipped frontline healthcare workers with the skills they need to protect themselves and their patients from injury and disease, is also saving lives -- particularly for the most vulnerable of patients like HIV- exposed infants where delays in treatment can lead to early death. But the partnership didn’t stop there, it also established a Center for Excellence at Kenya Medical Training College to ensure the continuation of training and sustain these results for years to come.
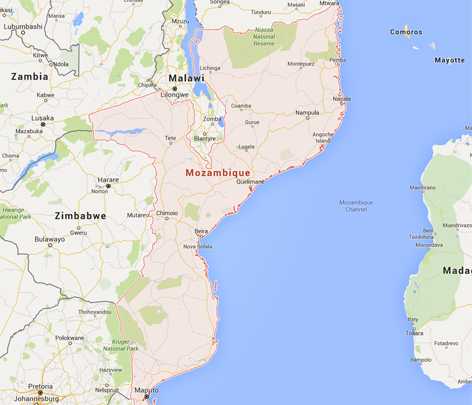
MOZAMBIQUE
Transforming Policy: The key to lasting change
In Mozambique, a southern African nation that sits on the coast of the Indian Ocean, over half of the nation’s population lives on less than $2 USD per day and the average life expectancy is just 55 (source: The World Bank). In 2010, when CDC, PEPFAR and BD launched the Labs for Life partnership to strengthen labs across the country, the national healthcare system was already crippled from a 15-year civil war. Facing these incredible challenges, the team knew it would need to take a different approach to have lasting impact.
Despite a lack of resources, the Mozambique Ministry of Health (MOH) was committed to delivering quality lab services to their citizens. Under the ministry of health’s leadership, the partnership focused on standardizing and improving the accuracy of labs across the country resulting in up to a three-fold increase in lab quality. These powerful results were then used to advocate for institutionalizing these changes across the country and building the capacity of MOH staff to audit and manage lab quality on a national scale. The MOH now had the strategy, tools and expertise to successfully deliver on their promise of an improved lab network for their citizens.

ETHIOPIA
Delivering Change: How Postal Workers in Ethiopia are Fighting HIV one Package at a Time
Postal workers probably aren’t the first thing that comes to mind when most people think of the response to HIV and TB throughout Africa. But in Ethiopia, a country where the HIV epidemic exposed a fragile lab network, that is exactly where experts from CDC, PEPFAR and BD knew they needed to start. In a country where timely lab results for HIV and TB testing and diagnosis are essential to getting people on life saving medicine – they knew lasting results in the fight against HIV couldn’t be achieved without addressing the weakest link in the healthcare system- the nation’s lab network.
In partnership with the Ethiopia Ministry of Health (MOH), Labs for Life started by addressing key gaps in the lab supply chain including reducing turnaround times and increasing access to lab services. The work unveiled another crucial gap - there was no standard way to transport lab specimens. In fact, lab workers were often leaving work or shutting down labs to take specimens for testing. A custom designed course for postal and lab workers on proper packaging and handling of lab samples was developed. A standardized network through the Ethiopian postal service was created to transport and track lab specimens from clinics to labs via GPS. This resulted in reduced turnaround times for lab results by 50 percent in the Amhara region and an astounding 71 percent in Addis Ababa.
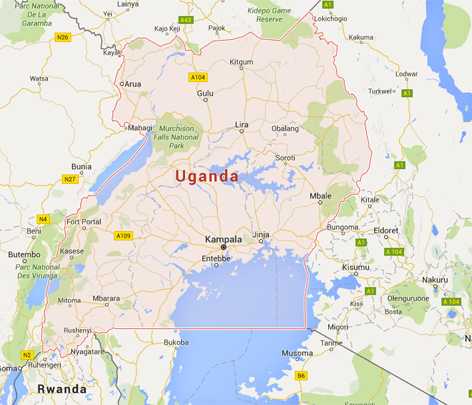
UGANDA
Two Epidemics: One Mission.
Because HIV and TB often go hand in hand, CDC is tackling these two epidemics together through the CDC, PEPFAR and BD partnership in Uganda to have the g reatest impact. Rapid diagnosis in patients that are co-infected with HIV and TB is critical to saving lives, but unfortunately in many parts of the world broken or missing labs and transport systems can mean many patients don’t get essential tests for multidrug-resistant tuberculosis (MDR-TB) or wait up to 5 months to receive results. Uganda was no exception. With no standardized way to collect or transport lab specimens, samples were often collected ad hoc and sometimes only transported to labs when a staff member was traveling to the capital city.
The CDC, PEPFAR and BD partnership, known as Labs for Life, focused on strengthening the transport system of TB specimens and training healthcare workers to accurately diagnose TB so patients could start treatment faster. Over 700 people in 80 districts were trained in standardized processes for handling and transporting lab samples. After four years, there was an eight-fold increase in the number of referrals of patients with suspected MDR-TB. TB specimens were arriving 83 percent faster for testing and 94 percent of specimens reached national labs within the targeted 3-day window as opposed to just 9 percent prior to the program. By working smarter together and combining the skills and resources of governments and the private sector the partnership is fighting these two deadly epidemics together.
Resources
To learn more about this innovative public private partnership to transform laboratory systems throughout Africa, CDC’s Division of Global HIV and TB offers the following resources:
Find us on social media to share our messages:
- Page last reviewed: October 27, 2016
- Page last updated: October 27, 2016
- Content source:


 ShareCompartir
ShareCompartir








