AMD Projects: Developing Faster Diagnostic Tests for Foodborne Bacteria
Exploring AMD methods for diagnosing gastrointestinal bacteria
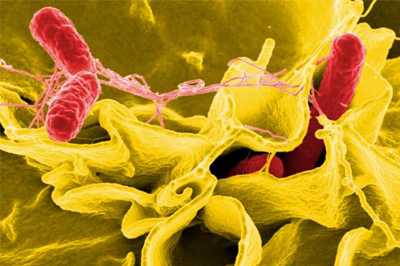
CDC is using AMD methods to develop new tests that can identify and characterize foodborne bacteria, such as Salmonella, directly from patient specimens without the need to culture the bacteria first.
CDC is racing to adapt its surveillance to rapidly changing technology in clinical diagnostic laboratories. Hospital and clinical laboratories are starting to use new DNA-based tests that can simultaneously test for multiple gastrointestinal pathogens, such as Salmonella and Shiga toxin-producing Escherichia coli (STEC). That’s great news for patients with foodborne illnesses because they will receive a diagnosis faster, but the news is mixed for public health investigators. The same technology that makes these new tests faster opens up new opportunities for public health, but also limits information provided to those who detect and investigate foodborne outbreaks.
The new diagnostic tests do not involve growth (“culture”) or isolation of the bacteria (“isolates”), steps that can add several days to testing. But bacterial isolates are the raw material of PulseNet, the national network of 82 laboratories that provides “DNA fingerprints” of disease-causing bacteria from ill patients to local, state, and federal health and regulatory agencies. Without isolates submitted to PulseNet, public health officials might lose the ability to match cases of illness, detect outbreaks, and identify the contaminated food sources that are making people sick.
This project will aggressively accelerate development of new tests to detect and characterize foodborne bacteria directly from patient specimens while providing usable data for PulseNet without the need for culture isolates. However, developing these types of tests is difficult because harmful bacteria targeted by PulseNet are genetically similar to bacteria normally found in the human intestinal tract. In addition, only a few of these bacteria might be present in the genetically complex environment of the human intestinal tract.
CDC investigators will explore multiple approaches to solving these problems, such as “targeted sequencing” (amplifying bits of the DNA of disease-causing bacteria and reading its genetic code without the need for culture) and “shotgun metagenomics” (reading the genetic code of all the DNA in the specimen). Researchers also will study various aspects of the stool micro-environment and look at microbial and human DNA found in the intestines of both healthy and sick people. As part of the development process, the project will collaborate with internal CDC partners working on similar problems, as well as clinical and public health laboratory partners. Advances made through this work will improve the nation’s ability to detect and stop foodborne outbreaks quickly.
2017 Project Update
In the project’s first year, researchers began collaborating with private- and public-sector partners to explore various laboratory techniques for extracting bacterial DNA directly from human stool specimens. The methods that were tested in CDC labs were rigorously evaluated for efficacy and safety. They designed a targeted sequencing method for STEC that is ready for initial laboratory testing and made progress on the development of computer software to automate the design of targeted sequencing methods for other bacteria, like Salmonella. Additionally, they have been evaluating bioinformatics software to sort sequencing data by species and strain of bacteria.
- Page last reviewed: March 27, 2017
- Page last updated: March 27, 2017
- Content source:


 ShareCompartir
ShareCompartir