Cocaine intoxication
Cocaine intoxication refers to the immediate and deleterious effects of cocaine on the body. Although cocaine intoxication and cocaine dependence can be present in the same individual, these syndromes present with different symptoms.
| Cocaine intoxication | |
|---|---|
 | |
| Cocaine | |
| Specialty | Psychiatry, narcology |
Signs and symptoms
Cocaine increases alertness, feelings of well-being, euphoria, energy, competence, sociability, and sexuality. Common side effects include anxiety, increased temperature, paranoia, restlessness, and teeth grinding. With prolonged use, the drug can cause insomnia, weight loss, anorexia, tachycardia, hallucinations, and paranoid delusions.[1] Possible lethal side effects include rapid heartbeat, abnormal heart rhythms, tremors, convulsions, markedly increased core temperature, renal failure, heart attack, stroke and heart failure.[2]
Depression with suicidal ideation may develop in heavy users.[3] Finally, a loss of vesicular monoamine transporters, neurofilament proteins, and other morphological changes appear to indicate a long-term damage to dopamine neurons.[4] Chronic intranasal usage can degrade the cartilage separating the nostrils (the septum nasi), which can eventually lead to its complete disappearance.[5]
Studies have shown that cocaine usage during pregnancy triggers premature labor[6] and may lead to abruptio placentae.[7]
Overdose
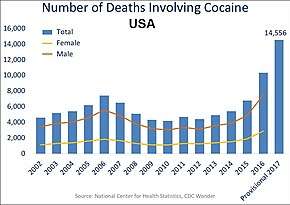
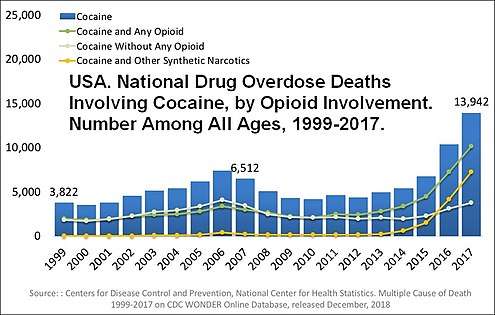
Cocaine can be snorted, swallowed, injected, or smoked. Most deaths due to cocaine are accidental but may also be the result of body packing or stuffing with rupture in the gastrointestinal tract. Use of cocaine causes tachyarrhythmias and a marked elevation of blood pressure (hypertension), which can be life-threatening. This can lead to death from acute myocardial infarction, respiratory failure, stroke, cerebral hemorrhage, or heart failure. Cocaine overdose may result in hyperthermia as stimulation and increased muscular activity cause greater heat production. Heat loss is also inhibited by the cocaine-induced vasoconstriction. Cocaine and/or associated hyperthermia may cause muscle cell destruction (rhabdomyolysis) and myoglobinuria resulting in renal failure. Individuals with cocaine overdose should be transported immediately to the nearest emergency department, preferably by ambulance in case cardiac arrest occurs en route. According to the National Institute on Drug Abuse, approximately 14,600 deaths occurred in the US in 2017 due to cocaine overdose.[8] Because of the increase in heart rate, cocaine users can be prone to elevated body temperatures, tremors, chest pains, and subject to nausea and vomiting. Some psychological symptoms due to an overdose include paranoia, delirium, anxiety as well as panicked feelings.[9] Some signs of an overdose of cocaine are difficulty breathing, loss of urine control, bluish color of the skin, loss of awareness or surroundings, and high blood pressure. Although not as common, death can be caused from an over intoxication of cocaine.[10] Most severe overdoses occur when users combine cocaine with other substances like alcohol or heroin, which increase the effects and heighten the chances of having a dangerous overdose. Treating an overdose can be done by bringing back blood flow to the heart, and restoring the body with oxygen rich blood, especially for the brain to reduce the risk of stroke.[11] Cocaine overdoses have fluctuated over the years. From 2006 to 2010 there has been a decline in the number of reported cases. Though, from 2010 to 2015 there has been an increase in the reported cases involving over cocaine Intoxication. As far as gender goes, it's found that males have a much higher chance of overdosing the females. The ratio of male to female cocaine over doses is 3:1.[12]
Withdrawal
Cocaine withdrawal isn't as severe as the withdrawal from other substances. For example, substances like alcohol and benzodiazepines can involve severe physical withdrawal symptoms while cocaine results in mostly psychological symptoms. Physiological changes caused by cocaine withdrawal include vivid and unpleasant dreams, insomnia, hypersomnia, anger, increased appetite, weight gain, psychomotor retardation, agitation, depression, and anxiety. According to a study done by Gawin and Kleber in 1986, there are three phases in the withdrawal process. They observed the behavior of 30 cocaine-dependent individuals. Phase one, the crash, is characterized by acute dysphoria, irritability and anxiety, increased desire for sleep, exhaustion, increased appetite, decreased craving to use. Phase two, withdrawal, is characterized by increasing craving to use, poor concentration, some irritability and some lethargy, which persisted for up to 10 weeks. Lastly, phase three is characterized by the intermittent craving to use in the context of external cues.