Ichthyosis
Ichthyosis is a family of rare genetic skin disorders characterized by dry, thickened, scaly skin.[1]
| Ichthyosis | |
|---|---|
| Other names | Ichthyoses |
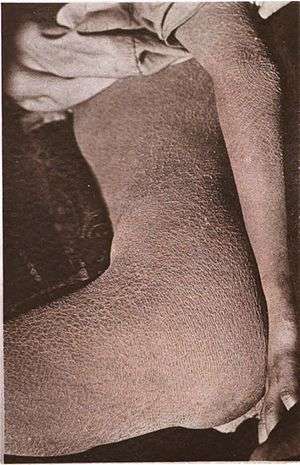 | |
| Ichthyosis is characterized by rough, scaly skin. | |
| Specialty | Dermatology |
The more than 20 types of ichthyosis range in severity of symptoms, outward appearance, underlying genetic cause, and mode of inheritance (e.g., whether the abnormal gene inherited is dominant, recessive, autosomal or X-linked).[2] Ichthyosis comes from the Greek ἰχθύς, ichthys, literally "fish", since dry, scaly skin is the defining feature of all forms of ichthyosis.[3]
The severity of symptoms can vary enormously, from the mildest, most common, types such as ichthyosis vulgaris, which may be mistaken for normal dry skin, up to life-threatening conditions such as harlequin-type ichthyosis. Ichthyosis vulgaris accounts for more than 95% of cases.[4]
Types
Many types of ichthyoses exist, and an exact diagnosis may be difficult. Types of ichthyoses are classified by their appearance and their genetic cause. Ichthyosis caused by the same gene can vary considerably in severity and symptoms. Some ichthyoses do not appear to fit exactly into any one type. Different genes can produce ichthyoses with similar symptoms. Of note, X-linked ichthyosis is associated with Kallmann syndrome (close to the KAL1 gene). The most common or well-known types are:[5]
Genetic simple ichthyoses
| Name | OMIM | Gene | Protein |
|---|---|---|---|
| Ichthyosis vulgaris | 146700 | FLG | Filaggrin |
| X-linked ichthyosis | 308100 | STS | Steroid sulfatase |
| Congenital ichthyosiform erythroderma, Nonbullous (nbCIE) | 242100 | TGM1, ALOXE3/ALOX12B | Transglutaminase 1 Arachidonate lipoxygenase 3 Arachidonate 12-lipoxygenase, 12R type |
| Epidermolytic hyperkeratosis (bullous ichthyosis, bCIE) | 113800 | KRT1, KRT10 | Keratins |
| Harlequin-type ichthyosis | 242500 | ABCA12 | ATP-binding cassette transporter 12 |
| Ichthyosis bullosa of Siemens | 146800 | KRT2 | Keratin 2A |
| Ichthyosis hystrix, Curth-Macklin type | 146590 | KRT1 | Keratin 1 |
| Hystrix-like ichthyosis with deafness | 602540 | GJB2 | Connexin-26 (Gap junction beta-2) |
| Lamellar ichthyosis, type 1 | 242300 | TGM1 | Transglutaminase 1 |
| Lamellar ichthyosis, type 2 | 601277 | ABCA12 | ATP-binding cassette transporter 12 |
| Lamellar ichthyosis, type 3 | 604777 | CYP4F22 | Cytochrome P450, subfamily 4F, polypeptide 22 |
| Lamellar ichthyosis, type 4 | 613943 | LIPN | Lipase family, member N |
| Lamellar ichthyosis, type 5 | 606545 | ALOXE3 | Arachidonate lipoxygenase 3 |
| Autosomal recessive congenital ichthyosis[6] | 615023 | CERS3 | ceramide synthase 3 |
Genetic disease with ichthyosis
| Name | OMIM | Gene | Protein |
|---|---|---|---|
| CHILD syndrome | 308050 | NSHDL | NAD(P) dependent steroid dehydrogenase-like |
| Conradi–Hünermann syndrome | 302960 | EBP | Emopamil binding protein |
| Ichthyosis follicularis with alopecia and photophobia syndrome | 308205 | MBTPS2 | Membrane-bound transcription factor peptidase, site 2 |
| Keratitis–ichthyosis–deafness syndrome | 148210 | GJB2 | Connexin-26 |
| Netherton syndrome | 256500 | SPINK5 | Serine peptidase inhibitor, Kazal type 5 |
| Neutral lipid storage disease with ichthyosis | 275630 | ABHD5 | 1-acylglycerol-3-phosphate O-acyltransferase |
| Adult Refsum disease | 266500 | PHYH PEX7 |
Phytanoyl-CoA hydroxylase Peroxin 7 |
| Ichthyosis and male hypogonadism | 308200 | ? | |
| Sjögren–Larsson syndrome | 270200 | ALDH3A2 | Fatty acid dehydrogenase |
| Photosensitive trichothiodystrophy (IBIDS syndrome) | 601675 | ERCC2, ERCC3, GTF2H5 | Transcription factor IIH components |
| Gaucher disease, type 2 | 230900 | GBA | Glucocerebrosidase |
Non-genetic ichthyosis
Diagnosis
A physician often can diagnose ichthyosis by looking at the skin. A family history is very useful. In some cases, a skin biopsy is done to help to confirm the diagnosis. In some instances, genetic testing may be helpful in making a diagnosis. Diabetes has not been definitively linked to acquired ichthyosis or ichthyosis vulgaris; however, there are case reports associating new onset ichthyosis with diabetes.[7]
Ichthyosis has been found to be more common in Native American, Asian, Mongolian groups. There is no way to prevent ichthyosis.
