2016 STD Prevention Conference Highlights
This web page is archived for historical purposes and is no longer being updated.
Syphilis
The 2016 STD Prevention Conference showcases the latest STD prevention research, both from the United States and abroad.
This page highlights four presentations and one scientific poster taking an in-depth look at the consequences of rising syphilis rates and measures that can help reduce the number of infections.
Poster or presentation images, as well as full abstracts and related links follow below.
Fast Facts
- The syphilis case rate increased 22.7% in women from 2013-2014.
- There were nearly 20,000 cases of syphilis in 2014 (compared to approximately 6,000 in 2001).
- The rate of congenital syphilis increased 37% from 2012-2014.
Syphilis Abstracts
- WP 70 – Syphilis in Philadelphia
- 4B2 – Ocular Syphilis
- 4B3 – Enhanced MSM Screening
- 5C1 – Congenital Syphilis
- 5C2 – Disease Intervention Specialists
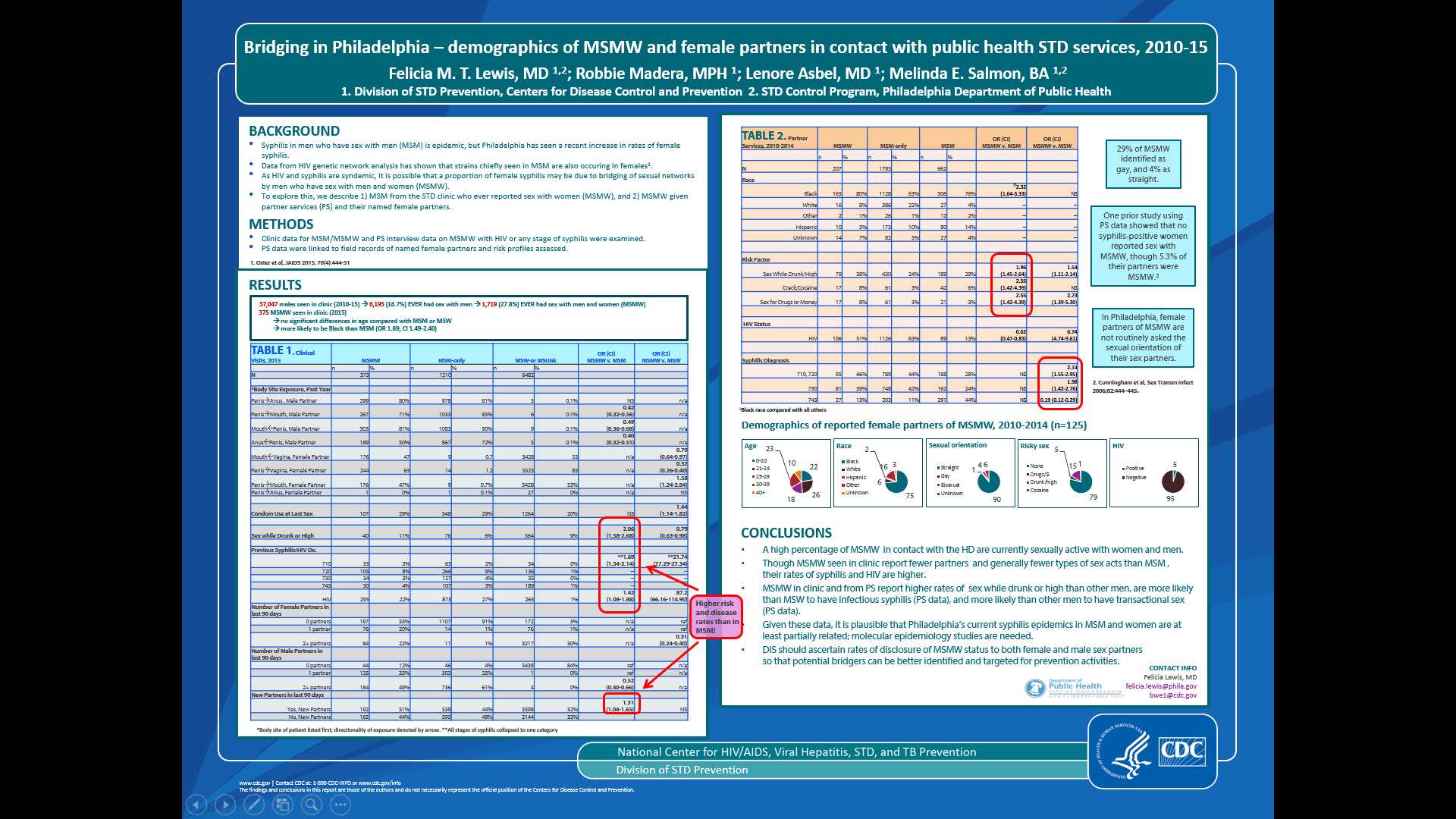
BRIDGING IN PHILADELPHIA – DEMOGRAPHICS OF MSMW AND THEIR NAMED FEMALE PARTNERS IN CONTACT WITH PUBLIC HEALTH STD SERVICES IN PHILADELPHIA, 2010-2014
Felicia M.T. Lewis, MD 1,2; Robbie Madera, MPH 2; Lenore Asbel, MD 2; Melinda E. Salmon 1,2
1Division of STD Prevention, Centers for Disease Control and Prevention
2STD Control Program, Philadelphia Department of Public Health
Background: Syphilis in men who have sex with men (MSM) has increased dramatically, but a recent increase has also occurred in female Philadelphians, raising the question of sexual networks among MSM and heterosexual women. To explore this, we describe 1) MSM from the STD clinic who ever reported sex with women (MSMW), and 2) MSMW given partner services (PS) and their female partners.