[13] Cocaine and its metabolites are completely eliminated from the body by 3 days.[14] There are not any FDA-approved medications that specifically help treat cocaine withdrawal, however, there are some useful medications that could possibly help individuals overcome their addiction. One example is propranolol. Propranolol is a beta blocker that has been approved to treat hypertension, angina, anxiety, and other related psychological problems. Buprenorphine and naltrexone are two substances that act as an effective treatment in the earlier stages of withdrawal.
Pathophysiology
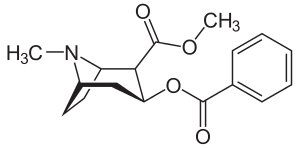
Cocaine pharmacodynamics involve multiple complex mechanisms, although its half-life is short (~ 1 hour).[14] This drug binds and blocks monoamine (dopamine, epinephrine, norepinephrine, and serotonin) re-uptake transporters with equal affinity. Monoamines accumulate in the synaptic cleft resulting in enhanced and prolonged sympathetic effects. Cocaine's acute effect in the central nervous system is to raise the amount of dopamine and serotonin in the nucleus accumbens (the pleasure center in the brain). When this effect ceases due to metabolism of cocaine, depletion of associated neurotransmitters, and receptor down-regulation (tachyphylaxis), the cocaine user may experience dysphoria, or a "crash" after the initial high. The principal actions of cocaine on the cardiovascular system are from alpha- and beta-1-adrenoceptor stimulation resulting in increased heart rate, systemic arterial pressure, and myocardial contractility, which are major determinants of myocardial oxygen demand. Cocaine and its metabolites may cause arterial vasoconstriction hours after use. Epicardial coronary arteries are especially vulnerable to these effects, leading to decreased myocardial oxygen supply. Cocaine-induced platelet activation and thrombus formation is another deleterious effect, caused by alpha-adrenergic- and adenosine diphosphate-mediated increase in platelet aggregation.[15] Plasminogen activator inhibitor is also increased following cocaine use, thereby promoting thrombosis. Similar to local anesthetics such as lidocaine, cocaine blocks sodium channels and interferes with action potential propagation.[16] This Vaughn-Williams class IC effect increases the risk of conduction disturbance and tachyarrhythmias. Adding to its complex toxicity, cocaine targets muscarinic acetylcholine, N-methyl-D-aspartate (NMDA), sigma, and kappa-opioid receptors.[17][18][19][20]
Management
Emergency treatment of cocaine-associated high body temperature consists of giving a benzodiazepine and physical cooling. Cooling is best accomplished with tepid water misting and cooling with a fan.[21][22] There is no specific antidote for cocaine. The chest pain, high blood pressure, and increased heart rate caused by cocaine may be also treated with a benzodiazepine.[23] Multiple and escalating dose of benzodiazepines may be necessary to achieve effect, which increases risk of over-sedation and respiratory depression. A review of cocaine cardiovascular toxicity found benzodiazepines may not always reliably lower heart rate and blood pressure.[24]
Nitric-oxide mediated vasodilators, such as nitroglycerin and nitroprusside, are effective at lowering blood pressure and reversing coronary arterial vasoconstriction, but not heart rate.[24] Nitroglycerin is useful for cocaine-induced chest pain, but the possibility of reflex tachycardia must be considered.[25] Alpha-blockers such as phentolamine have been recommended[23] and may be used to treat cocaine-induced hypertension and coronary arterial vasoconstriction, but these agents do not reduce heart rate.[24][26] Furthermore, phentolamine is rarely used, not readily available in many emergency departments, and many present-day clinicians are unfamiliar with its use. Calcium channel blockers may also be used to treat hypertension and coronary arterial vasoconstriction,[27] but fail to lower tachycardia based on all cocaine-related studies.[24] Non-dihydropyridine calcium channels blockers such as diltiazem and verapamil are preferable, as dihydropyridine agents such as nifedipine have much higher risk of reflex tachycardia.
