2016 STD Prevention Conference Highlights
This web page is archived for historical purposes and is no longer being updated.
Adolescents and Young Adults
The 2016 STD Prevention Conference showcases the latest STD prevention research, both from the United States and abroad.
This page highlights three presentations and one scientific poster focusing on STDs among adolescents and young adults, including research into increases in STDs among young male adolescents across the U.S. and an analysis of an innovative STD self-testing option for university students.
Poster or presentation images, as well as full abstracts and related links follow below.

Fast Facts
- Young people aged 15-24 account for half of the nearly 20 million new sexually transmitted infections that occur each year in the United States.
- Both the number and rates of reported cases of chlamydia and gonorrhea continues to be highest among people aged 15-24.
- Young women face the most serious long-term health consequences. It is estimated that undiagnosed STDs cause more than 20,000 women to become infertile each year.
Adolescents & Young Adults Abstracts
- 2C4 – College Sexual Health Services
- 2C5 STD Self-Test Program
- WP31 – Adolescent STD Rates
- 4C3 – Trans* College Students
MAKING THE GRADE: ASSESSING THE PROVISION OF SEXUAL HEALTH SERVICES AT U.S. COLLEGES & UNIVERSITIES
Alexandra Caccamo, MPH1, Melissa Habel, MPH1, Oscar Beltran, PhD1, Jeffrey Becasen, MPH2, William Pearson, PhD, FACE1 and Patricia Dittus, PhD1
1Division of STD Prevention, Centers for Disease Control and Prevention, Atlanta, 2Division of HIV/AIDS Prevention, Centers for Disease Control and Prevention, Atlanta
Background: College health centers (HCs) can play a pivotal role in the introduction and normalization of timely STD screenings. We surveyed colleges and universities across the United States to describe the array of sexual health services provided.
Methods: We sampled 885 US colleges from the Integrated Postsecondary Education Data System (2014-2015). Only active, 2- or 4-year, degree-granting, accredited institutions, which enrolled at least 500 students were included. 482 schools responded to the survey (55%), and were weighted to be nationally-representative. We reported on STD services provided and stratified results by minority-serving institutions (MSIs) and non-MSIs as well as 2-year and 4-year institutions; differences were tested using Chi-square analyses.
Results: Of the weighted sample 67.7% of colleges reported having a student HC, of which 74.4% offered STD diagnosis and treatment (4y vs. 2y; 78.3% vs. 57.6%, p<.001); 73.5% of HCs reported routine chlamydia (CT) screening in women (4y vs. 2y; 75.4% vs. 63.6%, p=.004) and 24.7% offered express STD testing (26.1% vs 15.6%, p=.005); follow-up CT screening and self-collected vaginal swabs were offered at 82.7% and 31.0% of HCs, though no significant differences existed. Nearly all HCs offered HIV testing (92.3%) with MSIs reporting higher availability of HIV testing compared to non-MSIs (96.2% vs. 91.2%, p=.005). In regard to services for MSM, 46.8% of HCs offered pharyngeal and rectal (43.8%) STD testing. HPV vaccination was offered at 70.3% of HCs. Free testing was offered at only 10.3% of HCs. Of note, 37.0% of HCs reported that a local health department or outside organization were the primary offerors of STD services.
Conclusions: Colleges with HCs are providing a variety of sexual health services, but 2-year colleges may require additional support. Improvements could entail increasing routine CT screening for women, extra-genital STD testing for MSM, and removing barriers to testing by offering express and self-testing.
CREATING INNOVATIVE STD TESTING OPTIONS FOR UNIVERSITY STUDENTS: THE IMPACT OF A STD SELF-TESTING PROGRAM
Melissa Habel, MPH1, Kate Brookmeyer, PhD1, Shelley Haffner, RNC2, and Robin Oliver-Veronesi, MD, FACOG3
1Division of STD Prevention, Centers for Disease Control and Prevention, Atlanta, 2Infectious Diseases, Penn State University, University Park, 3Women's Health, Penn State University, University Park
Background: National data estimates that STD testing among young adults remains low, despite high-risk behavior. University health settings are an ideal location for innovative testing methods; self-collected vaginal swabs (SCVS) are cost effective, more sensitive than urine, and easier to process/transport than traditional clinician-obtained specimens. However, research is limited on the acceptability of self-testing/SCVS and its effect on testing uptake.
Methods: To assess acceptability and uptake of SCVS (urine and self-collected vaginal swabs), we conducted a brief self-administered survey of students accessing a large US-based university health center from January – December 2015. The survey (PDA-based, Qualtrics) assessed student demographics, reasons for testing, and satisfaction with the self-testing option. The cost for CT/GC testing was $30.