Methods: Clinic data for MSM/MSMW and PS interview data on MSMW with HIV or any stage syphilis were examined. PS data were linked to field records of named female partners and risk profiles assessed.
Results: From 2010-15, 37,047 men visited clinic, 6195 (16.7%) of whom ever identified as MSM; of these, 1719 (27.8%) were MSMW. Compared to MSM, MSMW were likelier to be Black. Among MSMW, 65% reported vaginal and 47% receptive and/or insertive oral sex with a female in 2015. MSMW were significantly less likely than MSM to report anal receptive (50% vs 72%), oral insertive (71% vs 85%), or oral receptive sex (81% vs 90%) with males in 2015, but rates of anal insertive sex were similar. MSMW were more likely than MSM to have new partners, sex while drunk/high, and a past diagnosis of syphilis (OR 1.69, CI 1.34-2.14) or HIV (OR 1.42, CI 1.08-1.88). MSMW given PS were likelier to report intoxicated and/or transactional sex, and were likelier than MSW to have infectious syphilis (OR 2.14, CI 1.55-2.95).
Conclusions: MSMW comprise a substantial proportion of MSM in clinic, and most report recent sex with females. MSMW report less sexual activity than MSM, but have higher syphilis/HIV rates. Those given PS are likelier than MSW to have infectious syphilis and riskier sex. These data indicate possible routes of transmission to females and suggest that local syphilis epidemics in MSM and females may be related.