People who are agitated are best treated with benzodiazepines, though antipsychotics such as haloperidol and olanzapine may also be useful.[24] The alpha-2 agonist dexmedetomidine may also be useful for agitation, but effects on heart rate and blood pressure are variable based on several studies and case reports.[24] Lidocaine and intravenous lipid emulsion have been successfully used for serious ventricular tachyarrhythmias in several case reports.
Beta blockers
The use of beta-blockers for cocaine toxicity has been a relative contraindication despite extremely limited evidence. The phenomenon of “unopposed alpha-stimulation,” in which blood pressure increases or coronary artery vasoconstriction worsens after blockade of beta-2 vasodilation in people using cocaine, is controversial.[28][29] This rarely-encountered and unpredictable adverse effect has resulted in some clinicians advocating for an absolute contraindication of all beta-blockers, including specific, non-specific, and mixed.[30] Many clinicians have disregarded this dogma and administer beta-blockers for cocaine-related chest pain and acute coronary syndrome, especially when there is demand ischemia from uncontrolled tachycardia.[31][32][33][34][35] Of the 1,744 people in the aforementioned systematic review,[24] only 7 adverse events were from putative cases of “unopposed alpha-stimulation” due to propranolol (n=3), esmolol (n=3), and metoprolol (n=1).[36][37][38][39][40] Some detractors of beta-blockers for cocaine-induced chest pain have cited minimal acute mortality and the short half-life of the medication, making it unnecessary to aggressively treat any associated tachycardia and hypertension.[30][41] However, the long-term effect of cocaine use and development of heart failure, with early mortality, high morbidity, and tremendous demand on hospital utilization should be taken under consideration.[42][43][44]
The mixed beta/alpha blocker labetalol has been shown to be safe and effective for treating concomitant cocaine-induced high blood pressure and tachycardia, without any “unopposed alpha-stimulation” recorded.[24][45][46] The use of labetalol is approved by aAHA/ACC guideline for people who have used cocaine and methamphetamine with unstable angina/non-STEMI.[47]
See also
References
- Glauser, Jonathan; Queen, John R. (2007-02-01). "An overview of non-cardiac cocaine toxicity". The Journal of Emergency Medicine. 32 (2): 181–186. doi:10.1016/j.jemermed.2006.05.044. ISSN 0736-4679. PMID 17307630.
- Zimmerman, Janice L. (2012-10-01). "Cocaine intoxication". Critical Care Clinics. 28 (4): 517–526. doi:10.1016/j.ccc.2012.07.003. ISSN 1557-8232. PMID 22998988.
- Narvaez, Joana C. M.; Jansen, Karen; Pinheiro, Ricardo T.; Kapczinski, Flávio; Silva, Ricardo A.; Pechansky, Flávio; Magalhães, Pedro V. (2014-08-01). "Psychiatric and substance-use comorbidities associated with lifetime crack cocaine use in young adults in the general population". Comprehensive Psychiatry. 55 (6): 1369–1376. doi:10.1016/j.comppsych.2014.04.021. ISSN 1532-8384. PMID 24933652.