Results: Overall, 18.8% (825/4391) of students opted for the self-test option, of which 189/825 completed the survey. Of students surveyed, 63% reported that their main reason for testing was: “I had unprotected sex and wish to get tested.” In the past year, 44% had 2-3 sex partners (vaginal or anal intercourse) and 42% reported 4 or more partners. Ease of testing/no appointment needed was the main reason for choosing SCVS (69%). The majority were very satisfied with the self-test option and likely to use the service again (82%). Among students choosing self-tests, positivity was 11.8% (11.9% female, 11.6% males) compared to 6.7% positivity (4.7% female, 12.4% male) in clinician-collected tests during 2015. Since implementation of the self-test option (2013 baseline), the health center has seen an 18.1% increase in overall STD testing and a 44.6% increase in the detection of positive cases.
Conclusions: Self-testing in the university health setting may be an efficient and effective way to provide STD testing for students, and may increase testing uptake. Multiple partners, disclosure of unprotected sex, and detected infections suggest that it is not just the low-risk worried-well presenting for testing.
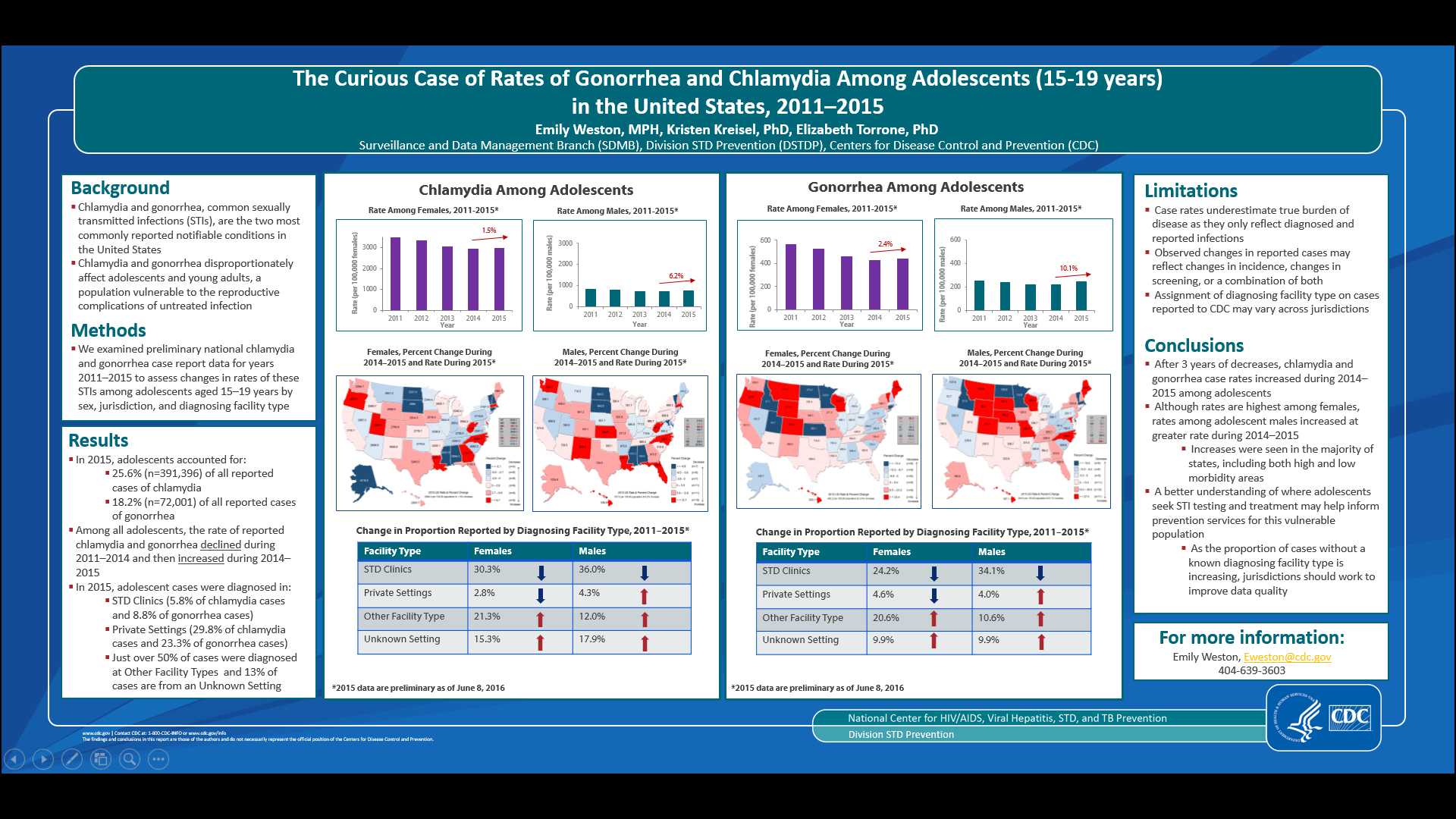
THE CURIOUS CASE OF RATES OF GONORRHEA AND CHLAMYDIA AMONG ADOLESCENTS (15-19 YEARS) IN THE UNITED STATES, 2011-2015
Emily Weston, MPH, Kristen Kreisel, PhD, Elizabeth Torrone, PhD
Background: Chlamydia and gonorrhea disproportionately affect adolescents and young adults. To describe burden of disease and inform prevention and control activities, we investigated trends in rates of reported cases among adolescents.