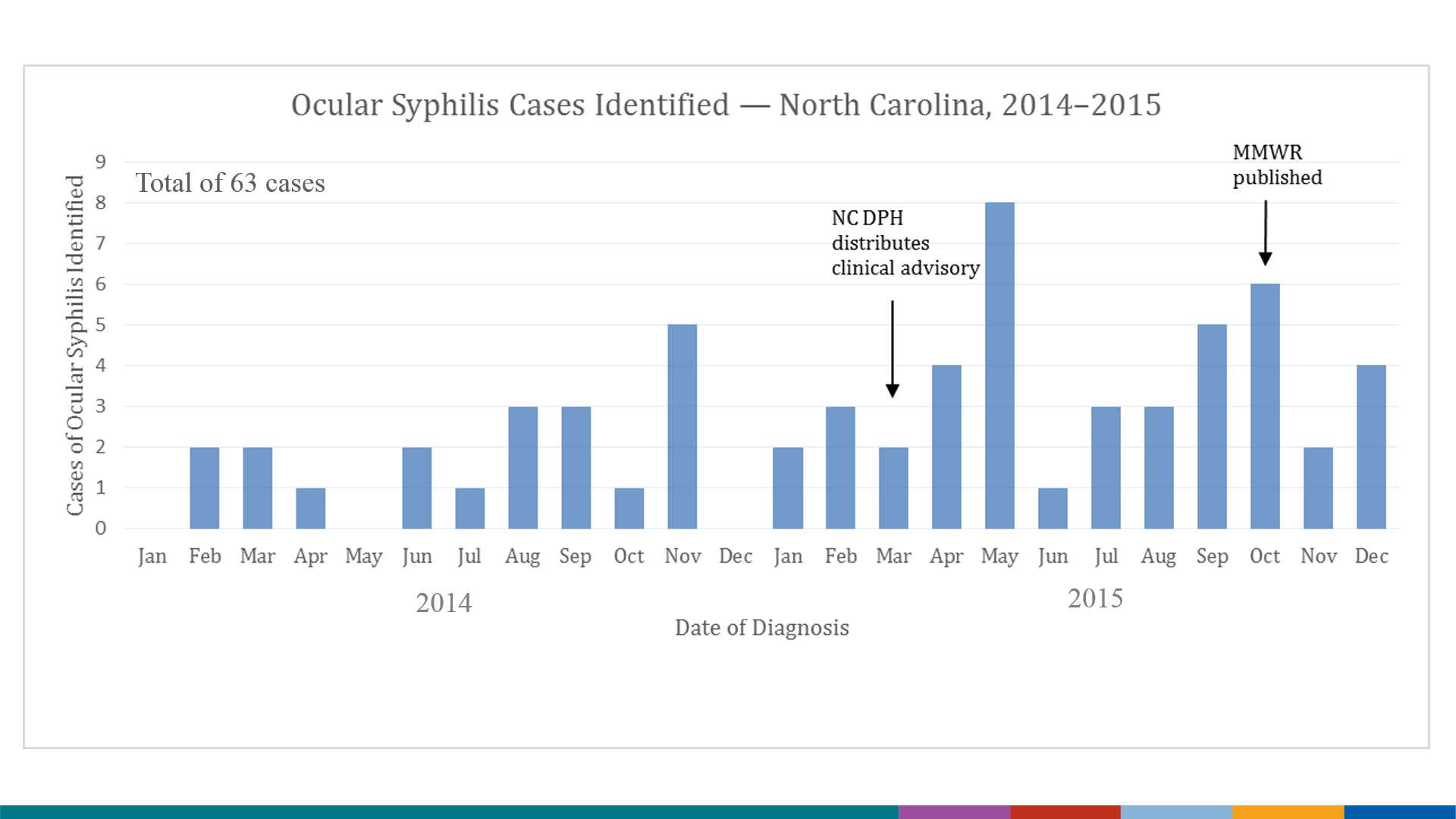
INCREASE IN OCULAR SYPHILIS —NORTH CAROLINA, 2014–2015
Sara Oliver, MD, MSPH, J. Rinsky, A. Cope, C. Williams, G. Liu, T. Peterman, L. Markowitz, A. Fleischauer, E. Samoff
Division of Viral Disease, Centers for Disease Control and Prevention, Atlanta
Background: Ocular syphilis, an inflammatory eye disease, can cause vision loss. Although syphilis is nationally notifiable, ocular manifestations are not. Proportions of syphilis patients with, and risk factors for, ocular syphilis are unknown. Nationally, syphilis rates have increased since 2000, but ocular syphilis clusters were only reported in late 2014. Reports of ocular syphilis in North Carolina increased markedly in 2015. We conducted an investigation to systematically identify ocular syphilis, and determine risk factors, by comparing syphilis cases with and without ocular manifestations.