- Little, Karley Y.; Ramssen, Eric; Welchko, Ryan; Volberg, Vitaly; Roland, Courtney J.; Cassin, Bader (2009-08-15). "Decreased brain dopamine cell numbers in human cocaine users". Psychiatry Research. 168 (3): 173–180. doi:10.1016/j.psychres.2008.10.034. ISSN 0165-1781. PMID 19233481.
- Trimarchi, M.; Bussi, M.; Sinico, R. A.; Meroni, Pierluigi; Specks, U. (2013-02-01). "Cocaine-induced midline destructive lesions - an autoimmune disease?". Autoimmunity Reviews. 12 (4): 496–500. doi:10.1016/j.autrev.2012.08.009. ISSN 1873-0183. PMID 22940554.
- Cain, Mary A.; Bornick, Patricia; Whiteman, Valerie (2013-03-01). "The maternal, fetal, and neonatal effects of cocaine exposure in pregnancy". Clinical Obstetrics and Gynecology. 56 (1): 124–132. doi:10.1097/GRF.0b013e31827ae167. ISSN 1532-5520. PMID 23314714.
- Flowers, D.; Clark, J. F.; Westney, L. S. (1991-03-01). "Cocaine intoxication associated with abruptio placentae". Journal of the National Medical Association. 83 (3): 230–232. ISSN 0027-9684. PMC 2627035. PMID 2038082.
- Overdose Death Rates. By National Institute on Drug Abuse (NIDA).
- Staff, Editorial. "Cocaine Overdose: Symptoms and Dangers". American Addiction Centers. Retrieved 2019-10-21.
- "Cocaine intoxication: MedlinePlus Medical Encyclopedia". medlineplus.gov. Retrieved 2019-10-21.
- Abuse, National Institute on Drug. "Cocaine". www.drugabuse.gov. Retrieved 2019-10-21.
- Staff, Editorial. "Cocaine Overdose: Symptoms and Dangers". American Addiction Centers. Retrieved 2019-10-29.
- "Department of Health | The cocaine withdrawal syndrome". www1.health.gov.au. Retrieved 2019-10-29.
- Jufer, R. A.; Wstadik, A.; Walsh, S. L.; Levine, B. S.; Cone, E. J. (2000-10-01). "Elimination of cocaine and metabolites in plasma, saliva, and urine following repeated oral administration to human volunteers". Journal of Analytical Toxicology. 24 (7): 467–477. doi:10.1093/jat/24.7.467. ISSN 0146-4760. PMID 11043648.
- Heesch, C. M.; Wilhelm, C. R.; Ristich, J.; Adnane, J.; Bontempo, F. A.; Wagner, W. R. (2000-06-01). "Cocaine activates platelets and increases the formation of circulating platelet containing microaggregates in humans". Heart. 83 (6): 688–695. doi:10.1136/heart.83.6.688. ISSN 1468-201X. PMC 1760877. PMID 10814631.
- Hariman, Robert J.; Liu, Dong; Loeb, Henry S.; McKieman, Thomas L.; Scanlon, Patrick J.; Bauman, Jerry L. (1996-02-01). "Competitive binding between cocaine and lidocaine". Journal of the American College of Cardiology. 27 (2): 80. doi:10.1016/S0735-1097(96)80520-1.
- Williams, Mark J.; Adinoff, Bryon (2008-07-01). "The role of acetylcholine in cocaine addiction". Neuropsychopharmacology. 33 (8): 1779–1797. doi:10.1038/sj.npp.1301585. ISSN 0893-133X. PMC 2667818. PMID 17928814.
- Haile, Colin N.; Mahoney, James J.; Newton, Thomas F.; De La Garza, Richard (2012-05-01). "Pharmacotherapeutics directed at deficiencies associated with cocaine dependence: focus on dopamine, norepinephrine and glutamate". Pharmacology & Therapeutics. 134 (2): 260–277. doi:10.1016/j.pharmthera.2012.01.010. ISSN 1879-016X. PMC 3341931. PMID 22327234.