Methods: We examined national chlamydia and gonorrhea case report data for 2011–2015 to assess rates of chlamydia and gonorrhea among adolescents aged 15–19 years by sex, region, and diagnosing facility type. Data from 2015 are preliminary and include cases reported to CDC as of March 3, 2016.
Results: In 2015, 379,496 chlamydia cases and 69,440 gonorrhea cases were reported among adolescents, accounting for 25.6% and 18.1% of all reported chlamydia and gonorrhea cases, respectively. During 2011–2015, rates of chlamydia and gonorrhea declined among adolescent females; chlamydia: 3,485.2 to 2,905.6 cases per 100,000 population and gonorrhea: 567.7 to 426.8 cases per 100,000. However, among adolescent males, rates declined during 2011–2014 (chlamydia: 816.3 to 722.4 cases per 100,000 and gonorrhea: 252.7 to 222.2 cases per 100,000) and then increased during 2014–2015 (chlamydia increased 2.8% to 742.6 cases per 100,000 and gonorrhea increased 6.2% to 235.9 cases per 100,000). Rates of gonorrhea among adolescent males increased in all regions during 2014–2015. Strikingly, the gonorrhea rate among adolescent males in the West increased annually 10.6% and 48% overall during 2011–2015 (109.5 to 162.1 cases per 100,000). During 2011–2015, the proportion of adolescent male cases diagnosed in STD clinics declined from 18.2% to 11.7% while the proportion diagnosed in private settings remained unchanged and proportion with unknown facility type increased.
Conclusions: After years of decreases, preliminary 2015 data indicate chlamydia and gonorrhea rates are increasing among adolescent males while rates continue to decline among adolescent females. A better understanding of where adolescents seek STI testing and treatment may help inform prevention services for this vulnerable population.
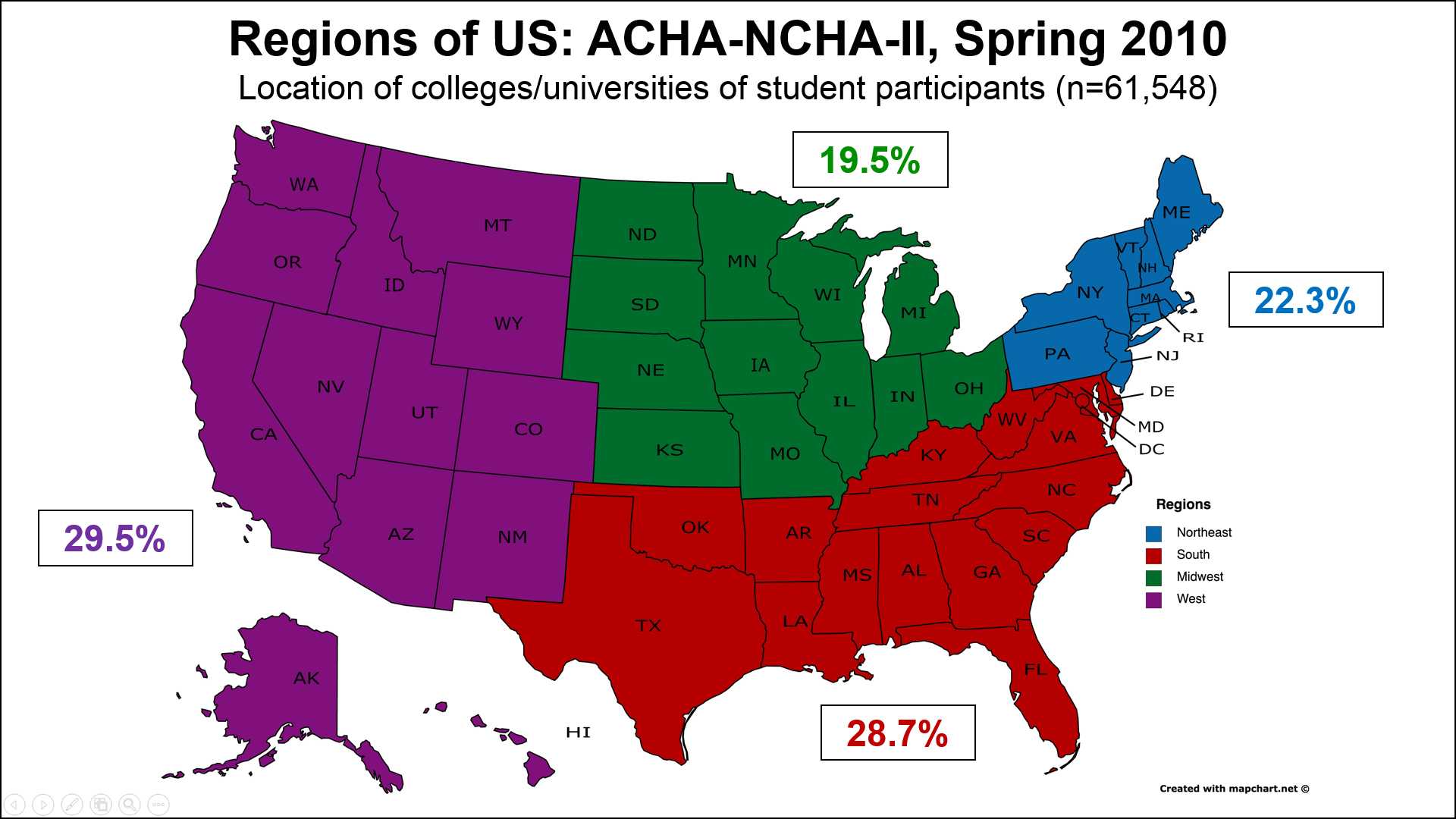
STDS AMONG TRANSGENDER COLLEGE STUDENTS IN THE US: THE ROLE OF EXPERIENCED DISCRIMINATION
Lisa Lindley, DrPH, MPH, CHES, Department of Global & Community Health, George Mason University, Fairfax, VA
Todd Sabato, PhD, Department of Kinesiology and Public Health Education, University of North Dakota, Grand Forks, ND