Methods: We reviewed syphilis cases reported to North Carolina during 2014–2015. Among these, we considered persons with ocular symptoms and signs to have ocular syphilis. We abstracted demographic, risk factor, and sex partner information from health department interviews; characteristics of syphilis cases with and without ocular manifestations were compared using log-binomial regression to estimate prevalence ratios (PRs) and 95% confidence intervals (CIs).
Results: Among 4,234 syphilis patients, 63 (1.5%) had ocular syphilis: 20 in 2014 and 43 in 2015, a 115% increase; syphilis cases increased 35% during this period. Of 59 males, 42 (71%) reported male sex partners. No ocular syphilis patients were identified as sex partners. Patients presented in all syphilis stages; 24 (38%) diagnosed in primary or secondary syphilis. Patients with ocular manifestations were more likely that those without to be male (PR: 2.8; CI:1.0–7.7), white (PR: 2.6; CI:1.6–4.4), aged ≥40 years (PR: 3.3; CI:2.0–5.4) and HIV-infected (PR: 1.8; CI:1.1–2.9). Median RPR tiers for ocular syphilis were higher at every stage. No behavioral risk factors were associated with ocular manifestations.
Conclusions: The increase in ocular syphilis exceeded the rise in reported syphilis cases. Demographic associations may be due to increased access to care, increased recognition or undetected risk factors. Further efforts are ongoing to determine contributing factors and increase awareness.
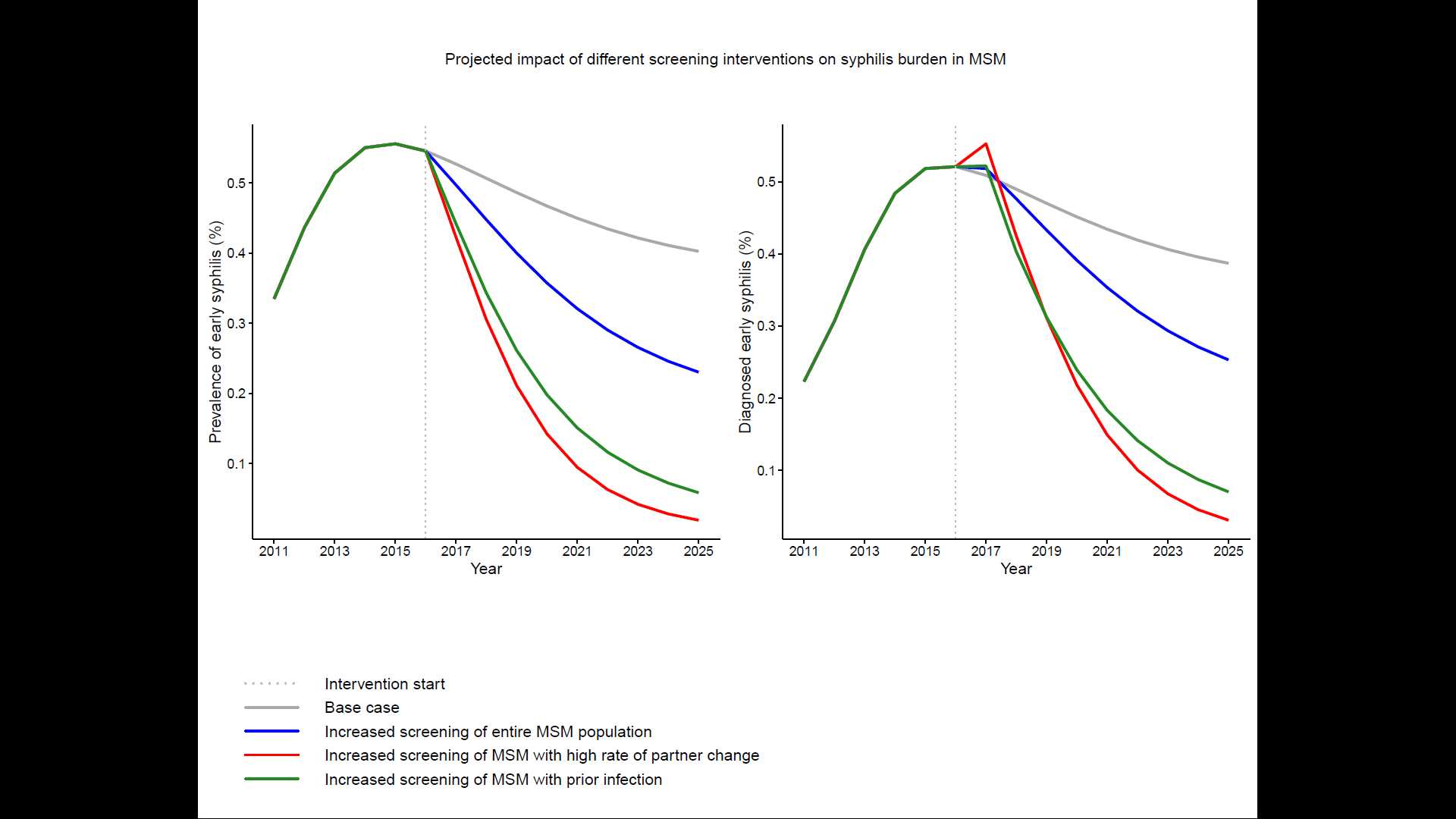
CAN ENHANCED SCREENING OF MEN WITH A HISTORY OF PRIOR SYPHILIS INFECTION STEM THE EPIDEMIC IN MEN WHO HAVE SEX WITH MEN? A MATHEMATICAL MODELING STUDY
Ashleigh Tuite, PhD, MPH1, Souradet Shaw, PhD2, Joss Reimer, MD, MPH2, Craig Ross, MA2, David Fisman, MD, MPH3 and Sharmistha Mishra, MD, PhD4
1Department of Global Health and Population, Harvard T.H. Chan School of Public Health, Boston, 2Winnipeg Regional Health Authority, Winnipeg, 3Dalla Lana School of Public Health, University of Toronto, Toronto, 4St Michael's Hospital, Toronto