- Narayanan, Sanju; Mesangeau, Christophe; Poupaert, Jacques H.; McCurdy, Christopher R. (2011-01-01). "Sigma receptors and cocaine abuse". Current Topics in Medicinal Chemistry. 11 (9): 1128–1150. doi:10.2174/156802611795371323. ISSN 1873-4294. PMID 21050176.
- Kivell, Bronwyn M.; Ewald, Amy W. M.; Prisinzano, Thomas E. (2014-01-01). Salvinorin A analogs and other κ-opioid receptor compounds as treatments for cocaine abuse. Advances in Pharmacology. 69. pp. 481–511. doi:10.1016/B978-0-12-420118-7.00012-3. ISBN 9780124201187. ISSN 1557-8925. PMC 4128345. PMID 24484985.
- Smith, Caroline J.; Johnson, John M. (2016-04-01). to hyperthermia.pdf "Responses to hyperthermia. Optimizing heat dissipation by convection and evaporation: Neural control of skin blood flow and sweating in humans" Check
|url=value (help) (PDF). Autonomic Neuroscience: Basic & Clinical. 196: 25–36. doi:10.1016/j.autneu.2016.01.002. ISSN 1872-7484. PMID 26830064. - Richards, John R.; Colby, Daniel K. (2016-01-01). "Stimulant-induced hyperthermia and ice-water submersion: Practical considerations". Clinical Toxicology. 54 (1): 69–70. doi:10.3109/15563650.2015.1104536. ISSN 1556-9519. PMID 26515112.
- McCord, J; Jneid, H; Hollander, JE; de Lemos, JA; Cercek, B; Hsue, P; Gibler, WB; Ohman, EM; Drew, B; Philippides, G; Newby, LK; American Heart Association Acute Cardiac Care Committee of the Council on Clinical, Cardiology (Apr 8, 2008). "Management of cocaine-associated chest pain and myocardial infarction: a scientific statement from the American Heart Association Acute Cardiac Care Committee of the Council on Clinical Cardiology". Circulation. 117 (14): 1897–907. doi:10.1161/CIRCULATIONAHA.107.188950. PMID 18347214.
- Richards, John R.; Garber, Dariush; Laurin, Erik G.; Albertson, Timothy E.; Derlet, Robert W.; Amsterdam, Ezra A.; Olson, Kent R.; Ramoska, Edward A.; Lange, Richard A. (2016-06-01). "Treatment of cocaine cardiovascular toxicity: a systematic review". Clinical Toxicology. 54 (5): 345–364. doi:10.3109/15563650.2016.1142090. ISSN 1556-9519. PMID 26919414.
- Ma, Sheng-xing; Schmid, Phillip G.; Long, John P. (1994-01-01). "Noradrenergic mechanisms and the cardiovascular actions of nitroglycerin". Life Sciences. 55 (21): 1595–1603. doi:10.1016/0024-3205(94)00325-4. PMID 7968233.
- Lange, Richard A.; Cigarroa, Ricardo G.; Yancy, Clyde W. Jr.; Willard, John E.; Popma, Jeffrey J.; Sills, Michael N.; McBride, Wade; Kim, Anatole S.; Hillis, L. David (1989-12-07). "Cocaine-Induced Coronary-Artery Vasoconstriction". New England Journal of Medicine. 321 (23): 1557–1562. doi:10.1056/NEJM198912073212301. ISSN 0028-4793. PMID 2573838.
- Negus, Brian H.; Willard, John E.; Hillis, L.David; Glamann, D.Brent; Landau, Charles; Snyder, Richard W.; Lange, Richard A. (1994-03-01). "Alleviation of cocaine-induced coronary vasoconstriction with intravenous verapamil". The American Journal of Cardiology. 73 (7): 510–513. doi:10.1016/0002-9149(94)90684-x. ISSN 0002-9149. PMID 8141094.
