Cervical Cancer Carcinogenesis
Most cervical cancer cases are attributed to HPV infection. However, HPV infection alone is not always enough to cause cervical cancer. For more information about additional causes of cervical cancer, please refer to the cervical cancer module within this curriculum.
HPV infection occurs with a break in the epithelium so that HPV can attach to and infect basal cells, typically in the cervical transformation zone.
HPV infection is usually transient, particularly in women younger than 30 years of age. Most infections (91%) clear within 3 years. The median duration of infection is 8 months for high-risk HPV types. The longer a high-risk HPV infection persists, the greater the risk of precancer.
The stages of cervical cancer carcinogenesis include (Figure 1)—
- HPV infection.
- Persistence, rather than clearance of the virus.
- Development of a high-grade precursor lesion or “precancer.”
- Invasion.
Below is a graphical representation of HPV’s role in cervical cancer carcinogenesis, with images of classical cytological and colposcopic findings of a normal cervix, an HPV-infected cervix, precancer, and cancer.
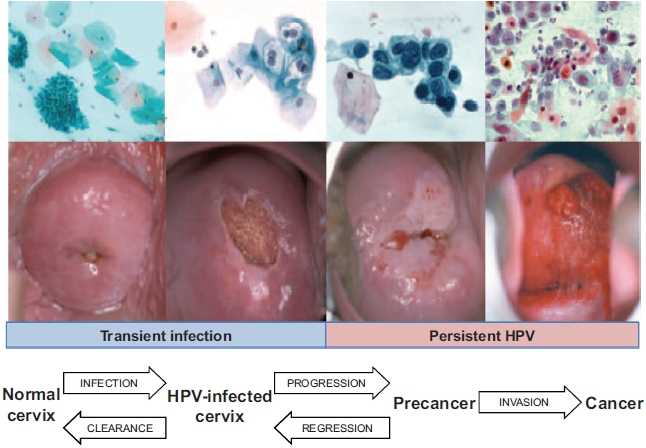
Figure 1: Stages of Cervical Cancer Carcinogenesis
Reprinted with permission from Schiffman M, Wentzensen N. From human papillomavirus to cervical cancer. Obstetrics and Gynecology 2010;116(1):177–185.
In most women, there is a 10- to 20-year gap between HPV infection and cancer development, underscoring the complexity of cancer development. Clearance of the virus can occur at all pre-cancer stages, with decreasing clearance rates at each progressive stage.
HPV is also linked to other cancers (vagina, vulva, penis, anus, and oropharynx).
Terminology
In the past, the terms “atypical squamous cells of undetermined significance” (ASCUS), “low-grade squamous intraepithelial lesion” (LSIL), and “high-grade squamous intraepithelial lesion” (HSIL) were used for cytology, and cervical intraepithelial neoplasia (CIN) 1, 2, and 3 were used for histology. Now these terms have been synchronized so that LSIL (corresponding to the older term CIN 1) and HSIL (corresponding to CIN 2 or CIN 3) are used for both cytology and histology. Some pathologists will categorize HSIL into CIN 2 or CIN 3, but more often these are no longer reported as separate diagnoses. Throughout this module, the terms CIN 2 or 3 will sometimes be used, particularly when referring to study findings when those were the appropriate terms.
Knowledge Check
Answer the question on your own and check your answer.
Can you name the cancers associated with HPV infection? 
Answer: cervical, vaginal, vulvar, penile, anal, and oropharyngeal.
- Page last reviewed: August 27, 2015
- Page last updated: August 27, 2015
- Content source:


 ShareCompartir
ShareCompartir