Background: Syphilis re-infections comprise 5-50% of annual diagnoses across syphilis outbreaks in men who have sex with men (MSM) in Canada. We used mathematical modeling to evaluate if previous infection could be used as a marker of risk in a targeted screening intervention.
Methods: We parameterized a risk-stratified compartmental model of syphilis transmission in MSM to reflect the epidemiologic characteristics of an ongoing syphilis outbreak in Winnipeg. We evaluated the impact of screening 75% of men with a prior syphilis infection every 3 months, and compared this to distributing equivalent numbers of tests each year to all MSM or men with the highest rate of partner change. We estimated incident and diagnosed early syphilis cases averted over a 10-year time horizon and prevalence at the end of the intervention period, relative to a base case of 30% of MSM screened annually.
Results: In the base case, re-infections accounted for 16% of diagnosed infections within 10 years. Targeted screening of men with a prior infection was expected to avert 48% of incident infections, 40% of diagnosed cases, and reduce early syphilis prevalence at the end of the intervention period by 83%, relative to the base case. General screening was projected to have the least impact, while targeted screening in men with high rates of partner change was projected to be most effective (averting 55% of incident cases). When frequency of enhanced screening was reduced to semi-annually or annually, focusing on men prior infection was more effective than allocating tests to men with high rates of partner change.
Conclusions: Targeted screening in MSM with a prior syphilis infection is a readily actionable intervention and is expected to reduce infection burden in the population, especially when identification of high-risk men via self-reported partner change and high-frequency screening among high-risk men are difficult to achieve.