- Schurr, James W.; Gitman, Brenda; Belchikov, Yuly (2014-12-01). "Controversial therapeutics: the β-adrenergic antagonist and cocaine-associated cardiovascular complications dilemma". Pharmacotherapy. 34 (12): 1269–1281. doi:10.1002/phar.1486. ISSN 1875-9114. PMID 25224512.
- Freeman, Kalev; Feldman, James A. (2008-02-01). "Cocaine, myocardial infarction, and beta-blockers: time to rethink the equation?". Annals of Emergency Medicine. 51 (2): 130–134. doi:10.1016/j.annemergmed.2007.08.020. ISSN 1097-6760. PMID 17933425.
- Gupta, Amit K.; Greller, Howard A.; Hoffman, Robert Steven (2010-11-08). "Beta-blockers and cocaine: still a bad idea". Archives of Internal Medicine. 170 (20): 1859–1860, author reply 1860. doi:10.1001/archinternmed.2010.398. ISSN 1538-3679. PMID 21059982.
- Dattilo, Philip B.; Hailpern, Susan M.; Fearon, Kerrie; Sohal, Davendra; Nordin, Charles (2008-02-01). "Beta-blockers are associated with reduced risk of myocardial infarction after cocaine use". Annals of Emergency Medicine. 51 (2): 117–125. doi:10.1016/j.annemergmed.2007.04.015. ISSN 1097-6760. PMID 17583376.
- Rangel, Carlos; Shu, Richard G.; Lazar, Lawrence D.; Vittinghoff, Eric; Hsue, Priscilla Y.; Marcus, Gregory M. (2010-05-24). "Beta-blockers for chest pain associated with recent cocaine use". Archives of Internal Medicine. 170 (10): 874–879. doi:10.1001/archinternmed.2010.115. ISSN 1538-3679. PMID 20498415.
- Ibrahim, Morhaf; Maselli, Diego Jose; Hasan, Reham; Hamilton, Andrew (2013-03-01). "Safety of β-blockers in the acute management of cocaine-associated chest pain". The American Journal of Emergency Medicine. 31 (3): 613–616. doi:10.1016/j.ajem.2012.09.027. ISSN 1532-8171. PMID 23122421.
- Fanari, Zaher; Kennedy, Kevin K.; Lim, Michael J.; Laddu, Abhay A.; Stolker, Joshua M. (2014-06-01). "Comparison of in-hospital outcomes for beta-blocker use versus non-beta blocker use in patients presenting with cocaine-associated chest pain". The American Journal of Cardiology. 113 (11): 1802–1806. doi:10.1016/j.amjcard.2014.03.010. ISSN 1879-1913. PMID 24742472.
- Gupta, Navdeep; Washam, Jeffrey B.; Mountantonakis, Stavros E.; Li, Shuang; Roe, Matthew T.; de Lemos, James A.; Arora, Rohit (2014-03-01). "Characteristics, management, and outcomes of cocaine-positive patients with acute coronary syndrome (from the National Cardiovascular Data Registry)". The American Journal of Cardiology. 113 (5): 749–756. doi:10.1016/j.amjcard.2013.11.023. ISSN 1879-1913. PMID 24388623.
- Ramoska, Edward; Sacchetti, Alfred D (1985-11-01). "Propranolol-induced hypertension in treatment of cocaine intoxication". Annals of Emergency Medicine. 14 (11): 1112–1113. doi:10.1016/s0196-0644(85)80934-3. ISSN 0196-0644. PMID 4051280.
- Fareed, Fareed N.; Chan, Gar; Hoffman, Robert S. (2007-12-01). "Death temporally related to the use of a Beta adrenergic receptor antagonist in cocaine associated myocardial infarction". Journal of Medical Toxicology. 3 (4): 169–172. doi:10.1007/bf03160934. ISSN 1556-9039. PMC 3550023. PMID 18072171.
