AMD in Action: AMD Methods Map the Genetic Range of a Common Cause of Respiratory Illness
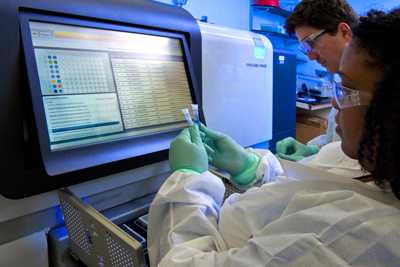
Pneumonia Response and Surveillance Laboratory staff prepare the RS PacBio II for whole genome sequencing.
CDC scientists are closing in on the genetic classification for one of the tiniest bacteria, Mycoplasma pneumoniae. Just as in human families, bacterial families can be closely related but have very different characteristics. When scientists map human genomes they can tell how people across generations are related. Similarly, using advanced molecular detection (AMD) to map bacterial genomes helps CDC understand the characteristics that allow bacteria to infect people or cause severe outbreaks of illness. By looking at and comparing bacterial DNA from closely related strains, scientists can develop better ways to more definitively identify bacteria. This will ideally result in better intervention strategies and more effective therapies, and possibly even lead to vaccines to protect people from getting sick.
Until now, scientists have had little understanding of the genetics of M. pneumoniae, which commonly causes “walking pneumonia.” Approximately 2 million people get sick from M. pneumoniae each year in the United States; most have minor symptoms, such as a sore throat. However, sometimes people develop serious, life-threatening complications such as lung infections (pneumonia) or swelling of the brain (encephalitis). The number of M. pneumoniae infections varies over time, with peaks of disease every 3 to 7 years. Researchers could not fully understand the complexity of M. pneumoniae infections because they knew little about the bacterium’s genetic information. Thanks to work performed through CDC’s AMD program, researchers have made significant progress in understanding the genetic elements of this bacterium that impact disease.
In 2016, researchers pulled 67 samples of M. pneumoniae from CDC’s bacterial strain archives. The samples were collected over decades from various parts of the world. Some samples came from people with mild illness and some from people who had died from their infection – and various ranges of illness in between. The researchers used multiple next generation sequencing methods to look at the bacterial genomes in these samples. Furthermore, researchers accessed genomic data on an additional 40 strains of M. pneumoniae from publicly available DNA databanks and included them in their analysis to generate the most comprehensive picture of this bacterium’s DNA to date.
Researchers found six distinct subtypes of M. pneumoniae that exist within two separate lineages, which each have three subtypes. Just as people have close and distant relatives, some of these bacterial types are more closely related to one another than others. The various genetic characteristics of M. pneumoniae may contribute to the reason why some people get sicker than others. This research has already resulted in the creation of a new diagnostic test that can quickly tell which type of M. pneumoniae someone has. This work will improve scientists’ understanding of this bacterium and the ability to identify new strains that might evolve in the future. Learning and understanding the genetics of this important respiratory pathogen is a critical step for improving public health and provides evidence-based data for developing and implementing effective ways to keep people healthy.
To learn more about this research, a comprehensive article is available online .
- Page last reviewed: April 26, 2017
- Page last updated: April 26, 2017
- Content source:
- Centers for Disease Control and Prevention
- Page maintained by: Office of Associate Director of Communication, Division of Public Affairs


 ShareCompartir
ShareCompartir