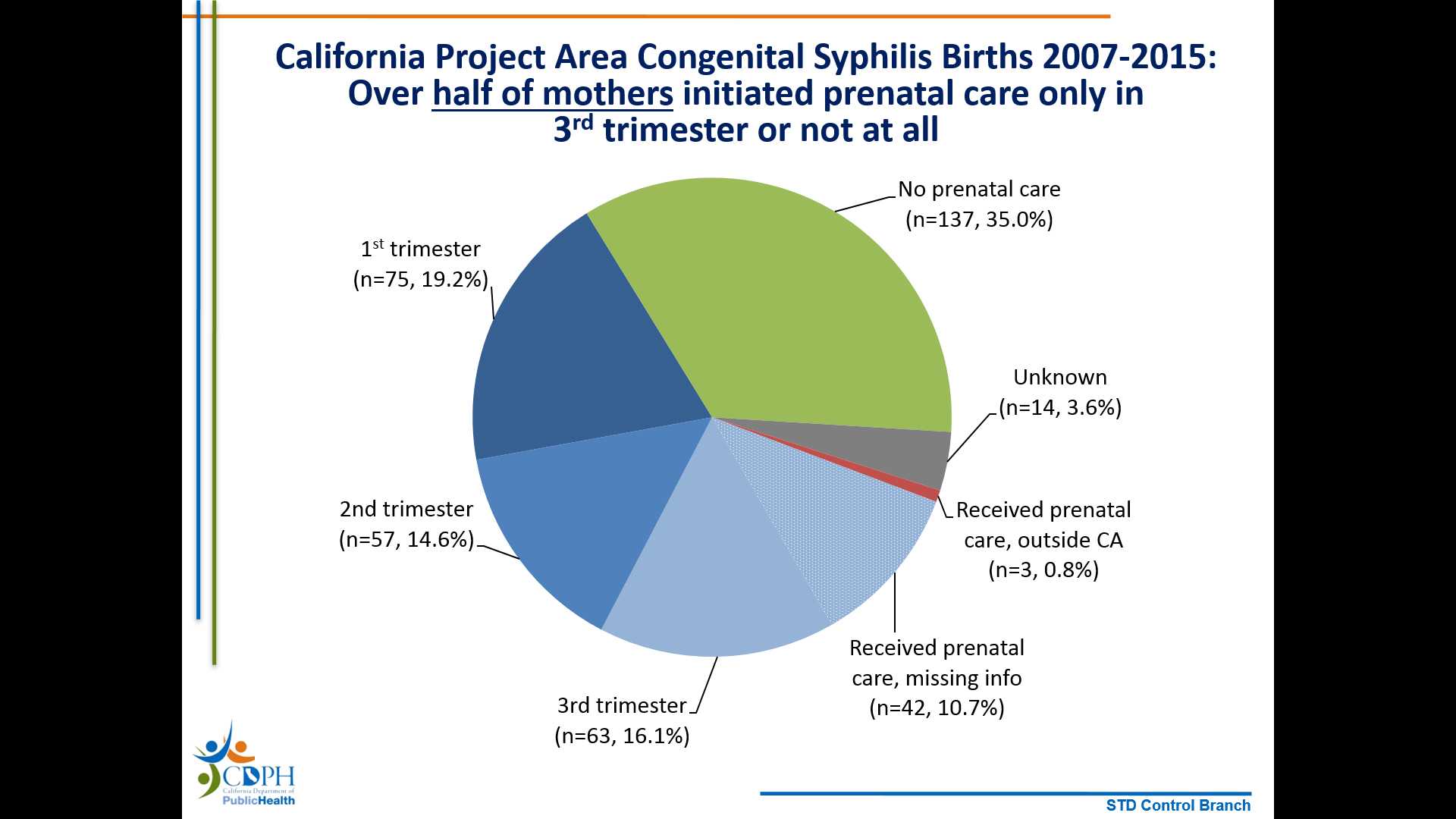
IDENTIFYING MISSED OPPORTUNITIES FOR PREVENTION: CONGENITAL SYPHILIS CASE REVIEW, CALIFORNIA PROJECT AREA, 2007-2015
Juliet E. Stoltey,1 Rilene C. Ng,1 Colleen Denny,2 Ina U. Park,1 Heidi M. Bauer1
1Sexually Transmitted Disease Control Branch, California Department of Public Health, Richmond, 2University of California, San Francisco, San Francisco
Background:
Between 2012 and 2015, congenital syphilis (CS) cases in California increased from 33 to 142. CS is of high public health importance because it can cause devastating outcomes and is preventable with proper treatment. We sought to characterize CS cases and identify missed opportunities for prevention.