Ichthyosis is a genetically and phenotypically heterogeneous disease that can be isolated and restricted to the skin manifestations or associated with extracutaneous symptoms. One of which is limb reduction defect known as CHILD syndrome; a rare inborn error of metabolism of cholesterol biosynthesis that is usually restricted to one side of the body. A research done in Egypt proved that it is not a child syndrome and discussed all the case report.[8]
Treatments
Treatments for ichthyosis often take the form of topical application of creams and emollient oils, in an attempt to hydrate the skin. Creams containing a high percentage of urea or lactic acid have been shown to work exceptionally well in some cases.[9] Application of propylene glycol is another treatment method. Retinoids are used for some conditions.
Exposure to sunlight may improve or worsen the condition. In some cases, excess dead skin sloughs off much better from wet tanned skin after bathing or a swim, although the dry skin might be preferable to the damaging effects of sun exposure.
There can be ocular manifestations of ichthyosis, such as corneal and ocular surface diseases. Vascularizing keratitis, which is more commonly found in congenital keratitis-ichythosis-deafness (KID), may worsen with isotretinoin therapy.
Other animals
Ichthyosis or ichthyosis-like disorders exist for several types of animals, including cattle, chickens, llamas, mice and dogs.[10] Ichthyosis of varying severity is well documented in some popular breeds of domestic dogs. The most common breeds to have ichthyosis are Golden retrievers, American bulldogs, Jack Russell terriers and Cairn terriers.[11]
See also
References
- "Frequently Asked Questions". Foundation for Ichthyosis & Related Skin Types (FIRST). Retrieved 12 July 2017.
- thefreedictionary.com/ichthyosis citing: Gale Encyclopedia of Medicine. Copyright 2008
- "Ichthyosis". Health Information Library. Johns Hopkins Medicine. Archived from the original on 2 February 2009.
- Okulicz JF, Schwartz RA (2003). "Hereditary and acquired ichthyosis vulgaris". International Journal of Dermatology. 42 (2): 95–8. doi:10.1046/j.1365-4362.2003.01308.x. PMID 12708996.
- Types of Ichthyosis, Foundation for Ichthyosis & Related Skin Types (F.I.R.S.T.)
- Impaired epidermal ceramide synthesis causes autosomal recessive congenital ichthyosis and reveals the importance of ceramide acyl chain length, J Invest Dermatol. 2013 Sep;133(9):2202-11.
- Scheinfeld, N; Libkind, M; Freilich, S (2001). "New-onset ichthyosis and diabetes in a 14-year-old". Pediatric Dermatology. 18 (6): 501–3. doi:10.1046/j.1525-1470.2001.1862004.x. PMID 11841637.
- Shawky, R. M., Elsayed, S. M., & Amgad, H. (2016). Autosomal recessive ichthyosis with limb reduction defect: A simple association and not CHILD syndrome. Egyptian Journal of Medical Human Genetics, 17(3), 255-258.
- Cicely Blair (February 1976). "The action of a urea—lactic acid ointment in ichthyosis". British Journal of Dermatology. 94 (2): 145–153. doi:10.1111/j.1365-2133.1976.tb04363.x. PMID 943169.
- Sundberg, John P., Handbook of Mouse Mutations with Skin and Hair Abnormalities, Page 333, Published by CRC Press, 1994, ISBN 0-8493-8372-2
- Gross, Thelma Lee, Veterinary Dermatopathology, Page 174-179, Published by Blackwell Publishing, 2004, ISBN 0-632-06452-8
External links
| Classification | |
|---|---|
| External resources |
| Wikimedia Commons has media related to Ichthyosis. |
- Ichthyosis Overview - US National Institute of Arthritis and Musculoskeletal and Skin Diseases