Background: Limited research has explored the relationship between experienced discrimination and STDs among transgender college students in the U.S.; which was the purpose of this investigation.
Methods: We conducted a secondary analysis of the American College Health Association’s Spring 2010 National College Health Assessment-II survey data. A total of 95,712 students from 139 institutions completed the survey. We restricted the sample to include students who were of traditional college age (18-24 years), attended a 4-year institution in the United States, and reported their gender (female, male, or transgender) (n=61,548). A total of 106 students identified as transgender. Because the NCHA-II does not distinguish between trans-men and trans-women in the transgender category, we combined male and female college students into a “cisgender” category for comparison purposes. Multivariate logistic regression analyses were conducted to identify factors associated with an STD (past year) based on gender (cis vs. trans), demographic characteristics (age, race/ethnicity, international status, region of U.S.), behavioral risk factors (sexual, alcohol and poly-drug use), and experienced discrimination (racism, sexism, homophobia) (past year).
Results: Overall, 2.5% of college students had an STD (past year) and 5.1% experienced discrimination (past year). Transgender students were significantly (p<.001) more likely than cisgender students to have had an STD (12.3% vs. 2.5%, respectively) and to have experienced discrimination (50.0% vs. 5.1%, respectively). In unadjusted models, transgender students had 5.6 times greater odds (95% CI: 3.1-9.9) of having an STD than cisgender students. This relationship remained significant after adjusting for demographic characteristics and risk behaviors. However, after adjusting for experienced discrimination, the association between gender and having an STD became non-significant, suggesting that experienced discrimination mediates this relationship.
Conclusions: Results indicate that experienced discrimination is a significant risk factor for STDs among transgender college students and reinforces the need for stigma reduction/discrimination prevention efforts on campus.
- Page last reviewed: September 7, 2016 (archived document)
- Content source:


 ShareCompartir
ShareCompartir