Methods:
California law mandates syphilis reporting to local health departments (HD); cases are investigated and entered into the California Project Area (CPA, excluding Los Angeles and San Francisco) STD surveillance system. CS cases born 2007-2015 in the CPA were included based on the 2013 Centers for Disease Control and Prevention CS algorithm, and were matched to maternal syphilis cases. Infant characteristics, maternal demographics, prenatal care (PNC), clinical, and HD factors were examined.
Results:
From 2007-2015, 391 CS cases met criteria for analysis; there were 365 (93%) probable cases and 26 (7%) stillbirths. Most mothers with infants with CS had late syphilis (n=236, 60%), were age 20-29 (n=227, 58%), and were Hispanic (n=216, 55%). Only 75 (19%) women initiated PNC in the first trimester, 57 (15%) in second trimester, 63 (16%) in third trimester, and 137 (35%) had no PNC. Of 132 mothers who initiated PNC in 1st/2nd trimester, 104 (79%) were tested ≥30 days prior to delivery. Of those, 67 (64%) had reactive syphilis serology ≥30 days prior to delivery; treatment status was delayed/inadequate (n=31), none (n=11), unknown (n=7), and adequate (n=18). Of 132 mothers with early syphilis, 66 (50%) were interviewed within 14 days of assignment; 40 (30%) were not interviewed.
Conclusions:
Most mothers who gave birth to infants with CS had late syphilis and lacked timely PNC. Testing was frequently delayed/absent, treatment was frequently delayed/inadequate, and there were challenges in HD follow-up. CS prevention requires state and local collaboration to optimize surveillance systems, clinical services, disease investigation/partner services, communications, and partnerships.
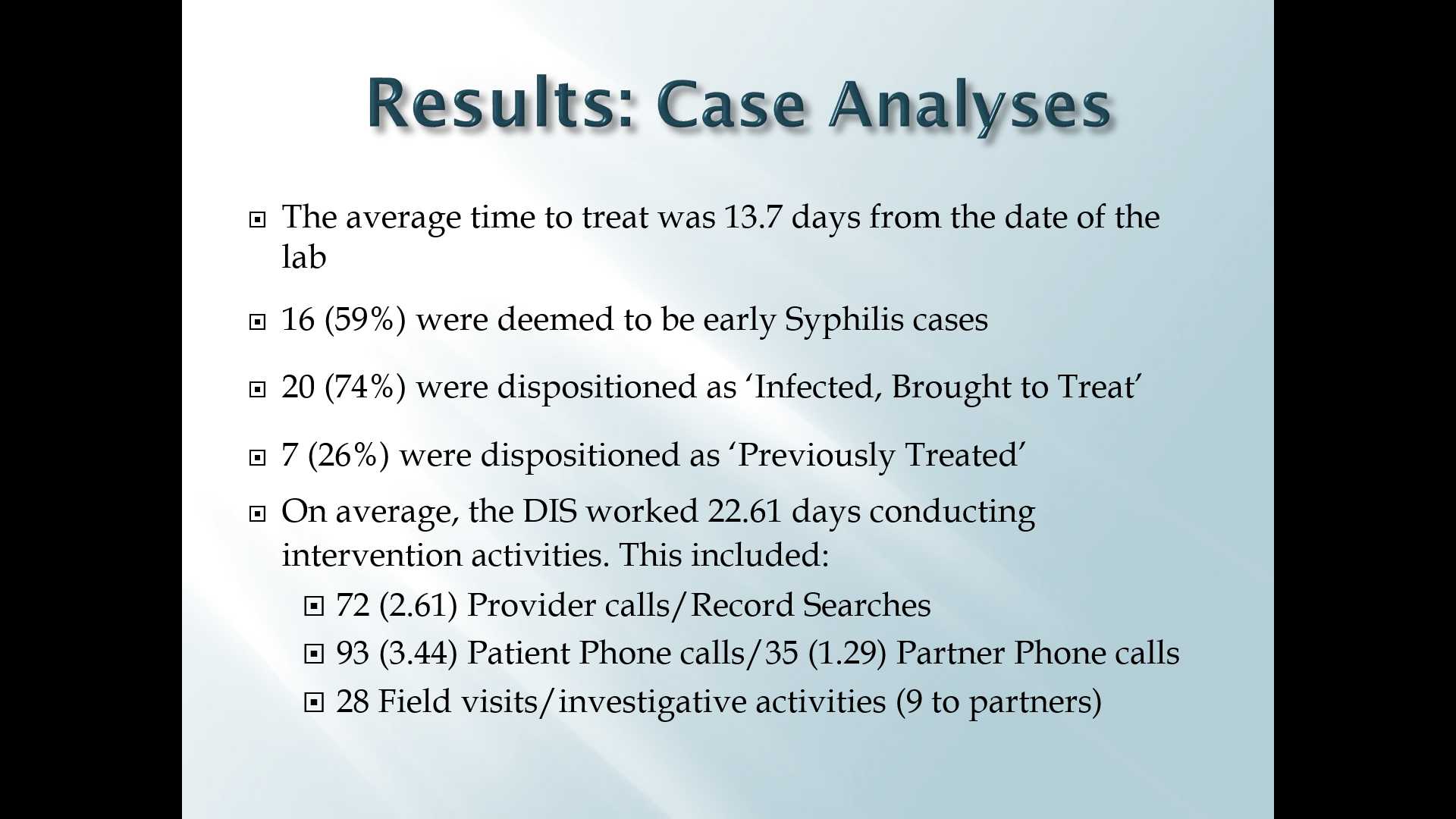
THE ROLE OF DISEASE INTERVENTION SPECIALISTS IN THE PREVENTION OF CONGENITAL SYPHILIS
Lavida Joseph Brown1, Justin Holderman1 Janet N. Arno MD1,2
1 Bell Flower Clinic, Health and Hospital Corporation of Marion County, Indianapolis, IN, 2Division of Infectious Diseases, Indiana University School of Medicine, Indianapolis, IN.