- Sand, I.Charles; Brody, Steven L.; Wrenn, Keith D.; Slovis, Corey M. (1991-03-01). "Experience with esmolol for the treatment of cocaine-associated cardiovascular complications". The American Journal of Emergency Medicine. 9 (2): 161–163. doi:10.1016/0735-6757(91)90182-j. ISSN 0735-6757. PMID 1671639.
- Lange, Richard A.; Cigarroa, Ricardo G.; Flores, Eduardo D.; McBride, Wade; Kim, Anatole S.; Wells, Peter J.; Bedotto, John B.; Danziger, Robert S.; Hillis, L. David (1990-06-15). "Potentiation of Cocaine-Induced Coronary Vasoconstriction by Beta-Adrenergic Blockade". Annals of Internal Medicine. 112 (12): 897–903. doi:10.7326/0003-4819-112-12-897. ISSN 0003-4819. PMID 1971166.
- Izquierdo Gómez, María Manuela; Domínguez-Rodríguez, Alberto; Gálvez Rodríguez, Manuel; Marrero Rodríguez, Francisco (2009-04-01). "Reflections on beta-adrenergic receptor blockers and cocaine use. A case in point". Revista Española de Cardiología. 62 (4): 455–456. doi:10.1016/s1885-5857(09)71677-9. ISSN 1579-2242. PMID 19401135.
- Hollander, Judd (December 28, 2011). "Update on Cocaine Myocardial Ischemia". Archived from the original on January 11, 2017.
- Casartelli, Alessandro; Dacome, Lisa; Tessari, Michela; Pascali, Jennifer; Bortolotti, Federica; Trevisan, Maria Teresa; Bosco, Oliviero; Cristofori, Patrizia; Tagliaro, Franco (2014-01-01). "Cocaine-associated increase of atrial natriuretic peptides: an early predictor of cardiac complications in cocaine users?". Heart Asia. 6 (1): 100–107. doi:10.1136/heartasia-2013-010482. ISSN 1759-1104. PMC 4832714. PMID 27326180.
- Liaudet, Lucas; Calderari, Belinda; Pacher, Pal (2014-11-01). "Pathophysiological mechanisms of catecholamine and cocaine-mediated cardiotoxicity" (PDF). Heart Failure Reviews. 19 (6): 815–824. doi:10.1007/s10741-014-9418-y. ISSN 1573-7322. PMID 24398587.
- Walsh, David W.; McVey, Molly C.; Gass, Abigal; Zhang, Jingwen; Mauldin, Patrick D.; Rockey, Don C. (2016-06-24). "Identification of high resource utilizing patients on internal medicine hospital services". Journal of Investigative Medicine. 64 (7): jim–2016–000118. doi:10.1136/jim-2016-000118. ISSN 1708-8267. PMID 27342424.
- Boehrer, James D.; Moliterno, David J.; Willard, John E.; Hillis, L.David; Lange, Richard A. (1993-06-01). "Influence of labetalol on cocaine-induced coronary vasoconstriction in humans". The American Journal of Medicine. 94 (6): 608–610. doi:10.1016/0002-9343(93)90212-8. ISSN 0002-9343. PMID 8506886.
- Richards, John R.; Lange, Richard A. (2016-02-01). "Labetalol and cardiovascular consequences of cocaine use". Trends in Cardiovascular Medicine. 26 (2): 202–203. doi:10.1016/j.tcm.2015.05.002. ISSN 1873-2615. PMID 26116092.
- Anderson, Jeffrey L.; Adams, Cynthia D.; Antman, Elliott M.; Bridges, Charles R.; Califf, Robert M.; Casey, Donald E.; Chavey, William E.; Fesmire, Francis M.; Hochman, Judith S. (2013-06-11). "2012 ACCF/AHA focused update incorporated into the ACCF/AHA 2007 guidelines for the management of patients with unstable angina/non-ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines". Journal of the American College of Cardiology. 61 (23): e179–347. doi:10.1016/j.jacc.2013.01.014. ISSN 1558-3597. PMID 23639841.
External links
| Classification | |
|---|---|
| External resources |