Background: According to the CDC, congenital syphilis rates increased by 38 percent between 2012 and 2014, from 334 to 458 cases. Indianapolis has had only 1 case of congenital syphilis from 2011 -2015 despite having the majority of syphilis morbidity in the state. We hypothesized that this was due to Disease Intervention Specialists (DIS) who played a major role in prevention.
Methods: All cases of pregnant women with positive non-treponemal tests reported by electronic laboratory reports and communicable disease reports from 2011-2015 were reviewed using data entered into the Indiana Statewide Investigating and Monitoring Surveillance System (SWIMSS) by DIS and surveillance personnel in the course of case investigations. Women with positive syphilis confirmatory tests identified as syphilis morbidity were further examined to determine their disposition and what DIS activity was done on each case.
Results: A total of forty-eight females were tested and found to have a positive non-treponemal test for syphilis during their pregnancy. Of these, 21 were found to be not infected because they had a negative treponemal confirmatory test or a previous history of treated syphilis leaving 27 pregnant women with syphilis of which 4 were secondary cases, 12 were early latent cases and 11 late latent cases by current definitions. Of these, DIS interviewed 23 of the 27 cases. 20 out of the 27 cases were infected and brought to treatment. Four others were treated prior to DIS contact.
Conclusions: DIS intensely followed up with each individual - making phone calls to providers and patients, conducting field investigative activities, and providing partner services. Some cases involved several hours of persistence in order to assure that these women and all of their partners were treated. Had it not been for DIS intervention, 74% of the women may not have been treated adequately in order to stop transmission to their infants underscoring the importance of DIS in congenital syphilis prevention.
- Page last reviewed: September 7, 2016 (archived document)
- Content source:


 ShareCompartir
ShareCompartir